1. Acid, Glycyrrhizic
2. Acid, Glycyrrhizinic
3. Diammonium Glycyrrhizinate
4. Dipotassium Glycyrrhizinate
5. Glycyrrhizate, Zinc
6. Glycyrrhizic Acid
7. Glycyrrhizinate, Diammonium
8. Glycyrrhizinate, Dipotassium
9. Glycyrrhizinic Acid
10. Zinc Glycyrrhizate
1. Glycyrrizin
2. Liquorice
3. Beta-glycyrrhizin
4. Nsc167409
5. Glycyrrhitin
6. Glycyrrhizinate
7. Dermacrin
8. Rizinsan K2 A2 (free Acid)
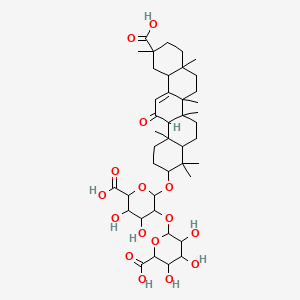
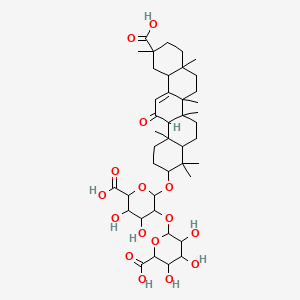
9. 6-((6-carboxy-2-((11-carboxy-4,4,6a,6b,8a,11,14b-heptamethyl-14-oxo-1,2,3,4,4a,5,6,6a,6b,7,8,8a,9,10,11,12,12a,14,14a,14b-icosahydropicen-3-yl)oxy)-4,5-dihydroxytetrahydro-2h-pyran-3-yl)oxy)-3,4,5-trihydroxytetrahydro-2h-pyran-2-carboxylic Acid
10. 29-hydroxy-11,29-dioxoolean-12-en-3-yl 2-o-hexopyranuronosylhexopyranosiduronic Acid
11. Glycrrhizin
12. Mfcd00065194
13. Glycyrrhizin, Jan
14. .alpha.-d-glucopyranosiduronic Acid,20.beta.)-20-carboxy-11-oxo-30-norolean-12-en-3-yl 2-o-.beta.-d-glucopyranuronosyl-
15. Chembl3188637
16. Schembl21424347
17. Dtxsid50859641
18. Nsc234419
19. Sy017548
20. Db-042522
21. Cs-0291800
22. Ft-0602820
23. Glycyrrhetic Acid 3-o-[b-d-glucuronopyranosyl-(1->2)-a-d-glucuronopyranoside]
| Molecular Weight | 822.9 g/mol |
|---|---|
| Molecular Formula | C42H62O16 |
| XLogP3 | 3.7 |
| Hydrogen Bond Donor Count | 8 |
| Hydrogen Bond Acceptor Count | 16 |
| Rotatable Bond Count | 7 |
| Exact Mass | 822.40378589 g/mol |
| Monoisotopic Mass | 822.40378589 g/mol |
| Topological Polar Surface Area | 267 Ų |
| Heavy Atom Count | 58 |
| Formal Charge | 0 |
| Complexity | 1730 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 19 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
DEMULCENT, MILD LAXATIVE; EXPECTORANT; USED TO DISGUISE TASTE OF MEDICATIONS
Arena, J.M. Poisoning: Toxicology-Symptoms Treatments. Third Edition. Springfield, Illinois: Charles C. Thomas, 1974., p. 575
SNMC (stronger Neominophagen C), whose active component is glycyrrhizin (a saponin extracted from licorice) has been utilized to improve the liver function in Japan. To assess the effectiveness of interferon (IFN), stronger Neominophagen C combination therapy in patients, who did not respond to interferon therapy alone, we investigate 28 patients with histology of CAH 2B at 12 weeks after interferon administration. 15 patients received interferon alone continuously (group A), and 13 patients received interferon with stronger Neominophagen C (group B) for 12 weeks thereafter. Normalization of serum ALT level was observed in 33.3% of group A and in 64.3% of group B. Disappearance of serum HVC RNA was 13.3% in group A and 38.5% in group B. But these data were not significant statistically. Histological improvement was not significant, between group A and B by Knodel's HAI score, but reversal of histological grade (Europe classification) was noted more frequently in group B. A case of post transfusion hepatitis type C, exacerbated by interferon therapy is reported. HLA class I antigen was strongly expressed in the liver tissue after administration of interferon. In this case, potentiation of cellular immunity was thought to be the cause of the exacerbation and interferon, stronger Neominophagen C combination therapy was useful in improving liver function.
PMID:7521424 Abe Y et al; Nippon Rinsho 52 (7): 1817-22 (1994)
Licorice (Glycyrrhiza glabra), a Mediterranean plant, has been used as an antidote, demulcent, and elixir folk medicine for generations in China. The main water-soluble constituent of licorice is glycyrrhizin (GL), which has been shown to possess several pharmacological properties. In this study, we show that oral feeding of glycyrrhizin to Sencar mice resulted in substantial protection against skin tumorigenesis caused by 7,12-dimethyl-benz [a]anthracene (DMBA) initiation and 12-O-tetradecanoylphorbol-13-acetate (TPA) promotion. The latent period prior to the onset of tumor development was considerably prolonged in glycyrrhizin-fed animals compared with animals not fed glycyrrhizin and resulted in significant decrease in the number of tumors per mouse, during and at the termination of the experiment. Oral feeding of glycyrrhizin in drinking water also resulted in inhibition in the binding of topically applied [3H]benzo[a]pyrene and [3H]DMBA to epidermal DNA. The possible mechanism(s) of the antitumor-initiating activity may be due to the involvement of glycyrrhizin as inhibitor of the carcinogen metabolism followed by DNA adduct formation. Our results suggest that glycyrrhizin possesses considerable antitumorigenic activity and could prove useful in protecting some forms of human cancer.
PMID:1907733 Agarwal R et al; Nutr Cancer 15 (3-4): 187-93 (1991)
Hepatocellular carcinoma (HCC) occurs in patients with hepatitis C virus-RNA positive chronic liver disease. It is important to prevent Hepatocellular carcinoma with drug administration. METHODS: A retrospective study was undertaken to evaluate the long term preventive effect of Stronger Neo-Minophagen C (SNMC) on Hepatocellular carcinoma development. Stronger Neo-Minophagen C is a Japanese medicine that is commonly administered to patients with chronic hepatitis C to improve the serum alanine aminotransferase (ALT) level. Of 453 patients diagnosed with chronic hepatitis C retrospectively in the study hospital between January 1979 and April 1984, 84 patients (Group A) had been treated with Stronger Neo-Minophagen C; Stronger Neo-Minophagen C was given at a dose of 100 mL daily for 8 weeks, then 2-7 times a week for 2-16 years (median, 10.1 years). Another group of 109 patients (Group B) could not be treated with Stronger Neo-Minophagen C or interferon for a long period of time (median, 9.2 years) and were given other herbal medicine (such as vitamin K). The patients were retrospectively monitored, and the cumulative incidence of Hepatocellular carcinoma and risk factors for Hepatocellular carcinoma were examined. RESULTS: The 10th-year rates of cumulative Hepatocellular carcinoma incidence for Groups A and B were 7% and 12%, respectively, and the 15th-year rates were 12% and 25%. By Cox regression analysis, the relative risk of Hepatocellular carcinoma incidence in patients not treated with Stronger Neo-Minophagen C (Group B) was 2.49 compared with that of patients treated with Stronger Neo-Minophagen C (Group A). CONCLUSIONS: In this study, long term administration of Stronger Neo-Minophagen C in the treatment of chronic hepatitis C was effective in preventing liver carcinogenesis.
PMID:9118029 Arase Y et al; Cancer 79 (8): 1494-500 (1997)
For more Therapeutic Uses (Complete) data for GLYCYRRHIZIN (6 total), please visit the HSDB record page.
Anti-Inflammatory Agents
Substances that reduce or suppress INFLAMMATION. (See all compounds classified as Anti-Inflammatory Agents.)
GLYCYRRHIZIN WAS ABSORBED IN RAT SMALL INTESTINE; THERE WAS NO DETECTABLE AMT OF GLYCYRRHETINIC ACID IN BLOOD AFTER BOLUS INJECTION OF GLYCYRRHIZIN INTO PORTAL VEIN; GLYCYRRHETINIC ACID WAS PRESENT IN DETECTABLE AMT IN BLOOD AFTER ORAL ADMIN.
SAKIYA ET AL; CHEM PHARM BULL 27(5) 1125 (1979)
Glycyrrhizic acid (GZA) and glycyrrhetinic acid (GRA) can be determined rapidly and precisely by high-performance liquid chromatography (HPLC) in biological fluids and tissues from experimental animals and humans. From plasma and tissues, glycyrrhizic acid and glycyrrhetinic acid are extracted by organic solvents and the extracts can directly be used for HPLC. From bile or urine, extraction and determination of glycyrrhizic acid and glycyrrhetinic acid are more difficult due to interfering endogenous compounds and conjugation of glycyrrhetinic acid with glucuronides or sulfates. Extraction of glycyrrhizic acid and glycyrrhetinic acid from urine or bile can be performed by ion-pairing followed by extraction with organic solvents or by solid phase extraction. Glycyrrhetinic acid conjugates can be determined by chromatographic separation or by pretreatment with beta-glucuronidase. The pharmacokinetics of glycyrrhetinic acid and glycyrrhizic acid can be described by a biphasic elimination from the central compartment with a dose-dependent second elimination phase. Depending on the dose, the second elimination phase in humans has a half-life of 3.5 hours for glycyrrhizic acid and between 10-30 hours for glycyrrhetinic acid. The major part of both glycyrrhetinic acid or glycyrrhizic acid is eliminated by the bile. While glycyrrhizic acid can be eliminated unmetabolized and undergoes enterohepatic cycling, Glycyrrhetinic acid is conjugated to glycyrrhetinic acid glucuronide or sulfate prior to biliary excretion. Orally administered glycyrrhizic acid is almost completely hydrolyzed by intestinal bacteria and reaches the systemic circulation as glycyrrhetinic acid.
PMID:8191540 Krahenbuhl S et al; Steroids 59 (2): 121-6 (1994)
Glycyrrhizic acid is currently of clinical interest for treatment of chronic hepatitis. It is also applied as a sweetener in food products and chewing tobacco. In some highly exposed subgroups of the population, serious side effects such as hypertension and electrolyte disturbances have been reported. In order to analyze the health risks of exposure to this compound, the kinetics of glycyrrhizic acid and its active metabolites were evaluated quantitatively. Glycyrrhizic acid and its metabolites are subject to complex kinetic processes, including enterohepatic cycling and presystemic metabolism. In humans, detailed information on these processes is often difficult to obtain. Therefore, a model was developed that describes the systemic and gastrointestinal tract kinetics of glycyrrhizic acid and its active metabolite glycyrrhetic acid in rats. Due to the physiologically based structure of the model, data from earlier in vitro and in vivo studies on absorption, enterohepatic cycling, and presystemic metabolism could be incorporated directly. The model demonstrates that glycyrrhizic acid and metabolites are transported efficiently from plasma to the bile, possibly by the hepatic transfer protein 3-alpha-hydroxysteroid dehydrogenase. Bacterial hydrolysis of the biliary excreted metabolites following reuptake of glycyrrhetic acid causes the observed delay in the terminal plasma clearance of glycyrrhetic acid. These mechanistic findings, derived from analysis of experimental data through physiologically based pharmacokinetic modeling, can eventually be used for a quantitative health risk assessment of human exposure to glycyrrhizic acid containing products. Copyright 2000 Academic Press.
PMID:10652246 Ploeger BA et al; Toxicol Appl Pharmacol 162 (3): 177-88 (2000)
To assess the multiplicity for the biliary excretion of xenobiotic conjugates, glycyrrhizic acid (glycyrrhizin) was studied in rats after intravenous (IV) injection of 10 mg/kg glycyrrhizic acid and IV infusion of inhibitors, dibromosulfophthalein and indocyanine green. Indocyanine green did not affect the biliary excretion of glycyrrhizic acid, whereas dibromosulfophthalein reduced it significantly. The plasma level of glycyrrhizic acid was increased by dibromosulfophthalein, but not by indocyanine green. In Eisai hyperbilirubinemic rats, the biliary excretion of glycyrrhizic acid was severely impaired, resulting in an increased plasma level. The findings suggested that the biliary excretion of glycyrrhizic acid is mediated by the system shared by liquiritigenin glucuronides and dibromosulfophthalein, but not by indocyanine green, and that the system is hereditarily defective in Eisai hyperbilirubinemic rats.
PMID:8987080 Shimamura H et al; Pharm Res 13 (Dec): 1833-7 (1996)
BOLUS INJECTION OF GLYCYRRHIZIN GIVEN RATS IN PORTAL VEIN, GAVE RISE IN BLOOD LEVEL OF SUBSTANCE WHICH APPEARS TO BE GLUCURONIC ACID CONJUGATE FORMED AS METABOLITE OF GLYCYRRHETINIC ACID.
SAKIYA ET AL; CHEM PHARM BULL 27(5) 1125 (1979)
GLYCYRRHIZIC ACID & ITS DERIVATIVES SHOWED PRONOUNCED ANTIINFLAMMATORY ACTION, INHIBITED DEVELOPMENT OF HISTAMINE-, SEROTONIN-, BRADKININ-, & FORMALIN-INDUCED EDEMA, & DECR VASCULAR PERMEABILITY.
NASYROV KM ET AL; FARMAKOL TOKSIKOL (MOSCOW) 43(4) 399 (1980)