
Synopsis
Synopsis
0
KDMF
0
NDC API
0
VMF
0
FDA Orange Book

DRUG PRODUCT COMPOSITIONS
0
US Patents
0
US Exclusivities
0
Health Canada Patents
0
Data Compilation #PharmaFlow
0
Stock Recap #PipelineProspector
0
Weekly News Recap #Phispers
1. Ardinex
2. Codeine Phosphate
3. Isocodeine
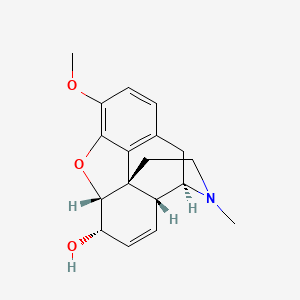
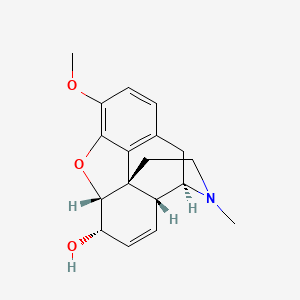
4. Morphinan-6-ol, 7,8-didehydro-4,5-epoxy-3-methoxy-17-methyl-, (5alpha,6alpha)-
5. N Methylmorphine
6. N-methylmorphine
1. Methylmorphine
2. Codeine Anhydrous
3. Codicept
4. Coducept
5. L-codeine
6. 76-57-3
7. Morphine Monomethyl Ether
8. O3-methylmorphine
9. Morphine 3-methyl Ether
10. (-)-codeine
11. Codeinum
12. Codeine Base
13. Morphine-3-methyl Ether
14. Codein
15. Norcodine, N-methyl
16. Norcodeine, N-methyl
17. Codeine Polistirex
18. Codeina
19. Ccris 7555
20. Hsdb 3043
21. Codeine (crm)
22. O(3)-methylmorphine
23. Chebi:16714
24. Ux6owy2v7j
25. Morphinan-6-ol, 7,8-didehydro-4,5-epoxy-3-methoxy-17-methyl-, (5alpha,6alpha)-
26. 7,8-didehydro-4,5-epoxy-3-methoxy-17-methylmorphinan-6-ol
27. Codeine Anhydrate
28. Ids-nc-005(sect.-2)
29. 7,8-didehydro-4,5alpha-epoxy-3-methoxy-17-methylmorphinan-6alpha-ol
30. (5alpha,6alpha)-7,8-didehydro-4,5-epoxy-3-methoxy-17-methylmorphinan-6-ol
31. Morphine-3-methyl Ester
32. Chembl369475
33. (5alpha,6alpha)-17-methyl-3-(methyloxy)-7,8-didehydro-4,5-epoxymorphinan-6-ol
34. (4r,4ar,7s,7ar,12bs)-9-methoxy-3-methyl-2,4,4a,7,7a,13-hexahydro-1h-4,12-methanobenzofuro[3,2-e]isoquinolin-7-ol
35. Codeine [inn:ban]
36. Einecs 200-969-1
37. Unii-ux6owy2v7j
38. Codeine Alkaloid
39. Codeine Usp
40. (codeine)
41. Morphinan-6-ol, 7,8-didehydro-4,5-epoxy-3-methoxy-17-methyl-, (5.alpha.,6.alpha.)-
42. 10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol(codeine)
43. 10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol[codeine]
44. Codeinum Monohydricum
45. Mytussin
46. Kodelak Fito
47. Codeine [hsdb]
48. Codeine [mi]
49. Dsstox_cid_341
50. Codeine [who-dd]
51. Morphinan-6alpha-ol, 7,8-didehydro-4,5alpha-epoxy-3-methoxy-17-methyl-
52. Chembl485
53. Epitope Id:120369
54. Codeine Polistirex [usan]
55. Schembl3257
56. Dsstox_rid_75524
57. Ss85u8k5zn
58. Dsstox_gsid_20341
59. Gtpl1673
60. Codeine 0.1 Mg/ml In Methanol
61. Codeine 1.0 Mg/ml In Methanol
62. Dtxsid2020341
63. (4r,4ar,7s,7ar,12bs)-9-methoxy-3-methyl-2,4,4a,7,7a,13-hexahydro-1h-4,12-methanobenzofuro[3,2-e]isoquinoline-7-ol
64. Zinc3806721
65. Tox21_200082
66. Bdbm50019351
67. Bdbm50105098
68. Akos015955539
69. Morphinan-6-alpha-ol, 7,8-didehydro-4,5-alpha-epoxy-3-methoxy-17-methyl-
70. Db00318
71. Cas-76-57-3
72. Morphinan-6-ol, 7,8-didehydro-4,5-epoxy-3-methoxy-17-methyl-, (5-alpha,6-alpha)-
73. Ncgc00248518-01
74. Ncgc00257636-01
75. Ac-11114
76. C06174
77. Morphine Sulfate Impurity A [ep Impurity]
78. Q174723
79. Codeine, European Pharmacopoeia (ep) Reference Standard
80. Dihydrocodeine Hydrogen Tartrate Impurity A [ep Impurity]
81. 3-methoxy-17-methyl-7,8-didehydro-4,5alpha-epoxymorphinan-6alpha-ol
82. Hydrocodone Hydrogen Tartrate 2.5-hydrate Impurity C [ep Impurity]
83. 7,8-didehydro-4,5.alpha.-epoxy-3-methoxy-17-methylmorphinan-6.alpha.-ol
84. Codeine Solution, 1 Mg/ml In Methanol, Ampule Of 1 Ml, Certified Reference Material
85. Codeine Solution, Analytical Standard, For Drug Analysis, 1.0 Mg/ml In Methanol
86. Morphinan-6-ol, 7,8-didehydro-4,5-epoxy-3-methoxy-17-methyl-, (5alpha,6alpha)- (9ci)
87. Morphinan-6alpha-ol, 7,8-didehydro-4,5alpha-epoxy-3-methoxy-17-methyl- (8ci)
88. (1s,13r,14s,17r)-10-methoxy-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0(1,13).0(5,17).0(7,18)]octadeca-7(18),8,10,15-tetraen-14-ol
89. (1s,5r,13r,14s,17r)-10-methoxy-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0?,??.0?,??.0?,??]octadeca-7,9,11(18),15-tetraen-14-ol
90. (1s,5r,13r,14s,17r)-10-methoxy-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0^{1,13}.0^{5,17}.0^{7,18}]octadeca-7(18),8,10,15-tetraen-14-ol
91. (1s,5r,13r,14s,17r)-10-methoxy-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0^{1,13}.0^{5,17}.0^{7,18}]octadeca-7,9,11(18),15-tetraen-14-ol
92. (codeine)10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol
93. 10-methoxy-4-methyl-(13r,14s)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10-trien-14-ol(dihydrocodeine)
94. 10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol
95. 10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol Phosphate(codeine)
96. 10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol(codeine (h3po4))
97. 10-methoxy-4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraen-14-ol(codeine Phosphate)
| Molecular Weight | 299.4 g/mol |
|---|---|
| Molecular Formula | C18H21NO3 |
| XLogP3 | 1.1 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 1 |
| Exact Mass | 299.15214353 g/mol |
| Monoisotopic Mass | 299.15214353 g/mol |
| Topological Polar Surface Area | 41.9 Ų |
| Heavy Atom Count | 22 |
| Formal Charge | 0 |
| Complexity | 509 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 5 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Analgesics, Opioid; Antitussive Agents; Narcotics
National Library of Medicine's Medical Subject Headings. Codeine. Online file (MeSH, 2016). Available from, as of August 12, 2016: https://www.nlm.nih.gov/mesh/2016/mesh_browser/MBrowser.html
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Codeine is included in the database.
NIH/NLM; ClinicalTrials.Gov. Available from, as of March 17, 2016: https://clinicaltrials.gov/ct2/results?term=codeine&Search=Search
(VET): Codeine, or codeine with acetaminophen, is indicated for treatment of moderate pain. It also has been used as an antitussive.
Papich, M.G. Saunders Handbook of Veterinary Drugs Small and Large Animal. 3rd ed. St. Louis, MO: Elsevier Saunders, 2011, p. 176
CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016; This guideline provides recommendations for primary care clinicians who are prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. The guideline addresses 1) when to initiate or continue opioids for chronic pain; 2) opioid selection, dosage, duration, follow-up, and discontinuation; and 3) assessing risk and addressing harms of opioid use. CDC developed the guideline using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework, and recommendations are made on the basis of a systematic review of the scientific evidence while considering benefits and harms, values and preferences, and resource allocation. CDC obtained input from experts, stakeholders, the public, peer reviewers, and a federally chartered advisory committee. It is important that patients receive appropriate pain treatment with careful consideration of the benefits and risks of treatment options. This guideline is intended to improve communication between clinicians and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder, overdose, and death.
Dowell D et al; Morbidity and Mortality Weekly Report (MMWR) 65 (1):1-49 (2016); Available from, as of March 22, 2016: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm
For more Therapeutic Uses (Complete) data for CODEINE (11 total), please visit the HSDB record page.
The U.S. Food and Drug Administration (FDA) is warning about several safety issues with the entire class of opioid pain medicines. These safety risks are potentially harmful interactions with numerous other medications, problems with the adrenal glands, and decreased sex hormone levels. We are requiring changes to the labels of all opioid drugs to warn about these risks. Opioids can interact with antidepressants and migraine medicines to cause a serious central nervous system reaction called serotonin syndrome, in which high levels of the chemical serotonin build up in the brain and cause toxicity. Taking opioids may lead to a rare, but serious condition in which the adrenal glands do not produce adequate amounts of the hormone cortisol. Cortisol helps the body respond to stress. Long-term use of opioids may be associated with decreased sex hormone levels and symptoms such as reduced interest in sex, impotence, or infertility.
FDA; FDA Drug Safety Communication: FDA Warns About Several Safety Issues with Opioid Pain Medicines; Requires Label Changes (March 22, 2016). Available from, as of March 22, 2016: https://www.fda.gov/Drugs/DrugSafety/ucm489676.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery
In a continuing effort to educate prescribers and patients about the potential risks related to opioid use, the U.S. Food and Drug Administration today announced required class-wide safety labeling changes for immediate-release (IR) opioid pain medications. Among the changes, the FDA is requiring a new boxed warning about the serious risks of misuse, abuse, addiction, overdose and death. Today's actions are among a number of steps the agency recently outlined in a plan to reassess its approach to opioid medications. The plan is focused on policies aimed at reversing the epidemic, while still providing patients in pain access to effective relief.
FDA; FDA News Release: FDA Announces Enhanced Warnings for Immediate-Release Opioid Pain Medications Related to Risks of Misuse, Abuse, Addiction, Overdose and Death (March 22, 2016). Available from, as of March 22, 2016 https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm491739.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery
Codeine should be used with caution in nursing women who are known or suspected ultrarapid metabolizers of cytochrome P-450 (CYP) 2D6 substrates.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2205
Children with obstructive sleep apnea receiving codeine for the management of postoperative pain following tonsillectomy and/or adenoidectomy, who also have evidence of ultrarapid metabolism of CYP2D6 substrates, are at increased risk of respiratory depression.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2205
For more Drug Warnings (Complete) data for CODEINE (12 total), please visit the HSDB record page.
In adults, ingestion of 7 to 14 mg/kg may cause death. Much higher doses may be tolerated by chronic users. Ingestion of more than 1 mg/kg of codeine in children is capable of producing symptoms, and doses more than 5 mg/kg have caused respiratory arrest.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 761
The lethal dose is between 500 mg and 1 g.
Gossel, T.A., J.D. Bricker. Principles of Clinical Toxicology. 3rd ed. New York, NY: Raven Press, Ltd., 1994., p. 298
Toxic codeine blood concentration: 20-50 ug/dL; Lethal codeine blood concentration: > 60 ug/dL /From table/
Gossel, T.A., J.D. Bricker. Principles of Clinical Toxicology. 3rd ed. New York, NY: Raven Press, Ltd., 1994., p. 298
Codeine sulfate is a form of this drug that is commonly used. It is available in tablet form and indicated for the relief of mild to moderately severe pain, where the use of an opioid analgesic is appropriate. The solution form is used by itself or combined in a syrup with other drugs and is used as a cough suppressant in adults aged 18 and above,.
FDA Label
**General effects** Codeine is a weak narcotic pain reliever and cough suppressant that is similar to morphine and hydrocodone. A small amount of ingested codeine is converted to morphine in the body. Codeine increases tolerance to pain, reducing existing discomfort. In addition to decreasing pain, codeine also causes sedation, drowsiness, and respiratory depression. **Antitussive activity** This drug has shown antitussive activity in clinical trials and has been effective in cough secondary to tuberculosis and insomnia due to coughing. Codeine suppresses the cough reflex through a direct effect on the cough center in the medulla. **Effects on intestinal motility** Codeine may reduce intestinal motility through both a local and possibly central mechanism of action. This may possibly lead to constipation. The chronic use of opioids, including codeine sulfate, may lead to obstructive bowel disease, particularly in patients with underlying disorders of intestinal motility. **Effects on the central nervous system** Codeine phosphate is an opioid analgesic with uses similar to those of morphine, but is much less potent as an analgesic. Its primary site of action is at the _mu_ opioid receptors distributed throughout the central nervous system. The sedative activities of codeine are less potent than those of morphine. Codeine may cause respiratory system depression by the activation of -opioid receptors at specific sites in the central nervous system. **Effects on blood pressure** This drug poses an increased risk of compromised ability to maintain blood pressure due to peripheral vasodilation and other mechanisms. **Effects on chronic cancer pain and other types of pain** Codeine is an opioid analgesic with similar indications to those of morphine, however, is much less potent in its pain alleviating properties. Its primary action takes place at the mu opioid receptors, which are distributed throughout the central nervous system. The average duration of action is about 4 hours. Regular dosing of opioid analgesics such as codeine in patients with severe cancer pain has been well documented to improve symptoms,.
Analgesics, Opioid
Compounds with activity like OPIATE ALKALOIDS, acting at OPIOID RECEPTORS. Properties include induction of ANALGESIA or NARCOSIS. (See all compounds classified as Analgesics, Opioid.)
Antitussive Agents
Agents that suppress cough. They act centrally on the medullary cough center. EXPECTORANTS, also used in the treatment of cough, act locally. (See all compounds classified as Antitussive Agents.)
Narcotics
Agents that induce NARCOSIS. Narcotics include agents that cause somnolence or induced sleep (STUPOR); natural or synthetic derivatives of OPIUM or MORPHINE or any substance that has such effects. They are potent inducers of ANALGESIA and OPIOID-RELATED DISORDERS. (See all compounds classified as Narcotics.)
R05DA04
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
R - Respiratory system
R05 - Cough and cold preparations
R05D - Cough suppressants, excl. combinations with expectorants
R05DA - Opium alkaloids and derivatives
R05DA04 - Codeine
Absorption
**Absorption** Codeine is absorbed from the gastrointestinal tract. The maximum plasma concentration occurs 60 minutes after administration. **Food Effects** When 60 mg codeine sulfate was given 30 minutes post-ingestion of a high high-calorie meal, there was no significant change in the absorption of codeine. **Steady-state concentration** The administration of 15 mg codeine sulfate every 4 hours for 5 days lead to steady-state concentrations of codeine, morphine, morphine-3-glucuronide (M3G) and morphine-6-glucuronide (M6G) within 48 hours.
Route of Elimination
About 90% of the total dose of codeine is excreted by the kidneys. Approximately 10% of the drug excreted by the kidneys is unchanged codeine. The majority of the excretion products can be found in the urine within 6 hours of ingestion, and 40-60 % of the codeine is excreted free or conjugated, approximately 5 to 15 percent as free and conjugated morphine, and approximately 10-20% free and conjugated norcodeine.
Volume of Distribution
Apparent volume of distribution: about 3-6 L/kg, showing an extensive distribution of the drug into tissues.
Clearance
Renal clearance of codeine was 183 +/- 59 ml min-1 in a clinical study. Renal impairment may decrease codeine clearance [LABEL].
Oral absorption of codeine is good, but there is a significant first-pass effect. The Vd is 2.6 L/kg, and there is a minimal protein binding. The onset os analgesic effect is 30 to 60 minutes, and antitussive effect is 1 to 2 hours. Peak effect is reached in 2 to 4 hours. ... Between 3% and 16% is excreted unchanged in the urine, and 90% of the absorbed dose if excreted via the kidney.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 761
Postmortem samples from 14 cases of suspected heroin overdose were subjected to a preliminary systematic toxicological analysis in order to highlight the presence of unknown exogenous compounds (e.g., drugs of abuse, alcohol) that may have played a role in the mechanism of death. This analysis unveiled histories of poly-drug use in seven of the cases under investigation. Moreover, the concentrations of morphine and codeine in the brain were also investigated, and the results were compared with the data obtained from the blood specimens. The concentration of morphine in blood ranged from 33 to 688 ng/mL, while the concentration of codeine ranged from 0 to 193 ng/mL. However, in the brain, the concentration of morphine was found to be between 85 and 396 ng/g, while the levels of codeine ranged from 11 to 160 ng/g. The codeine/morphine ratio in the blood ranged from 0.043 to 0.619; however, in the brain, the same ratio was found to be between 0.129 and 0.552. In most cases, a significantly higher codeine/morphine ratio was found in the brain, suggesting the accumulation of codeine in brain tissue due its high lipophilicity as compared with morphine.
PMID:24727081 Gambaro V et al; J Anal Toxicol 38 (5): 289-94 (2014)
Opiates are an important component for drug testing due to their high abuse potential. Proper urine opiate interpretation includes ruling out poppy seed ingestion; however, detailed elimination studies after controlled poppy seed administration with known morphine and codeine doses are not available. Therefore, we investigated urine opiate pharmacokinetics after controlled oral administration of uncooked poppy seeds with known morphine and codeine content. Participants were administered two 45 g oral poppy seed doses 8 hr apart, each containing 15.7 mg morphine and 3 mg codeine. Urine was collected ad libitum up to 32 hr after the first dose. Specimens were analyzed with the Roche Opiates II immunoassay at 2000 and 300 ug/L cutoffs, and the ThermoFisher CEDIA heroin metabolite (6-acetylmorphine, 6-AM) and Lin-Zhi 6-AM immunoassays with 10 ug/L cutoffs to determine if poppy seed ingestion could produce positive results in these heroin marker assays. In addition, all specimens were quantified for morphine and codeine by GC/MS. Participants (N=22) provided 391 urine specimens over 32 hr following dosing; 26.6% and 83.4% were positive for morphine at 2000 and 300 ug/L GC/MS cutoffs, respectively. For the 19 subjects who completed the study, morphine concentrations ranged from <300 to 7522 ug/L with a median peak concentration of 5239 ug/L. The median first morphine-positive urine sample at 2000 ug/L cutoff concentration occurred at 6.6 hr (1.2-12.1), with the last positive from 2.6 to 18 hr after the second dose. No specimens were positive for codeine at a cutoff concentration of 2000 ug/L, but 20.2% exceeded 300 ug/L, with peak concentrations of 658 ug/L (284-1540). The Roche Opiates II immunoassay had efficiencies greater than 96% for the 2000 and 300 ug/L cutoffs. The CEDIA 6-AM immunoassay had a specificity of 91%, while the Lin-Zhi assay had no false positive results. These data provide valuable information for interpreting urine opiate results.
PMID:24887324 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127332 Smith ML et al; Forensic Sci Int 241: 87-90 (2014)
Opiates are an important drug class in drug testing programs. Ingestion of poppy seeds containing morphine and codeine can yield positive opiate tests and mislead result interpretation in forensic and clinical settings. Multiple publications evaluated urine opiate concentrations following poppy seed ingestion, but only two addressed oral fluid (OF) results; neither provided the ingested morphine and codeine dosage. We administered two 45 g raw poppy seed doses, each containing 15.7 mg morphine and 3.1 mg codeine, 8 hr apart to 17 healthy adults. All OF specimens were screened by on-site OF immunoassay Draeger DrugTest 5000, and confirmed with OF collected with Oral-Eze device and quantified by liquid chromatography-tandem mass spectrometry (1 ug/L morphine and codeine limits of quantification). Specimens (n=459) were collected before and up to 32 hr after the first dose. All specimens screened positive 0.5 hr after dosing and remained positive for 0.5-13 hr at Draeger 20 ug/L morphine cut-off. Maximum OF morphine and codeine concentrations (Cmax) were 177 and 32.6 ug/L, with times to Cmax (Tmax) of 0.5-1 hr and 0.5-2.5 hr post-dose, respectively. Windows of detection after the second dose extended at least 24 hr for morphine and to 18 hr for codeine. After both doses, the last morphine positive OF result was 1 hr with 40 ug/L 2004 proposed US Substance Abuse and Mental Health Services Administration cut-off, and 0.5 hr with 95 ug/L cut-off, recently recommended by the Driving under the Influence of Drugs and Medicines project. Positive OF morphine results are possible 0.5-1 hr after ingestion of 15.7 mg of morphine in raw poppy seeds, depending on the cut-off employed.
PMID:25345619 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4409445 Concheiro M et al; Drug Test Anal 7 (7): 586-91 (2015)
For more Absorption, Distribution and Excretion (Complete) data for CODEINE (7 total), please visit the HSDB record page.
Approximately 70 to 80% of the ingested dose of codeine is metabolized in the liver by conjugation with glucuronic acid to _codeine-6 glucuronide_ (C6G) and by O-demethylation to _morphine_ (about 5-10%) and N-demethylation to _norcodeine_ (about 10%) respectively. UDP-glucuronosyltransferase (UGT) 2B7 and 2B4 are the major metabolic enzymes mediating the glucurodination of codeine to the metabolite, _codeine 6 glucuronide_. Cytochrome P450 2D6 is the major enzyme responsible for the transformation of codeine to morphine and P450 3A4 is the main enzyme mediating the conversion of codeine to _norcodeine_. Morphine and norcodeine are then further metabolized by conjugation with glucuronic acid. The glucuronide metabolites of morphine are _morphine-3-glucuronide_ (M3G) and_ morphine-6-glucuronide _(M6G). Morphine and M6G have been proven to have analgesic activity in humans. The analgesic activity of C6G in humans is not known at this time. Norcodeine and M3G are generally not considered to have analgesic properties.
Codeine is metabolized in the liver by glucuronidation to codeine-6-glucuronide, by O-demethylation to morphine via CYP2D6, and by N-demethylation to norcodeine via CYP3A, all active metabolites. There is genetic polymorphism od CYP2D6. .. Poor /CYP2D6/ metabolizers have decreased analgesic effectiveness by inhibiting conversion of codeine to morphine. Concomitant administration with CYP2D6 inducers may result in increased metabolism and clearance of drug and also produce decreased clinical efficacy. Examples of CYP2D6 inducers include dexamethasone and rifampin.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 761
... Results confirm biotransformation of codeine to ... normorphine in rodents.
The Chemical Society. Foreign Compound Metabolism in Mammals. Volume 2: A Review of the Literature Published Between 1970 and 1971. London: The Chemical Society, 1972., p. 190
Cytochrome P450 2D6 (CYP2D6) is a member of the cytochrome P450 (CYP) superfamily involved in the biotransformation of drugs and substances of abuse encountered in clinical toxicology. Among the CYP superfamily, the CYP2D6 gene is considered as the most polymorphic as more than 105 different alleles have been identified so far. CYP2D6 genetic polymorphisms have the potential to affect the toxicity of their substrates. This review will focus specifically on CYP2D6 genetic polymorphisms and their relevance for poisoning due to amphetamines, opioid analgesics and antidepressants in humans. PubMed (up to August 2013) was searched with the following selection criteria: 'CYP2D6 AND (toxicology OR poisoning OR intoxication OR overdose)'. Of the 454 citations retrieved, only 46 papers dealt with the impact of CYP2D6 polymorphisms on poisoning due to amphetamines, opioid analgesics and antidepressants. ... Opioid analgesics. CYP2D6 ultra-rapid metabolizers are more likely to experience the adverse effects of codeine and tramadol. Opioid analgesics that do not rely on CYP2D6 for therapeutic activity, such as morphine and hydromorphone, may therefore be a better alternative to codeine and tramadol, with the limitation that these drugs have their own set of adverse reactions. ... Either poor or extensive/ultra-rapid CYP2D6 metabolizers may be exposed to toxic effects of amphetamines, opioid analgesics and antidepressants. In these three categories, the level of evidence is substance dependent, with differences within the same pharmacological class.
PMID:25998998 Haufroid V, Hantson P; Clin Toxicol (Phila) 53 (6): 501-10 (2015)
Opioid analgesics are commonly prescribed for acute and chronic pain, but are subject to abuse. Consequently, toxicology testing programs are frequently implemented for both forensic and clinical applications. Understanding opioid metabolism and disposition is essential for assessing risk of toxicity and, in some cases, providing additional information regarding risk of therapeutic failure. Opioids significantly metabolized by the cytochromeP450 (CYP450) enzyme system maybe subject to drug-drug interactions, including codeine, hydrocodone, oxycodone, fentanyl, meperidine, methadone, buprenorphine, and tramadol. CYP2D6 metabolism is polymorphic, and pharmacogenetic testing has been investigated for codeine, tramadol, oxycodone, and hydrocodone. CYP2B6 pharmacogenetic testing of methadone may reduce the risk of cardiac toxicity associated with the S-enantiomer. Opioids metabolized primarily by uridine 5'-diphospho-glucuronsyltransferase (UGT) enzymes include morphine, hydromorphone, dihydrocodeine, oxymorphone, levorphanol, and tapentadol. Parent and metabolite disposition is described for blood, oral fluid, and urine. Parent drug is most commonly detected in blood and oral fluid, whereas metabolites typically predominate in urine. Oral fluid/blood ratios exceed 1 for most opioids, making this an excellent alternative matrix for testing of this drug class. Metabolites of codeine, hydrocodone, and oxycodone are commercially available, and knowledge of metabolism is necessary for correct interpretation.
PMID:26227254 DePriest AZ et al; Forensic Sci Rev 27 (2): 115-45 (2015)
For more Metabolism/Metabolites (Complete) data for CODEINE (7 total), please visit the HSDB record page.
Codeine has known human metabolites that include (2S,3S,4S,5R)-6-[[(4R,4Ar,7S,7aR,12bS)-9-methoxy-3-methyl-2,4,4a,7,7a,13-hexahydro-1H-4,12-methanobenzofuro[3,2-e]isoquinolin-7-yl]oxy]-3,4,5-trihydroxyoxane-2-carboxylic acid, morphine, and norcodeine.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
Plasma half-lives of codeine and its metabolites have been reported to be approximately 3 hours.
Radioimmunoassay (RIA) was used to determine several pharmacokinetic parameters of codeine in man, including the relative bioavailability after oral and intramuscular administration. The study followed a crossover design in 6 healthy, young (18 to 21 yr), male volunteers. Three subjects received 65 mg codeine phosphate orally in an analgesic mixture which also contained aspirin, phenacetin, and caffeine. At the same time a similar group received an equivalent dose of codeine phosphate in a single intramuscular injection. Two weeks later the study was repeated so that each group received the alternate treatment. Plasma samples were collected at various times after drug administration, and codeine concentrations were determined by a specific RIA procedure. The procedure can detect less than 50 pg of codeine. Following intramuscular administration, peak plasma concentrations (194 to 340 ng/ml) were observed between 0.25 to 1 hr; after oral dosing, peak codeine plasma concentrations (102 to 140 ng/ml) appeared within 0.75 to 1 hr. The mean plasma t1/2 and volume of distribution of codeine following intramuscular injection were 3.32 hr and 5.1 L/kg, respectively. Oral, relative to intramuscular, bioavailability of codeine, based on areas under the codeine plasma curves, was 42% to 71% (mean, 53%).
PMID:902456 Findlay JW et al; Clin Pharmacol Ther 22 (10): 439-46 (1977)
Assuming a rate of hair growth of 1 cm/month, the mean hair elimination half-life of /codeine was 0.61 months (95% CI, 0.54-0.69)/ ... .
PMID:23165127 Shen M et al; Forensic Sci Int 227 (1-3): 64-8 (2013)
The elimination half-life of codeine is 2.5 to 3.5 hours with a clinical duration of 4 to 8 hours because of active metabolites.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 761
Codeine is metabolized rapidly by the tissues of humans, dogs, & rats. Metabolic alteration followed by rapid urinary excretion begins a few minutes after im injection & after a slight delay following oral admin. About one-half an ordinary dose is eliminated within 6 hr & all within 24 hr.
Booth, N.H., L.E. McDonald (eds.). Veterinary Pharmacology and Therapeutics. 5th ed. Ames, Iowa: Iowa State University Press, 1982., p. 284
Codeine is a selective agonist for the mu opioid receptor, but with a much weaker affinity to this receptor than morphine, a more potent opioid drug. Codeine binds to mu-opioid receptors, which are involved in the transmission of pain throughout the body and central nervous system,. The analgesic properties of codeine are thought to arise from its conversion to [Morphine], although the exact mechanism of analgesic action is unknown at this time,.
Codeine causes suppression of the cough reflex by a direct effect on the cough center in the medulla of the brain and appears to exert a drying effect on respiratory tract mucosa and to increase viscosity of bronchial secretions.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2869

API/FDF Prices: Book a Demo to explore the features and consider upgrading later
API Imports and Exports
| Importing Country | Total Quantity (KGS) |
Average Price (USD/KGS) |
Number of Transactions |
|---|
Upgrade, download data, analyse, strategize, subscribe with us
Related Excipient Companies

Excipients by Applications
Global Sales Information

Market Place

REF. STANDARDS & IMPURITIES

ANALYTICAL

ABOUT THIS PAGE
71
PharmaCompass offers a list of Codeine API manufacturers, exporters & distributors, which can be sorted by GMP, USDMF, JDMF, KDMF, CEP (COS), WC, Price,and more, enabling you to easily find the right Codeine manufacturer or Codeine supplier for your needs.
Send us enquiries for free, and we will assist you in establishing a direct connection with your preferred Codeine manufacturer or Codeine supplier.
PharmaCompass also assists you with knowing the Codeine API Price utilized in the formulation of products. Codeine API Price is not always fixed or binding as the Codeine Price is obtained through a variety of data sources. The Codeine Price can also vary due to multiple factors, including market conditions, regulatory modifications, or negotiated pricing deals.
A Codeine polistirex manufacturer is defined as any person or entity involved in the manufacture, preparation, processing, compounding or propagation of Codeine polistirex, including repackagers and relabelers. The FDA regulates Codeine polistirex manufacturers to ensure that their products comply with relevant laws and regulations and are safe and effective to use. Codeine polistirex API Manufacturers are required to adhere to Good Manufacturing Practices (GMP) to ensure that their products are consistently manufactured to meet established quality criteria.
click here to find a list of Codeine polistirex manufacturers with USDMF, JDMF, KDMF, CEP, GMP, COA and API Price related information on PhamaCompass.
A Codeine polistirex supplier is an individual or a company that provides Codeine polistirex active pharmaceutical ingredient (API) or Codeine polistirex finished formulations upon request. The Codeine polistirex suppliers may include Codeine polistirex API manufacturers, exporters, distributors and traders.
click here to find a list of Codeine polistirex suppliers with USDMF, JDMF, KDMF, CEP, GMP, COA and API Price related information on PharmaCompass.
A Codeine polistirex DMF (Drug Master File) is a document detailing the whole manufacturing process of Codeine polistirex active pharmaceutical ingredient (API) in detail. Different forms of Codeine polistirex DMFs exist exist since differing nations have different regulations, such as Codeine polistirex USDMF, ASMF (EDMF), JDMF, CDMF, etc.
A Codeine polistirex DMF submitted to regulatory agencies in the US is known as a USDMF. Codeine polistirex USDMF includes data on Codeine polistirex's chemical properties, information on the facilities and procedures used, and details about packaging and storage. The Codeine polistirex USDMF is kept confidential to protect the manufacturer’s intellectual property.
click here to find a list of Codeine polistirex suppliers with USDMF on PharmaCompass.
The Pharmaceuticals and Medical Devices Agency (PMDA) established the Japan Drug Master File (JDMF), also known as the Master File (MF), to permit Japanese and foreign manufacturers of drug substances, intermediates, excipients, raw materials, and packaging materials (‘Products’) to voluntarily register confidential information about the production and management of their products in Japan.
The Codeine polistirex Drug Master File in Japan (Codeine polistirex JDMF) empowers Codeine polistirex API manufacturers to present comprehensive information (e.g., production methods, data, etc.) to the review authority, i.e., PMDA (Pharmaceuticals & Medical Devices Agency).
PMDA reviews the Codeine polistirex JDMF during the approval evaluation for pharmaceutical products. At the time of Codeine polistirex JDMF registration, PMDA checks if the format is accurate, if the necessary items have been included (application), and if data has been attached.
click here to find a list of Codeine polistirex suppliers with JDMF on PharmaCompass.
A Codeine polistirex CEP of the European Pharmacopoeia monograph is often referred to as a Codeine polistirex Certificate of Suitability (COS). The purpose of a Codeine polistirex CEP is to show that the European Pharmacopoeia monograph adequately controls the purity of Codeine polistirex EP produced by a given manufacturer. Suppliers of raw materials can prove the suitability of Codeine polistirex to their clients by showing that a Codeine polistirex CEP has been issued for it. The manufacturer submits a Codeine polistirex CEP (COS) as part of the market authorization procedure, and it takes on the role of a Codeine polistirex CEP holder for the record. Additionally, the data presented in the Codeine polistirex CEP (COS) is managed confidentially and offers a centralized system acknowledged by numerous nations, exactly like the Codeine polistirex DMF.
A Codeine polistirex CEP (COS) is recognised by all 36 nations that make up the European Pharmacopoeia Convention. Codeine polistirex CEPs may be accepted in nations that are not members of the Ph. Eur. at the discretion of the authorities there.
click here to find a list of Codeine polistirex suppliers with CEP (COS) on PharmaCompass.
A Codeine polistirex written confirmation (Codeine polistirex WC) is an official document issued by a regulatory agency to a Codeine polistirex manufacturer, verifying that the manufacturing facility of a Codeine polistirex active pharmaceutical ingredient (API) adheres to the Good Manufacturing Practices (GMP) regulations of the importing country. When exporting Codeine polistirex APIs or Codeine polistirex finished pharmaceutical products to another nation, regulatory agencies frequently require a Codeine polistirex WC (written confirmation) as part of the regulatory process.
click here to find a list of Codeine polistirex suppliers with Written Confirmation (WC) on PharmaCompass.
Codeine polistirex Active pharmaceutical ingredient (API) is produced in GMP-certified manufacturing facility.
GMP stands for Good Manufacturing Practices, which is a system used in the pharmaceutical industry to make sure that goods are regularly produced and monitored in accordance with quality standards. The FDA’s current Good Manufacturing Practices requirements are referred to as cGMP or current GMP which indicates that the company follows the most recent GMP specifications. The World Health Organization (WHO) has its own set of GMP guidelines, called the WHO GMP. Different countries can also set their own guidelines for GMP like China (Chinese GMP) or the EU (EU GMP).
PharmaCompass offers a list of Codeine polistirex GMP manufacturers, exporters & distributors, which can be sorted by USDMF, JDMF, KDMF, CEP (COS), WC, API price, and more, enabling you to easily find the right Codeine polistirex GMP manufacturer or Codeine polistirex GMP API supplier for your needs.
A Codeine polistirex CoA (Certificate of Analysis) is a formal document that attests to Codeine polistirex's compliance with Codeine polistirex specifications and serves as a tool for batch-level quality control.
Codeine polistirex CoA mostly includes findings from lab analyses of a specific batch. For each Codeine polistirex CoA document that a company creates, the USFDA specifies specific requirements, such as supplier information, material identification, transportation data, evidence of conformity and signature data.
Codeine polistirex may be tested according to a variety of international standards, such as European Pharmacopoeia (Codeine polistirex EP), Codeine polistirex JP (Japanese Pharmacopeia) and the US Pharmacopoeia (Codeine polistirex USP).
