
Synopsis
Synopsis
0
EU WC
0
KDMF
0
NDC API
0
VMF
0
FDF Dossiers
0
FDA Orange Book

0
Europe

0
Canada

0
Australia

0
South Africa

0
Listed Dossiers
DRUG PRODUCT COMPOSITIONS
0
US Patents
0
US Exclusivities
0
Health Canada Patents
US Medicaid
NA
Annual Reports
NA
Regulatory FDF Prices
NA
0
FDF
0
Stock Recap #PipelineProspector
0
Weekly News Recap #Phispers
1. L-isomer Leucine
2. L-leucine
3. Leucine, L Isomer
4. Leucine, L-isomer
1. L-leucine
2. 61-90-5
3. (s)-2-amino-4-methylpentanoic Acid
4. (s)-leucine
5. H-leu-oh
6. (2s)-2-amino-4-methylpentanoic Acid
7. (s)-(+)-leucine
8. Leucin
9. L-norvaline, 4-methyl-
10. Leucine, L-
11. (s)-2-amino-4-methylvaleric Acid
12. Leu
13. L-alpha-aminoisocaproic Acid
14. Leucin [german]
15. Fema No. 3297
16. Leucine (van)
17. Leucinum
18. (2s)-alpha-leucine
19. L-(+)-leucine
20. L-(-)-2-amino-4-methylpentanoic Acid
21. L-leucin
22. Leucine [usan:inn]
23. Leucinum [inn-latin]
24. Leucina [inn-spanish]
25. Leucina [latin,spanish]
26. Alpha-aminoisocaproic Acid
27. Valeric Acid, 2-amino-4-methyl-, (s)-
28. 2-amino-4-methylvaleric Acid
29. Pentanoic Acid, 2-amino-4-methyl-, (s)-
30. 2-amino-4-methylpentanoic Acid, (s)-
31. L-leuzin
32. Ai3-08899
33. Leucine, L
34. 2-amino-4-methylvaleric Acid (l)
35. 2-amino-4-methylpentanoic Acid (l)
36. Nsc 46709
37. Leucine (l-leucine)
38. (2s)-alpha-2-amino-4-methylvaleric Acid
39. Nsc-46709
40. Gmw67qnf9c
41. Chembl291962
42. L-leucine, Labeled With Tritium
43. Chebi:15603
44. L-leu
45. Mfcd00002617
46. Leucina
47. Poly-l-leucine
48. (2s)-2-amino-4-methylpentanoate
49. L-a-aminoisocaproic Acid
50. 2-amino-4-methylpentanoicacid
51. Einecs 200-522-0
52. Unii-gmw67qnf9c
53. Hsdb 7799
54. Leuoh
55. 1lan
56. 1usk
57. 3h-l-leucine
58. 4-methyl-norvalin
59. L-2-amino-4-methylpentanoic Acid
60. L-leucine;
61. (l)-leucine
62. .alpha.-amino-.gamma.-methylvaleric Acid
63. (3h)leucine
64. Alpha-amino-gamma-methylvaleric Acid
65. H-leu
66. Leucine (usp)
67. L-a-aminoisocaproate
68. 4-methyl-l-norvalin
69. L-leucine,(s)
70. Leucine (h-3)
71. 4-methyl-l-norvaline
72. L-leu-oh
73. (2s)-2-amino-4-methyl-pentanoic Acid
74. H-leu-oh Usp Grade
75. 1f2o
76. Starbld0005460
77. L-leucine (jp17)
78. L-alpha-aminoisocaproate
79. Leucine [vandf]
80. Leucine [hsdb]
81. Leucine [inci]
82. Leucine [usan]
83. Leucine [inn]
84. Leucine [ii]
85. Leucine [mi]
86. L-leucine [fcc]
87. L-leucine [jan]
88. Leucine [mart.]
89. L-leucine [fhfi]
90. Leucine [who-dd]
91. Bmse000042
92. Bmse000920
93. Ec 200-522-0
94. L-leucine, 99%, Fg
95. Schembl3889
96. Ncistruc1_001860
97. Ncistruc2_000010
98. H-leu-2-chlorotrityl Resin
99. Iso-c4h9ch(nh2)cooh
100. 2-amino-4-methyl-valericaci
101. L-leucine [usp-rs]
102. Leucine [ep Monograph]
103. 2-amino-4-methyl-valeric Acid
104. Gtpl3312
105. L-.alpha.-aminoisocaproic Acid
106. (s)-2-amino-4-methylvalerate
107. Leucine [usp Monograph]
108. Dtxsid9023203
109. Norvaline, 4-methyl-, (l)-
110. (s)-2-amino-4-methylpentanoate
111. (s)-2-amino-4-methylvalericacid
112. Pharmakon1600-01301005
113. 25322-63-8
114. Hy-n0486
115. Nci46709
116. Str01720
117. Zinc3645145
118. L-leucine, Vetec(tm), 98.5%
119. Bdbm50219348
120. Ccg-37658
121. Ncgc00013565
122. Nsc760100
123. S3753
124. Oxirane, 2,3-bis(2-chlorophenyl)-
125. (s)-2-amino-4-methyl-pentanoic Acid
126. 2-amino-4-methylvaleric Acid, (l)-
127. Akos010373766
128. Akos015841779
129. Am81871
130. Cs-w020705
131. Db00149
132. Nsc-760100
133. 2-amino-4-methylpentanoic Acid, (l)-
134. Valine Impurity C [ep Impurity]
135. L-leucine, Tested According To Ph.eur.
136. Ncgc00013565-02
137. Ncgc00096678-01
138. 71000-80-1
139. Certified Reference Material Of L-leucine
140. E641
141. 1-leucine;2-amino-4-methylpentanoic Acid
142. L-leucine, Bioultra, >=99.5% (nt)
143. Db-029966
144. L-leucine, Saj Special Grade, >=99.0%
145. Bb 0256932
146. L-leucine, Reagent Grade, >=98% (hplc)
147. L0029
148. L-leucine, Vetec(tm) Reagent Grade, >=98%
149. C00123
150. D00030
151. F70226
152. L-2700
153. M03060
154. (2s)-2-azaniumyl-4-methyl-pentanoate;h-leu-oh
155. L-leucine, Cell Culture Reagent (h-l-leu-oh)
156. 002l617
157. A821449
158. A833479
159. Q483745
160. Q-201312
161. (2r)-2-amino-4-methyl-pentanoic Acid;d-homo-valine
162. L-leucine, Certified Reference Material, Tracecert(r)
163. Lysine Hydrochloride Impurity A [ep Impurity]
164. 2b9ff792-3ca1-4bea-bc63-6d4e1a86714e
165. F8889-8638
166. Leucine, European Pharmacopoeia (ep) Reference Standard
167. Z1250208667
168. L-leucine, United States Pharmacopeia (usp) Reference Standard
169. (s)-2-amino-4-methyl-pentanoic Acid Methyl Ester Hydrochloride
170. L-leucine, Pharmaceutical Secondary Standard; Certified Reference Material
171. L-leucine, From Non-animal Source, Meets Ep, Jp, Usp Testing Specifications, Suitable For Cell Culture, 98.5-101.0%
172. L-leucine, Pharmagrade, Ajinomoto, Ep, Jp, Usp, Manufactured Under Appropriate Gmp Controls For Pharma Or Biopharmaceutical Production, Suitable For Cell Culture
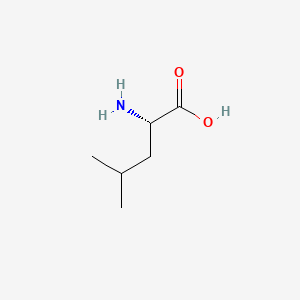
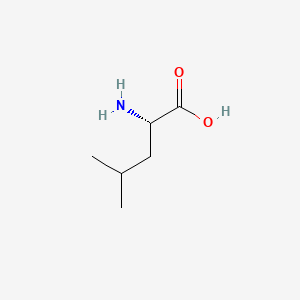
| Molecular Weight | 131.17 g/mol |
|---|---|
| Molecular Formula | C6H13NO2 |
| XLogP3 | -1.5 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 3 |
| Rotatable Bond Count | 3 |
| Exact Mass | 131.094628657 g/mol |
| Monoisotopic Mass | 131.094628657 g/mol |
| Topological Polar Surface Area | 63.3 Ų |
| Heavy Atom Count | 9 |
| Formal Charge | 0 |
| Complexity | 101 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 1 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Branched chain amino acid (BCAA)-enriched protein or amino acid mixtures and, in some cases, BCAA alone, have been used in the treatment of a variety of metabolic disorders. These amino acids have received considerable attention in efforts to reduce brain uptake of aromatic amino acids and to raise low circulating levels of BCAA in patients with chronic liver disease and encephalopathy. They have also been used in parenteral nutrition of patients with sepsis and other abnormalities.
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 705, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
/Experimental Therapy/ There have been several reports of clinical trials in which groups of healthy humans, in most cases trained athletes, were given high doses of leucine by intravenous infusion. Most of the studies involved a single dose of the amino acid. These trials measured physical and mental performance, the impact on blood levels of other amino acids, and in one case, of insulin and glucose output.
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 706, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
/Experimental Therapy/ This study was designed to evaluate the effects of enriching an essential amino acid (EAA) mixture with leucine on muscle protein metabolism in elderly and young individuals. Four (2 elderly and 2 young) groups were studied before and after ingestion of 6.7 g of EAAs. EAAs were based on the composition of whey protein [26% leucine (26% Leu)] or were enriched in leucine [41% leucine (41% Leu)]. A primed, continuous infusion of L-[ring-2H5]phenylalanine was used together with vastus lateralis muscle biopsies and leg arteriovenous blood samples for the determinations of fractional synthetic rate (FSR) and balance of muscle protein. FSR increased following amino acid ingestion in both the 26% (basal: 0.048 +/- 0.005%/hr; post-EAA: 0.063 +/- 0.007%/hr) and the 41% (basal: 0.036 +/- 0.004%/hr; post-EAA: 0.051 +/- 0.007%/hr) Leu young groups (p < 0.05). In contrast, in the elderly, FSR did not increase following ingestion of 26% Leu EAA (basal: 0.044 +/- 0.003%/hr; post-EAA: 0.049 +/- 0.006%/hr; p > 0.05) but did increase following ingestion of 41% Leu EAA (basal: 0.038 +/- 0.007%/hr; post-EAA: 0.056 +/- 0.008%/hr; p < 0.05). Similar to the FSR responses, the mean response of muscle phenylalanine net balance, a reflection of muscle protein balance, was improved (p < 0.05) in all groups, with the exception of the 26% Leu elderly group ... Increasing the proportion of leucine in a mixture of EAA can reverse an attenuated response of muscle protein synthesis in elderly but does not result in further stimulation of muscle protein synthesis in young subjects.
PMID:16507602 Katsanos, CS, et al; Am J Physiol Endocrinol Metab 291 (2): 381-7 (2006).
/Experimental Therapy/ The objective was to assess the effect of 3 mo of leucine supplementation on muscle mass and strength in healthy elderly men. Thirty healthy elderly men with a mean (+/- SEM) age of 71 +/- 4 yr and body mass index (BMI; in kg/m(2)) of 26.1 +/- 0.5 were randomly assigned to either a placebo-supplemented (n = 15) or leucine-supplemented (n = 15) group. Leucine or placebo (2.5 g) was administered with each main meal during a 3-mo intervention period. Whole-body insulin sensitivity, muscle strength (one-repetition maximum), muscle mass (measured by computed tomography and dual-energy X-ray absorptiometry), myosin heavy chain isoform distribution, and plasma amino acid and lipid profiles were assessed before, during, and/or after the intervention period. No changes in skeletal muscle mass or strength were observed over time in either the leucine- or placebo-supplemented group. No improvements in indexes of whole-body insulin sensitivity (oral glucose insulin sensitivity index and the homeostasis model assessment of insulin resistance), blood glycated hemoglobin content, or the plasma lipid profile were observed.
PMID:19321567 Verhoeven S, et al; Am J Clin Nutr 89 (5): 1468-75 (2009).
Although some evidence of reduced muscle catabolism and clear evidence of an impact on blood concentrations of other amino acids (most especially, declines in the other branched chain amino acid (BCAA) and several other neutral amino acids) can be found in these /clinical trial/ reports, none of these provides evidence of an adverse effect of leucine.
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 706, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
Long-term leucine supplementation (7.5 g/day) does not augment skeletal muscle mass or strength and does not improve glycemic control or the blood lipid profile in healthy elderly men.
PMID:19321567 Verhoeven S, et al; Am J Clin Nutr 89 (5): 1468-75 (2009).
Indicated to assist in the prevention of the breakdown of muscle proteins that sometimes occur after trauma or severe stress.
An essential amino acid. (Claim) Leucine helps with the regulation of blood-sugar levels, the growth and repair of muscle tissue (such as bones, skin and muscles), growth hormone production, wound healing as well as energy regulation. It can assist to prevent the breakdown of muscle proteins that sometimes occur after trauma or severe stress. It may also be beneficial for individuals with phenylketonuria - a condition in which the body cannot metabolize the amino acid phenylalanine
Although the free amino acids dissolved in the body fluids are only a very small proportion of the body's total mass of amino acids, they are very important for the nutritional and metabolic control of the body's proteins. ... Although the plasma compartment is most easily sampled, the concentration of most amino acids is higher in tissue intracellular pools. Typically, large neutral amino acids, such as leucine and phenylalanine, are essentially in equilibrium with the plasma. Others, notably glutamine, glutamic acid, and glycine, are 10- to 50-fold more concentrated in the intracellular pool. Dietary variations or pathological conditions can result in substantial changes in the concentrations of the individual free amino acids in both the plasma and tissue pools.
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 596, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
Table: Comparison of the Pool Sizes of Free and Protein-Bound Amino Acids in Rat Muscle [Table#7501]
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 597, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
[Table#7501]
A kinetic modeling of leucine plasma concentration changes is proposed to describe the plasma leucine reduction rate during continuous extracorporeal removal therapy (CECRT) in neonates with maple syrup urine disease. Data were obtained from seven neonates using a bicompartmental model for the best fitted curve of plasma leucine decrease during CECRT. During the first 3 hr, leucine plasma levels decreased according to an exponential curve: [Leu](t) = [Leu](i) x 0.95 x 10(-0.09t) where [Leu](t) is the leucine plasma level (umol/L) at time t (hr) during CECRT and [Leu](I) is the initial plasma level. From hr 4 to the end of CECRT, a second exponential curve was observed: [Leu](t) = [Leu](i) x 0.74 x 10(-0.05t). Plasma leucine levels obtained from three other neonates were similar to those predicted by the model. The apparent distribution volumes for leucine that correspond to the two exponential equations obtained were calculated from the leucine mass removal collected in the spent dialysate and ultrafiltrate. The distribution volume was 34 +/- 3% of body weight during the first 3 h of CECRT and 72 +/- 7% from hr 4 to the end of CECRT. These figures are similar to known values for the extracellular water compartment and for total body water in the newborn. The findings suggest that leucine handling during CECRT is similar to that of nonprotein-bound small-molecular-weight solutes such as urea.
PMID:16085796 Jouvet P, et al; Pediatr Res 58 (2): 278-82 (2005).
The transport of L-leucine by two human breast cancer cell lines has been examined. L-leucine uptake by MDA-MB-231 and MCF-7 cells was via a BCH-sensitive, Na+ -independent pathway. L-leucine uptake by both cell lines was inhibited by L-alanine, D-leucine and to a lesser extent by L-lysine but not by L-proline. Estrogen (17beta-estradiol) stimulated L-leucine uptake by MCF-7 but not by MDA-MB-231 cells. L-leucine efflux from MDA-MB-231 and MCF-7 cells was trans-stimulated by BCH in a dose-dependent fashion. The effect of external BCH on L-leucine efflux from both cell types was almost abolished by reducing the temperature from 37 to 4 degrees C. There was, however, a significant efflux of L-leucine under zero-trans conditions which was also temperature-sensitive. L-glutamine, L-leucine, D-leucine, L-alanine, AIB and L-lysine all trans-stimulated L-leucine release from MDA-MB-231 and MCF-7 cells. In contrast, D-alanine and L-proline had little or no effect. The anti-cancer agent melphalan inhibited L-leucine uptake by MDA-MB-231 cells but had no effect on L-leucine efflux. Quantitative real-time PCR revealed that LAT1 mRNA was approximately 200 times more abundant than LAT2 mRNA in MCF-7 cells and confirmed that MDA-MB-231 cells express LAT1 but not LAT2 mRNA. LAT1 mRNA levels were higher in MCF-7 cells than in MDA-MB-231 cells. Furthermore, LAT1 mRNA was more abundant than CD98hc mRNA in both MDA-MB-231 and MCF-7 cells. The results suggest that system L is the major transporter for L-leucine in both MDA-MB-231 and MCF-7 cells. It is possible that LAT1 may be the major molecular correlate of system L in both cell types. However, not all of the properties of system L reflected those of LAT1/LAT2/CD98hc.
PMID:15328053 Shennan DB, et al; Biochim Biophysica Acta 1664 (2): 206-16 (2004).
For more Absorption, Distribution and Excretion (Complete) data for L-Leucine (7 total), please visit the HSDB record page.
The branched-chain amino acids (BCAA) -- leucine, isoleucine, and valine -- differ from most other indispensable amino acids in that the enzymes initially responsible for their catabolism are found primarily in extrahepatic tissues. Each undergoes reversible transamination, catalyzed by a branched-chain aminotransferase (BCAT), and yields alpha-ketoisocaproate (KIC, from leucine), alpha-keto-beta-methylvalerate (KMV, from isoleucine), and alpha-ketoisovalerate (KIV, from valine). Each of these ketoacids then undergoes an irreversible, oxidative decarboxylation, catalyzed by a branchedchain ketoacid dehydrogenase (BCKAD). The latter is a multienzyme system located in mitochondrial membranes. The products of these oxidation reactions undergo further transformations to yield acetyl CoA, propionyl CoA, acetoacetate, and succinyl CoA; the BCAA are thus keto- and glucogenic.
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 704, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
Once the amino acid deamination products enter the tricarboxylic acid (TCA) cycle (also known as the citric acid cycle or Krebs cycle) or the glycolytic pathway, their carbon skeletons are also available for use in biosynthetic pathways, particularly for glucose and fat. Whether glucose or fat is formed from the carbon skeleton of an amino acid depends on its point of entry into these two pathways. If they enter as acetyl-CoA, then only fat or ketone bodies can be formed. The carbon skeletons of other amino acids can, however, enter the pathways in such a way that their carbons can be used for gluconeogenesis. This is the basis for the classical nutritional description of amino acids as either ketogenic or glucogenic (ie, able to give rise to either ketones [or fat] or glucose). Some amino acids produce both products upon degradation and so are considered both ketogenic and glucogenic. /Amino acids/
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 606, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
Kinetics of leucine and its oxidation were determined in human pregnancy and in the newborn infant, using stable isotopic tracers, to quantify the dynamic aspects of protein metabolism. These data show that in human pregnancy there is a decrease in whole-body rate of leucine turnover compared with nonpregnant women. In addition, data in newborn infants show that leucine turnover expressed as per kg body weight is higher compared with adults. The administering of nutrients resulted in a suppression of the whole-body rate of proteolysis ... The relations among the transamination of leucine, leucine N kinetics, and urea synthesis and glutamine kinetics in human pregnancy and newborn infants /were also examined/. In human pregnancy, early in gestation, there is a significant decrease in urea synthesis in association with a decrease in the rate of transamination of leucine. A linear correlation was evident between the rate of leucine reamination and urea synthesis during fasting in pregnant and nonpregnant women. In healthy-term newborn and growing infants, although the reamination of leucine was positively related to glutamine flux, leucine reamination was negatively related to urea synthesis, suggesting a redirection of amino N toward protein accretion ...
PMID:16365099 Kalhan SC, Parimi PS; J Nutr 136 (1 Suppl): 281-7 (2006).
The metabolic disease 3-methylglutaconic aciduria type I (MGA1) is characterized by an abnormal organic acid profile in which there is excessive urinary excretion of 3-methylglutaconic acid, 3-methylglutaric acid and 3-hydroxyisovaleric acid. Affected individuals display variable clinical manifestations ranging from mildly delayed speech development to severe psychomotor retardation with neurological handicap. MGA1 is caused by reduced or absent 3-methylglutaconyl-coenzyme A (3-MG-CoA) hydratase activity within the leucine degradation pathway. The human AUH gene has been reported to encode for a bifunctional enzyme with both RNA-binding and enoyl-CoA-hydratase activity. In addition, it was shown that mutations in the AUH gene are linked to MGA1 ...
PMID:16640564 Mack M, et al; FEBS J 273 (9): 2012-22 (2006).
For more Metabolism/Metabolites (Complete) data for L-Leucine (8 total), please visit the HSDB record page.
This group of essential amino acids are identified as the branched-chain amino acids, BCAAs. Because this arrangement of carbon atoms cannot be made by humans, these amino acids are an essential element in the diet. The catabolism of all three compounds initiates in muscle and yields NADH and FADH2 which can be utilized for ATP generation. The catabolism of all three of these amino acids uses the same enzymes in the first two steps. The first step in each case is a transamination using a single BCAA aminotransferase, with a-ketoglutarate as amine acceptor. As a result, three different a-keto acids are produced and are oxidized using a common branched-chain a-keto acid dehydrogenase, yielding the three different CoA derivatives. Subsequently the metabolic pathways diverge, producing many intermediates. The principal product from valine is propionylCoA, the glucogenic precursor of succinyl-CoA. Isoleucine catabolism terminates with production of acetylCoA and propionylCoA; thus isoleucine is both glucogenic and ketogenic. Leucine gives rise to acetylCoA and acetoacetylCoA, and is thus classified as strictly ketogenic. There are a number of genetic diseases associated with faulty catabolism of the BCAAs. The most common defect is in the branched-chain a-keto acid dehydrogenase. Since there is only one dehydrogenase enzyme for all three amino acids, all three a-keto acids accumulate and are excreted in the urine. The disease is known as Maple syrup urine disease because of the characteristic odor of the urine in afflicted individuals. Mental retardation in these cases is extensive. Unfortunately, since these are essential amino acids, they cannot be heavily restricted in the diet; ultimately, the life of afflicted individuals is short and development is abnormal The main neurological problems are due to poor formation of myelin in the CNS.
The mechanism of intracellular protein degradation, by which protein is hydrolyzed to free amino acids, is more complex and is not as well characterized at the mechanistic level as that of synthesis. A wide variety of different enzymes that are capable of splitting peptide bonds are present in cells. However, the bulk of cellular proteolysis seems to be shared between two multienzyme systems: the lysosomal and proteasomal systems. The lysosome is a membrane-enclosed vesicle inside the cell that contains a variety of proteolytic enzymes and operates mostly at acid pH. Volumes of the cytoplasm are engulfed (autophagy) and are then subjected to the action of the protease enzymes at high concentration. This system is thought to be relatively unselective in most cases, although it can also degrade specific intracellular proteins. The system is highly regulated by hormones such as insulin and glucocorticoids, and by amino acids. The second system is the ATP-dependent ubiquitin-proteasome system, which is present in the cytoplasm. The first step is to join molecules of ubiquitin, a basic 76-amino acid peptide, to lysine residues in the target protein. Several enzymes are involved in this process, which selectively targets proteins for degradation by a second component, the proteasome.
NAS, Food and Nutrition Board, Institute of Medicine; Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academy Press, Washington, D.C., pg. 602, 2009. Available from, as of March 10, 2010: https://www.nap.edu/catalog/10490.html
Dietary leucine transported into the brain parenchyma serves several functions. Most prominent is the role of leucine as a metabolic precursor of fuel molecules, alpha-ketoisocaproate and ketone bodies. As alternatives to glucose, these compounds are forwarded by the producing astrocytes to the adjacent neural cells. Leucine furthermore participates in the maintenance of the nitrogen balance in the glutamate/glutamine cycle pertinent to the neurotransmitter glutamate. Leucine also serves as a regulator of the activity of some enzymes important for brain energy metabolism. Another role of leucine as an informational molecule is in mTOR signaling that participates in the regulation of food ingestion. The importance of leucine for brain function is stressed by the fact that inborn errors in its metabolism cause metabolic diseases often associated with neuropathological symptoms. In this overview, the current knowledge on the metabolic and regulatory roles of this essential amino acid in neural cells are briefly summarized.
PMID:17721727 Murin R, Hamprecht B; Neurochem Res 33 (2): 279-84 (2008).
Ingestion of a leucine-enriched essential amino acid nutrient solution rapidly and potently activates the mammalian target of rapamycin signalling pathway and protein synthesis in human skeletal muscle. Further, mTOR signalling and muscle protein synthesis are enhanced when leucine-enriched nutrients are ingested following resistance exercise. The addition of leucine to regular meals may improve the ability of feeding to stimulate protein synthesis in old human muscle. ... Leucine and essential amino acids appear to stimulate human muscle protein synthesis primarily by activating the mammalian target of rapamycin signalling pathway. How human muscle cells sense an increase in leucine and/or essential amino acids to activate mammalian target of rapamycin signalling is currently unknown. Recent work, however, suggests that the kinases hVps34 and MAP43K may be involved. Leucine-enriched essential amino acid ingestion, in combination with resistance exercise in some cases, may be a useful intervention to promote mTOR signalling and protein synthesis in an effort to counteract a variety of muscle wasting conditions (e.g. sarcopenia, cachexia, AIDS, inactivity/bed rest, sepsis, kidney failure, and trauma).
PMID:18403916 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5096790 Drummond MJ, Rasmussen BB; Curr Opin Clin Nutr Metab Care 11 (3): 222-6 (2008).
One of the amino acids most affected by exercise is the branched-chain amino acid leucine. ... Leucine appears to exert a synergistic role with insulin as a regulatory factor in the insulin/ phosphatidylinositol-3 kinase (PI3-K) signal cascade. Insulin serves to activate the signal pathway, while leucine is essential to enhance or amplify the signal for protein synthesis at the level of peptide initiation. Studies feeding amino acids or leucine soon after exercise suggest that post-exercise consumption of amino acids stimulates recovery of muscle protein synthesis via translation regulations ...
PMID:12501002 Layman DK; Can J Appl Physiol 27 (6): 646-63 (2002).
For more Mechanism of Action (Complete) data for L-Leucine (12 total), please visit the HSDB record page.
Related Excipient Companies

Excipients by Applications
Market Place

REF. STANDARDS & IMPURITIES

ABOUT THIS PAGE
23
PharmaCompass offers a list of L-Leucine API API manufacturers, exporters & distributors, which can be sorted by GMP, USDMF, JDMF, KDMF, CEP (COS), WC, Price,and more, enabling you to easily find the right L-Leucine API manufacturer or L-Leucine API supplier for your needs.
Send us enquiries for free, and we will assist you in establishing a direct connection with your preferred L-Leucine API manufacturer or L-Leucine API supplier.
PharmaCompass also assists you with knowing the L-Leucine API API Price utilized in the formulation of products. L-Leucine API API Price is not always fixed or binding as the L-Leucine API Price is obtained through a variety of data sources. The L-Leucine API Price can also vary due to multiple factors, including market conditions, regulatory modifications, or negotiated pricing deals.
A L-Leucine API manufacturer is defined as any person or entity involved in the manufacture, preparation, processing, compounding or propagation of L-Leucine API, including repackagers and relabelers. The FDA regulates L-Leucine API manufacturers to ensure that their products comply with relevant laws and regulations and are safe and effective to use. L-Leucine API API Manufacturers are required to adhere to Good Manufacturing Practices (GMP) to ensure that their products are consistently manufactured to meet established quality criteria.
click here to find a list of L-Leucine API manufacturers with USDMF, JDMF, KDMF, CEP, GMP, COA and API Price related information on PhamaCompass.
A L-Leucine API supplier is an individual or a company that provides L-Leucine API active pharmaceutical ingredient (API) or L-Leucine API finished formulations upon request. The L-Leucine API suppliers may include L-Leucine API API manufacturers, exporters, distributors and traders.
click here to find a list of L-Leucine API suppliers with USDMF, JDMF, KDMF, CEP, GMP, COA and API Price related information on PharmaCompass.
A L-Leucine API DMF (Drug Master File) is a document detailing the whole manufacturing process of L-Leucine API active pharmaceutical ingredient (API) in detail. Different forms of L-Leucine API DMFs exist exist since differing nations have different regulations, such as L-Leucine API USDMF, ASMF (EDMF), JDMF, CDMF, etc.
A L-Leucine API DMF submitted to regulatory agencies in the US is known as a USDMF. L-Leucine API USDMF includes data on L-Leucine API's chemical properties, information on the facilities and procedures used, and details about packaging and storage. The L-Leucine API USDMF is kept confidential to protect the manufacturer’s intellectual property.
click here to find a list of L-Leucine API suppliers with USDMF on PharmaCompass.
The Pharmaceuticals and Medical Devices Agency (PMDA) established the Japan Drug Master File (JDMF), also known as the Master File (MF), to permit Japanese and foreign manufacturers of drug substances, intermediates, excipients, raw materials, and packaging materials (‘Products’) to voluntarily register confidential information about the production and management of their products in Japan.
The L-Leucine API Drug Master File in Japan (L-Leucine API JDMF) empowers L-Leucine API API manufacturers to present comprehensive information (e.g., production methods, data, etc.) to the review authority, i.e., PMDA (Pharmaceuticals & Medical Devices Agency).
PMDA reviews the L-Leucine API JDMF during the approval evaluation for pharmaceutical products. At the time of L-Leucine API JDMF registration, PMDA checks if the format is accurate, if the necessary items have been included (application), and if data has been attached.
click here to find a list of L-Leucine API suppliers with JDMF on PharmaCompass.
A L-Leucine API CEP of the European Pharmacopoeia monograph is often referred to as a L-Leucine API Certificate of Suitability (COS). The purpose of a L-Leucine API CEP is to show that the European Pharmacopoeia monograph adequately controls the purity of L-Leucine API EP produced by a given manufacturer. Suppliers of raw materials can prove the suitability of L-Leucine API to their clients by showing that a L-Leucine API CEP has been issued for it. The manufacturer submits a L-Leucine API CEP (COS) as part of the market authorization procedure, and it takes on the role of a L-Leucine API CEP holder for the record. Additionally, the data presented in the L-Leucine API CEP (COS) is managed confidentially and offers a centralized system acknowledged by numerous nations, exactly like the L-Leucine API DMF.
A L-Leucine API CEP (COS) is recognised by all 36 nations that make up the European Pharmacopoeia Convention. L-Leucine API CEPs may be accepted in nations that are not members of the Ph. Eur. at the discretion of the authorities there.
click here to find a list of L-Leucine API suppliers with CEP (COS) on PharmaCompass.
L-Leucine API Active pharmaceutical ingredient (API) is produced in GMP-certified manufacturing facility.
GMP stands for Good Manufacturing Practices, which is a system used in the pharmaceutical industry to make sure that goods are regularly produced and monitored in accordance with quality standards. The FDA’s current Good Manufacturing Practices requirements are referred to as cGMP or current GMP which indicates that the company follows the most recent GMP specifications. The World Health Organization (WHO) has its own set of GMP guidelines, called the WHO GMP. Different countries can also set their own guidelines for GMP like China (Chinese GMP) or the EU (EU GMP).
PharmaCompass offers a list of L-Leucine API GMP manufacturers, exporters & distributors, which can be sorted by USDMF, JDMF, KDMF, CEP (COS), WC, API price, and more, enabling you to easily find the right L-Leucine API GMP manufacturer or L-Leucine API GMP API supplier for your needs.
A L-Leucine API CoA (Certificate of Analysis) is a formal document that attests to L-Leucine API's compliance with L-Leucine API specifications and serves as a tool for batch-level quality control.
L-Leucine API CoA mostly includes findings from lab analyses of a specific batch. For each L-Leucine API CoA document that a company creates, the USFDA specifies specific requirements, such as supplier information, material identification, transportation data, evidence of conformity and signature data.
L-Leucine API may be tested according to a variety of international standards, such as European Pharmacopoeia (L-Leucine API EP), L-Leucine API JP (Japanese Pharmacopeia) and the US Pharmacopoeia (L-Leucine API USP).
