
Synopsis
Synopsis
0
API Suppliers
0
USDMF
0
CEP/COS
0
JDMF
0
EU WC
0
KDMF
0
NDC API
0
VMF
0
Listed Suppliers
0
API
0
FDF
0
FDF Dossiers
0
FDA Orange Book

0
Europe

0
Canada

0
Australia

0
South Africa

0
Listed Dossiers
DRUG PRODUCT COMPOSITIONS
0
EDQM
0
USP
0
JP
0
Others
0
US Patents
0
US Exclusivities
0
Health Canada Patents
0
Data Compilation #PharmaFlow
0
Stock Recap #PipelineProspector
0
Weekly News Recap #Phispers
US Medicaid
NA
Annual Reports
NA
Finished Drug Prices
NA
1. 2 Aminoethanethiol
2. 2-aminoethanethiol
3. 35s-labeled Cysteamine
4. Becaptan
5. Beta Mercaptoethylamine
6. Beta-mercaptoethylamine
7. Bitartrate, Cysteamine
8. Cystagon
9. Cysteamine Bitartrate
10. Cysteamine Dihydrochloride
11. Cysteamine Hydrobromide
12. Cysteamine Hydrochloride
13. Cysteamine Maleate (1:1)
14. Cysteamine Tartrate
15. Cysteamine Tartrate (1:1)
16. Cysteamine Tosylate
17. Cysteamine, 35s Labeled
18. Cysteamine, 35s-labeled
19. Cysteinamine
20. Dihydrochloride, Cysteamine
21. Hydrobromide, Cysteamine
22. Hydrochloride, Cysteamine
23. Mercamine
24. Mercaptamine
25. Mercaptoethylamine
26. Tartrate, Cysteamine
27. Tosylate, Cysteamine
1. 2-aminoethanethiol
2. 60-23-1
3. Mercaptamine
4. Thioethanolamine
5. Becaptan
6. Mercamine
7. Beta-mercaptoethylamine
8. 2-mercaptoethylamine
9. Cysteinamine
10. Cysteamin
11. Lambraten
12. Lambratene
13. Beta-aminoethanethiol
14. Cystagon
15. Riacon
16. Decarboxycysteine
17. Mercaptoethylamine
18. 2-amino-1-ethanethiol
19. Ethanethiol, 2-amino-
20. Cisteamina
21. 2-aminoethyl Mercaptan
22. Beta-aminoethylthiol
23. 2-mercaptoethanamine
24. Mercaptamin
25. (2-mercaptoethyl)amine
26. Beta-mea
27. Mea (mercaptan)
28. Ethanethiolamine
29. 2-amino-ethanethiol
30. Aminoethyl Mercaptan
31. Mercaptamina
32. Mercaptaminum
33. Cysteamide
34. Mecramine
35. Mercamin
36. Merkamin
37. Cisteamina [italian]
38. Cystaran
39. Mercaptaminum [inn-latin]
40. Mercaptamina [inn-spanish]
41. 1-amino-2-mercaptoethylamine
42. L-1573
43. Cysteamine (usan)
44. Cysteamine [usan]
45. Wr 347
46. 2-aminoethane-1-thiol
47. B-mercaptoethylamine
48. Nsc 647528
49. Mercaptamine (inn)
50. Mercaptamine [inn]
51. .beta.-mercaptoethylamine
52. Nsc-647528
53. 5ux2sd1ke2
54. Chebi:17141
55. 2-aminoethane-1-thiol; Cysteamine
56. Nsc647528
57. Ncgc00015691-03
58. Cysteamine [usan:ban]
59. Beta-mercaptoethylamine;2-aminoethanethiol;2-mercaptoethylamine
60. Cysteamine Bitartate
61. Ccris 3083
62. Hsdb 7353
63. Einecs 200-463-0
64. L 1573
65. Unii-5ux2sd1ke2
66. Cystagone
67. B-aminoethylthiol
68. B-mea
69. B-aminoethanethiol
70. Mercapto Ethylamine
71. Dhl
72. Mfcd00008196
73. 2-amino-ethyl Thiol
74. Cash
75. .beta.-mea
76. Cysteamine, ~95%
77. Cysteamine, Free Base
78. .beta.-aminoethylthiol
79. Spectrum_001755
80. .beta.-aminoethanethiol
81. Cysteamine [mi]
82. Specplus_000654
83. Cysteamine [hsdb]
84. Cysteamine [inci]
85. Lopac-m-6500
86. Dsstox_cid_2875
87. Cysteamine [vandf]
88. Bmse000388
89. Chembl602
90. C-9500
91. Dsstox_rid_76770
92. Dsstox_gsid_22875
93. Kbioss_002235
94. Mercaptamine [mart.]
95. Divk1c_006750
96. Mercaptamine [who-dd]
97. Bdbm7968
98. Gtpl7440
99. 2,3-deshydrolanthionine
100. Dtxsid3022875
101. Kbio1_001694
102. Kbio2_002235
103. Kbio2_004803
104. Kbio2_007371
105. Cysteamine, >=98.0% (rt)
106. Bcp15015
107. Zinc8034121
108. Tox21_113092
109. Hy-77591a
110. S6402
111. Stk315355
112. Akos003793343
113. Ccg-204834
114. Db00847
115. Sb75360
116. Sdccgsbi-0050727.p004
117. Cas-60-23-1
118. Ncgc00015691-01
119. Ncgc00015691-02
120. Ncgc00015691-04
121. Ncgc00015691-14
122. Ncgc00162236-01
123. Ncgc00162236-02
124. Amy202100105
125. As-56218
126. Bp-13401
127. Nci60_002000
128. Sbi-0050727.p003
129. Db-053562
130. A0648
131. Ft-0611243
132. C01678
133. D03634
134. D88299
135. D88360
136. Ab00053754_09
137. Ab00053754_10
138. A832648
139. Q617563
140. F0001-1576
141. 2dfda1f8-7010-4225-8280-ab1c4c43f546
142. 2-aminoethanethiol;cysteamine, Beta-mercaptoethylamine, 2-mercaptoethylamine, Decarboxycysteine, Thioethanolamine, Mercaptamine
143. 2-mercaptoethylamine, Polymer-bound, 70-90 Mesh, Extent Of Labeling: 0.6-1.1 Mmol/g Loading, 1 % Cross-linked With Divinylbenzene
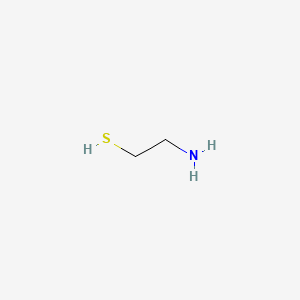
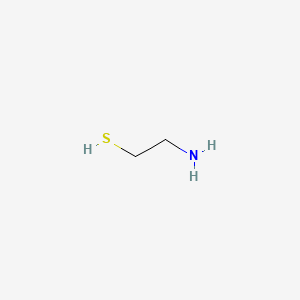
| Molecular Weight | 77.15 g/mol |
|---|---|
| Molecular Formula | C2H7NS |
| XLogP3 | -0.4 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 2 |
| Rotatable Bond Count | 1 |
| Exact Mass | 77.02992040 g/mol |
| Monoisotopic Mass | 77.02992040 g/mol |
| Topological Polar Surface Area | 27 Ų |
| Heavy Atom Count | 4 |
| Formal Charge | 0 |
| Complexity | 10 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 2 | |
|---|---|
| Drug Name | CYSTAGON |
| Active Ingredient | CYSTEAMINE BITARTRATE |
| Company | MYLAN (Application Number: N020392) |
| 2 of 2 | |
|---|---|
| Drug Name | CYSTARAN |
| Active Ingredient | CYSTEAMINE HYDROCHLORIDE |
| Company | LEADIANT BIOSCI INC (Application Number: N200740) |
Cysteamine is indicated for the management of nephropathic cystinosis in children and adults. /Included in US product labeling/
Thomson.Micromedex. Drug Information for the Health Care Professional. 25th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2005.
Nephropathic cystinosis is a rare, autosomal recessive lysosomal storage disorder caused by mutations in the CTNS gene that codes for a cystine transporter in the lysosomal membrane. Affected patients store 50-100 times the normal amounts of cystine in their cells, and suffer renal tubular and glomerular disease, growth retardation, photophobia, and other systemic complications, including a myopathy and swallowing dysfunction. Using videofluoroscopy and ultrasound examinations, we assessed the swallowing function of 101 patients with nephropathic cystinosis on their most recent admission to the National Institutes of Health Clinical Center between 1987 and 2004. These patients ranged in age from 6 to 45 years; more than half had significant complaints of swallowing difficulty. On examination of barium swallow, the oral, pharyngeal, and esophageal phases of swallowing were abnormal in 24%, 51%, and 73% of patients, respectively. The frequency of dysfunction increased with age for each phase of swallowing. Both the Swallowing Severity Score (a measure of dysfunction on barium swallow) and the Oral Muscle Composite Score (a reflection of vocal strength, oral-facial movement, and tongue and lip function) increased (that is, worsened) with the number of years that a patient was not receiving treatment with cysteamine, the cystine-depleting agent of choice in cystinosis. The severity scores decreased with the number of years on cysteamine therapy. The Swallowing Severity Score varied directly with the severity of muscle disease, but was not correlated with the presence or absence of the 57-kb CTNS deletion that commonly occurs in nephropathic cystinosis patients. We conclude that swallowing dysfunction in cystinosis presents a risk of fatal aspiration, correlates with the presence of muscle atrophy, and, based on cross-sectional data, increases in frequency with age and number of years without cysteamine treatment. Cystine-depleting therapy with cysteamine should be considered the treatment of choice for both pre- and posttransplant cystinosis patients.
PMID:15879904 Sonies BC et al; Medicine (Baltimore) 84 (3): 137-46 (2005)
/EXPL THER/ N-Acetylcysteine (NAC) is protective against acetaminophen-induced hepatotoxicity primarily by providing precursor for the glutathione synthetase pathway, while cysteamine has been demonstrated to alter the cytochrome P-450 dependent formation of toxic acetaminophen metabolite. Mice administered acetaminophen (500 mg/kg) had elevations of serum alanine aminotransferase (ALT) to 273.0 +/- 37.5 and 555.8 +/- 193.4 U/mL at 12 and 24 h, respectively, after injection. Administration of cysteamine (100 mg/kg) or NAC (500 mg/kg) significantly reduced serum ALT activity (p less than 0.001). Reducing the dose of NAC or cysteamine by 50% greatly reduced their hepatoprotective effect while the co-administration of the reduced doses of NAC (250 mg/kg) and cysteamine (50 mg/kg) following acetaminophen overdose prevented elevation of serum ALT activity (39.2 +/- 1.17 and 32.5 +/- 5.63 U/mL at 12 and 24 h post-injection, p less than 0.001) and preserved normal mouse hepatic histology. Neither NAC (500 mg/kg), cysteamine (100 mg/kg), or the lower doses in combination of both agents were found to alter the half-life or peak levels of acetaminophen. Liver microsomal aryl hydrocarbon hydroxylase activity measured 24 h after drug administration was not significantly different between treatment groups and controls receiving only saline. These results indicate a possible role for the concomitant use of NAC and cysteamine in the prevention of hepatic necrosis following toxic doses of acetaminophen. Neither decrease in plasma acetaminophen levels nor depression of cytochrome P-450 enzyme activity appears to be the mechanism of protection when these doses of NAC, cysteamine, or both drugs together are administered with a toxic dose of acetaminophen in mice.
PMID:1581851 Peterson TC, Brown IR; Can J Physiol Pharmacol 70 (1): 20-8 (1992)
Although renal disease is the most prominent feature of the lysosomal storage disease cystinosis, corneal cystine crystal formation remains a major complication, leading to photophobia, corneal erosions, and keratopathies. Moreover, the extent of corneal crystal accumulation reflects the course and severity of the disease itself, and the cornea is accessible to direct examination. Therefore, we employed a scoring system, based on a library of slit-lamp photographs of corneas with increasing crystal densities (0.00-3.00), to assess the degree of crystal accumulation in 170 patients with nephropathic cystinosis examined at the National Institutes of Health between 1976 and 2000. None of the patients had received topical cystine-depleting therapy at the time of the evaluation. In this natural history study, infants in the first year of life had absent or minimal corneal crystals, i.e., a corneal cystine crystal score (CCCS) of 0 or 0.25. However, the CCCS increased linearly with age, such that every patient had visible crystals by 16 months of age, and plateaued at approximately 3.00 by early adolescence. Longitudinal studies in representative patients support the cross-sectional results. Individuals homozygous for the common 57-kb deletion involving the cystinosis gene (CTNS) displayed the same course of corneal crystal accumulation as did individuals not bearing the large deletion. Patients with ocular or nonnephropathic cystinosis had CCCSs that were, in general, half those expected for patients with nephropathic cystinosis of the same age. Administration of 0.55% cysteamine eyedrops, given 6 to 12 times per day, dissolved corneal cystine crystals in 10 representative patients with nephropathic cystinosis aged 1 to 32 years within 8 to 41 months.
PMID:11001803 Gahl WA et al; Mol Genet Metab 71 (1-2): 100-20 (2000)
The necessity to apply near-toxic amounts of radioprotective drugs to achieve adequate protection during radiation treatments represents a major problem in human medicine. One of the promising strategies to suppress the toxicity of these drugs involves their incorporation into biocompatible polymers. In this study cysteamine (Cy) was attached to poly(oxyethylene phosphate), POEP, via an ionic bond. Radioprotection of E. coli B cells by this substance and its acute toxicity on male C57 BL mice were measured. The toxicity of Cy immobilized within the poly(oxyethylene phosphate) was significantly lower in comparison to pure Cy while its radioprotective efficiency remained high at half the maximum tolerable dose. The high radioprotective efficiency of the Cy/POEP complexes was further confirmed on mice at different polymer molecular weight characteristics, drug immobilization degrees, application times, and doses. It was found that POEP with molecular weight 4700 Da and containing 24% repeating units with attached Cy has the highest protection potential combined with a depot effect.
PMID:12477362 Georgieva R et al; J Med Chem 45 (26): 5797-801 (2002)
The most frequent adverse reactions seen involve the GI and central nervous systems. These are especially prominent at the initiation of therapy. Temporarily suspending treatment, then gradual reintroduction may be effective in improving tolerance. The most common events (> 5%) were vomiting (35%), anorexia (31%), fever (22%), diarrhea (16%), lethargy 11%) and rash (7%). Other adverse reactions are as follows: CNS: Somnolence; encephalopathy; headache; seizures; ataxia; confusion; tremor; hyperkinesia; decreased hearing; dizziness; jitteriness. GI: Nausea; bad breath; abdominal pain; dyspepsia; constipation; gastroenteritis; duodenitis; duodenal ulceration. Psychiatric: Nervousness; abnormal thinking; depression; emotional lability; hallucinations; nightmares. Miscellaneous: Abnormal liver function; anemia; leukopenia; dehydration; hypertension; urticaria.
Novak, K.M. (ed.). Drug Facts and Comparisons 59th Edition 2005. Wolters Kluwer Health. St. Louis, Missouri 2005., p. 738
Cysteamine has occasionally been associated with reversible leukopenia and abnormal liver function studies. Therefore, monitor blood counts and liver function studies.
Novak, K.M. (ed.). Drug Facts and Comparisons 59th Edition 2005. Wolters Kluwer Health. St. Louis, Missouri 2005., p. 738
Patients sensitive to penicillamine may be sensitive to this medication also.
Thomson.Micromedex. Drug Information for the Health Care Professional. 25th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2005.
FDA Pregnancy category C: Adequate, well controlled human studies are lacking, and animal studies have shown risk to the fetus or are lacking as well. There is a chance of fetal harm if the drug is given during pregnancy; but the potential benefits may outweigh the potential risk.
Thomson.Micromedex. Drug Information for the Health Care Professional. 25th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2005.
For more Drug Warnings (Complete) data for CYSTEAMINE (11 total), please visit the HSDB record page.
The bitartrate salt of cysteamine is used for the oral treatment of nephropathic cystinosis and cystinuria in children 6 years old and above, and adults. The hydrochloride salt, used in eye drop preparations, is indicated for the treatment of corneal cystine crystal accumulation in patients with cystinosis.
FDA Label
Cystadrops is indicated for the treatment of corneal cystine crystal deposits in adults and children from 2 years of age with cystinosis.
Treatment of corneal cystine deposits,
Cystine accumulation is the cause of organ damage in cystinosis. Cysteamine prevents the accumulation of cystine crystals in the body and is specifically prescribed to prevent kidney and eye damage. Cysteamine converts cystine into a form that may easily exit cells, preventing harmful accumulation.
Cystine Depleting Agents
Compounds and drugs that react with CYSTINE and convert it into a compound that can be more easily metabolized or intracellularly transported. Drugs in this class have been used to treat CYSTINOSIS. (See all compounds classified as Cystine Depleting Agents.)
S01XA21
S01XA21
A16AA04
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
A - Alimentary tract and metabolism
A16 - Other alimentary tract and metabolism products
A16A - Other alimentary tract and metabolism products
A16AA - Amino acids and derivatives
A16AA04 - Mercaptamine
S - Sensory organs
S01 - Ophthalmologicals
S01X - Other ophthalmologicals
S01XA - Other ophthalmologicals
S01XA21 - Mercaptamine
Absorption
Orally administered cysteamine is absorbed in the gastrointestinal tract and reaches its maximum plasma concentration in about 1.4 hours, with some variation according to the type of formulation (delayed versus immediate-release). One pharmacokinetic study of adults with Cystic Fibrosis revealed a Cmax of 2.86 mg/L.The maximum plasma concentration after administration of cysteamine eye drops is unknown, however, it is likely to be considerably lower than oral administration. According to prescribing information, the AUC 0-12 h for the delayed-release oral tablets is 99.26 44.2 mol*h/L with a Cmax of 27.70 14.99 mol/L. The AUC 0-12 for the immediate-release tablets is 192.00 75.62 mol*h/L with a Cmax of 37.72 12.10 mol/L.
Volume of Distribution
Cysteamine has a volume of distribution of about 129 L, according to one pharmacokinetic study. Prescribing information indicates a volume of distribution of 382 L for the delayed-release formulation and 198 L for the immediate-release preparation. It is known to cross the blood-brain barrier.
Clearance
The plasma clearance of cysteamine is about 1.2 - 1.4 L/min. One reference mentions a clearance of 89.9 L/h in patients with Cystic Fibrosis.
/Cysteamine is/ poorly bound to plasma proteins.
Thomson.Micromedex. Drug Information for the Health Care Professional. 25th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2005.
It is not known whether cysteamine is distributed into breast milk.
Thomson.Micromedex. Drug Information for the Health Care Professional. 25th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2005.
In a patient with cystinosis, an oral dose of cysteamine was absorbed rapidly, with plasma cysteamine reaching a maximum of 56 microM 1 h after the dose. By 1.8 h the plasma cysteamine concentration had decreased to one-half the maximum value.
PMID:3364734 Smolin LA et al; Anal Biochem.168 (2): 374-9 (1988)
Cysteamine bitartrate was administered to 11 cystinosis patients at their regular dose level in a single-dose, open-label, steady-state study. Blood samples were collected and analysed for plasma cysteamine and white blood cell cystine content and pharmacokinetic and pharmacodynamic parameters estimated by NONMEM analysis using a linked pharmacokinetic-pharmacodynamic model. Cysteamine was rapidly cleared from the plasma (mean CL/F = 32.3 mL min(-1) kg(-1), range = 17.3-52.2), appeared to be extensively distributed (mean Vss/F = 15.1 l, range 2.7-32.3) and exhibited a mean Tmax of 1.4 hr. White blood cell cystine content post-dosing was significantly decreased compared with pre- and post-dose values (average decrement approximately 47%). A counter-clockwise hysteresis was noted in all patients, suggestive of a lag time (mean Tlag = 0.44 hr, range 0.22-0.92) between drug concentration and effect. The results of this study establish that cysteamine is rapidly cleared from the plasma but that an every 6 hr dosing interval adequately maintains white blood cell cystine content below the target of 1 nmol cystine per mg protein. /Cysteamine bitartrate/
PMID:14651726 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1884393 Belldina EB et al; Br J Clin Pharmacol 56 (5): 520-5 (2003)
Cysteamine (beta-mercaptoethylamine, MEA) is currently used to treat children with nephropathic cystinosis. In this study MEA was compared to phosphocysteamine (MEAP), a phosphorothioester that tastes and smells better than MEA, with respect to its ability to elevate plasma MEA and deplete leukocytes of cystine. Studies were performed in six children with nephropathic cystinosis ranging in age from 2 to 10 yr. After equimolar oral doses of either MEA or MEAP plasma cysteamine was determined at various times for 6 h. MEA was determined by sodium borohydride reduction followed by high-performance liquid chromatography separation and electrochemical detection. Leukocyte cystine was measured before and 1 and 6 h after drug administration. Peak plasma MEA was obtained 30 min to 1 hr after a dose and was not significantly different when MEA (48.6 +/- 10.7, mean +/- SD) or MEAP (54.1 +/- 20.2) was given. Significant plasma MEA concentrations were seen as early as 15 min after an oral dose, indicating rapid absorption. Analysis of vomitus indicated that hydrolysis of the phosphate group of MEAP occurs in the stomach. The percent decrease in leukocyte cystine content obtained with MEA administration (61.9%) was not significantly different from the decrease observed when MEAP was administered (65.3%). MEA and MEAP appear to be equally effective in their cystine-depleting properties.
PMID:3393396 Smolin LA et al; Pediatr Res 23 (6): 616-20 (1988)
There is limited information in the literature regarding the metabolism of cysteamine. This drug undergoes significant first-pass metabolism.
The half-life of cysteamine is about 3.7 hours.
Individuals born without the ability to metabolize cystine suffer from cystinosis, a rare genetic disorder characterized by the widespread accumulation of cystine crystals throughout the body and eye tissues. The cystine crystals may cause considerable damage, particularly in the renal tissues and corneal tissues. In some cases, renal failure can occur during childhood if the condition is left untreated. Other organs that may be affected by cystinosis include the CNS, thyroid, pancreas, muscle tissues, and gonads. Cysteamine converts cystine to cysteine and cysteine-cysteamine mixed disulfides, reducing the buildup of corneal cystine crystals. This drug participates in a thiol-disulfide interchange reaction with lysosomes, leading to cysteine exit from the lysosome in patients diagnosed with cystinosis.
Cysteamine is an aminothiol that converts cystine to cysteine and cysteine-cysteamine mixed disulfide, both of which can pass through the lysosomal membrane of patients with cystinosis. In the nephropathic form of cystinosis, the accumulation of cystine and the formation of crystals damage various organs, especially the kidney. Cysteamine improves glomerular function without affecting tubular function.
Thomson.Micromedex. Drug Information for the Health Care Professional. 25th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2005.
ABOUT THIS PAGE


LOOKING FOR A SUPPLIER?