1. 4,5 Diphenyl 2 Oxazolepropionic Acid
2. 4,5-diphenyl-2-oxazolepropionic Acid
3. Apo Oxaprozin
4. Apo-oxaprozin
5. Danoprox
6. Daypro
7. Dayrun
8. Rhoxal Oxaprozin
9. Rhoxal-oxaprozin
10. Wy 21,743
11. Wy-21,743
1. 21256-18-8
2. Daypro
3. 3-(4,5-diphenyl-1,3-oxazol-2-yl)propanoic Acid
4. Alvo
5. 3-(4,5-diphenyloxazol-2-yl)propanoic Acid
6. Oxaprozine
7. Oxaprozinum
8. Deflam
9. Wy-21,743
10. Oxaprozine [inn-french]
11. Oxaprozinum [inn-latin]
12. Wy-21743
13. Oxaprozina [inn-spanish]
14. Oxaprozina
15. 4,5-diphenyl-2-oxazolepropanoic Acid
16. 4,5-diphenyl-2-oxazolepropionic Acid
17. 2-oxazolepropanoic Acid, 4,5-diphenyl-
18. Duraprox
19. Oxaprozinum;wy21743
20. Wy 21743
21. Mfcd00215977
22. Nsc310839
23. Nsc-310839
24. 3-(4,5-diphenyl-2-oxazolyl)propenoic Acid
25. 3-(diphenyl-1,3-oxazol-2-yl)propanoic Acid
26. Beta-(4,5-diphenyloxazol-2-yl)propionic Acid
27. Mhj80w9lrb
28. Nsc 310839
29. Chembl1071
30. Chebi:7822
31. Voir
32. 2-oxazolepropionic Acid, 4,5-diphenyl-
33. .beta.-(4,5-diphenyloxazol-2-yl)propionic Acid
34. Danoprox
35. Dayrun
36. 3-(4,5-diphenyl-2-oxazolyl)propanoic Acid
37. Cas-21256-18-8
38. Dsstox_cid_25118
39. Dsstox_rid_80684
40. Dsstox_gsid_45118
41. Actirin
42. Xopane
43. Smr000058286
44. Daypro (tn)
45. Sr-01000076053
46. Oxaprosin
47. Durapro
48. Duraprost
49. Oxaprozi
50. Oxapro
51. Walix
52. Oxaprozin, Solid
53. Oxaprozin,(s)
54. Oxaprozin- Bio-x
55. Einecs 244-296-1
56. Nci310839
57. 4, 5-diphenyl-2-oxazolepropionic Acid
58. Brn 1083168
59. Oxaprozin [inn]
60. Oxaprozin [jan]
61. Oxaprozin [mi]
62. Oxaprozin [hsdb]
63. Oxaprozin [usan]
64. Maybridge1_008800
65. Prestwick0_001060
66. Prestwick1_001060
67. Prestwick2_001060
68. Prestwick3_001060
69. Spectrum2_001696
70. Spectrum3_001078
71. Spectrum4_001231
72. Unii-mhj80w9lrb
73. Lopac-o-9637
74. Oxaprozin [vandf]
75. Oxaprozin [mart.]
76. O 9637
77. Oxaprozin [usp-rs]
78. Oxaprozin [who-dd]
79. Schembl3286
80. Ncistruc1_000799
81. Ncistruc2_000787
82. Bidd:pxr0149
83. Lopac0_000944
84. Oprea1_509470
85. Bspbio_001020
86. Bspbio_002696
87. Kbiogr_001722
88. Mls000759535
89. Mls001424072
90. Bidd:gt0438
91. Spectrum1505267
92. Spbio_001652
93. Spbio_002940
94. Oxaprozin (jp17/usp/inn)
95. Bpbio1_001122
96. Gtpl7252
97. Oxaprozin [orange Book]
98. Dtxsid1045118
99. Hms566h22
100. Hsdb 7586
101. Kbio3_001916
102. Oxaprozin [usp Monograph]
103. Hms1571c22
104. Hms1922p17
105. Hms2051l15
106. Hms2093o08
107. Hms2098c22
108. Hms3262n10
109. Hms3393l15
110. Hms3652h17
111. Hms3715c22
112. Hms3885l11
113. Pharmakon1600-01505267
114. Wy21743
115. Amy32551
116. Bcp28431
117. Hy-b0808
118. Tox21_110059
119. Tox21_500944
120. 2-oxazolepropanoic Acid,5-diphenyl-
121. 2-oxazolepropionic Acid,5-diphenyl-
122. Bdbm50002861
123. Ccg-36508
124. Ncgc00014711
125. Nsc758949
126. S4230
127. Zinc49643479
128. 4,5-diphenyloxazole-2-propanoic Acid
129. Oxaprozin 100 Microg/ml In Methanol
130. 4,5-diphenyloxazole-2-propionic Acid
131. Akos000206807
132. Oxaprozin [usan:usp:inn:ban:jan]
133. Tox21_110059_1
134. Cs-7975
135. Db00991
136. Ks-5196
137. Lp00944
138. Nc00214
139. Nsc-758949
140. Sdccgsbi-0050918.p004
141. Ncgc00014711-01
142. Ncgc00014711-02
143. Ncgc00014711-03
144. Ncgc00014711-04
145. Ncgc00014711-05
146. Ncgc00014711-06
147. Ncgc00014711-07
148. Ncgc00014711-08
149. Ncgc00014711-09
150. Ncgc00014711-10
151. Ncgc00014711-11
152. Ncgc00014711-14
153. Ncgc00014711-15
154. Ncgc00094249-01
155. Ncgc00094249-02
156. Ncgc00094249-03
157. Ncgc00094249-04
158. Ncgc00094249-05
159. Ncgc00094249-06
160. Ncgc00094249-07
161. Ncgc00261629-01
162. Oxaprozin 100 Microg/ml In Acetonitrile
163. Ac-26512
164. Bo164184
165. Nci60_002681
166. Sy050819
167. Sbi-0050918.p002
168. 3-(4,5-diphenyl-2-oxazolyl)propionic Acid
169. Ab00514024
170. B1804
171. Eu-0100944
172. Ft-0638104
173. O0377
174. Sw197319-4
175. 3-(4, 5-diphenyl-2-oxazolyl)propenoic Acid
176. En300-25629
177. 3-(4,5-diphenyl-oxazol-2-yl)-propionic Acid
178. C07356
179. D00463
180. Ab00514024_08
181. Ab00514024_09
182. 256o188
183. A815225
184. 1-aminocyclobutane-cis-1,3-dicarboxylicacid
185. J-013955
186. Q1749609
187. Sr-01000076053-1
188. Sr-01000076053-3
189. Sr-01000076053-7
190. Sr-01000076053-9
191. 3-(4,5-diphenyl-1,3-oxazol-2-yl)propanoic Acid #
192. Brd-k25394294-001-05-7
193. Brd-k25394294-001-08-1
194. Z217102860
195. Oxaprozin, United States Pharmacopeia (usp) Reference Standard
| Molecular Weight | 293.3 g/mol |
|---|---|
| Molecular Formula | C18H15NO3 |
| XLogP3 | 4.2 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 5 |
| Exact Mass | 293.10519334 g/mol |
| Monoisotopic Mass | 293.10519334 g/mol |
| Topological Polar Surface Area | 63.3 Ų |
| Heavy Atom Count | 22 |
| Formal Charge | 0 |
| Complexity | 361 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 4 | |
|---|---|
| Drug Name | Daypro |
| PubMed Health | Oxaprozin (By mouth) |
| Drug Classes | Analgesic, Antirheumatic, Central Nervous System Agent, Musculoskeletal Agent |
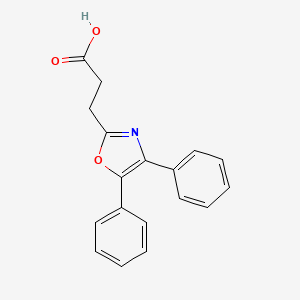
| Drug Label | DAYPRO (oxaprozin) is a nonsteroidal anti-inflammatory drug (NSAID), chemically designated as 4,5-diphenyl-2-oxazole-propionic acid, and has the following chemical structure:The empirical formula for oxaprozin is C18H15NO3, and the molecular weight i... |
| Active Ingredient | Oxaprozin |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 600mg |
| Market Status | Prescription |
| Company | Gd Searle |
| 2 of 4 | |
|---|---|
| Drug Name | Oxaprozin |
| PubMed Health | Oxaprozin (By mouth) |
| Drug Classes | Analgesic, Antirheumatic, Central Nervous System Agent, Musculoskeletal Agent |
| Drug Label | Oxaprozin, USP is a nonsteroidal anti-inflammatory drug (NSAID), chemically designated as 4,5-diphenyl-2-oxazole-propionic acid, and has the following chemical structure:The empirical formula for oxaprozin, USP is C18H15NO3, and the molecular weight... |
| Active Ingredient | Oxaprozin |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 600mg |
| Market Status | Prescription |
| Company | Teva; Apotex; Sun Pharm Inds; Sandoz; Ivax Sub Teva Pharms; Dr Reddys Labs |
| 3 of 4 | |
|---|---|
| Drug Name | Daypro |
| PubMed Health | Oxaprozin (By mouth) |
| Drug Classes | Analgesic, Antirheumatic, Central Nervous System Agent, Musculoskeletal Agent |
| Drug Label | DAYPRO (oxaprozin) is a nonsteroidal anti-inflammatory drug (NSAID), chemically designated as 4,5-diphenyl-2-oxazole-propionic acid, and has the following chemical structure:The empirical formula for oxaprozin is C18H15NO3, and the molecular weight i... |
| Active Ingredient | Oxaprozin |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 600mg |
| Market Status | Prescription |
| Company | Gd Searle |
| 4 of 4 | |
|---|---|
| Drug Name | Oxaprozin |
| PubMed Health | Oxaprozin (By mouth) |
| Drug Classes | Analgesic, Antirheumatic, Central Nervous System Agent, Musculoskeletal Agent |
| Drug Label | Oxaprozin, USP is a nonsteroidal anti-inflammatory drug (NSAID), chemically designated as 4,5-diphenyl-2-oxazole-propionic acid, and has the following chemical structure:The empirical formula for oxaprozin, USP is C18H15NO3, and the molecular weight... |
| Active Ingredient | Oxaprozin |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 600mg |
| Market Status | Prescription |
| Company | Teva; Apotex; Sun Pharm Inds; Sandoz; Ivax Sub Teva Pharms; Dr Reddys Labs |
Oxaprozin ... /is/ indicated for the treatment of acute or chronic rheumatoid arthritis. /Included in US product labeling/
Thomson/Micromedex. Drug Information for the Health Care Professional. Volume 1, Greenwood Village, CO. 2007., p. 376
Oxaprozin ... /is/ indicated for relief of acute or chronic osteoarthritis. /Included in US product labeling/
Thomson/Micromedex. Drug Information for the Health Care Professional. Volume 1, Greenwood Village, CO. 2007., p. 376
... In this open, multicenter, randomized, controlled study, eligible patients with periarthritis of the shoulder were randomized to receive either oxaprozin 1200 mg once daily (n = 49) or diclofenac 50 mg three times daily (n = 47). The treatment period was 15 +/- 1 days. The study was planned on a hypothesis of equivalence between the two study drugs. The primary study endpoint was the change from baseline at day 15 in the patient-assessed shoulder pain score. Secondary efficacy variables included investigator-assessed shoulder function, patient-assessed quality of life on the Short-Form-36 (SF-36) Acute Health Survey and both patients' and investigators' overall assessment of efficacy. At day 15, the mean changes in shoulder pain score from baseline in the oxaprozin and diclofenac groups were -5.85 +/- SD 4.62 and -5.54 +/- SD 4.41, respectively. The difference between the two groups was not statistically significant, confirming the hypothesis of the study that oxaprozin is as effective as diclofenac. Investigator-assessed shoulder function improved in both groups but more so in the oxaprozin group (p = 0.028 at day 15). Quality of life as measured by SF-36 total score was also improved in both treatment groups, with a trend toward greater improvement in the oxaprozin group. Furthermore, a significantly more favorable effect on the SF-36 'mental health' item was observed in oxaprozin compared with diclofenac-treated patients at day 15 (p = 0.0202). As assessed by investigators, the overall efficacy of oxaprozin was superior to that for diclofenac at visit 3 (8 +/- 1 days) (p = 0.0067). Patients also assessed the overall efficacy of oxaprozin as superior to that of diclofenac at visits 3 (8 +/- 1 days) (p = 0.0235) and 4 (15 +/- 1 days) (p = 0.0272). Only six adverse events, all of which were mild or moderate in intensity and occurred in four diclofenac recipients, were observed in the study. As expected, once-daily oxaprozin proved to be as effective as diclofenac three times daily in reducing the primary efficacy variable of patient-assessed shoulder pain score in patients with periarthritis of the shoulder refractory to previous treatments with other NSAIDs. Oxaprozin was shown to be superior to diclofenac in improving shoulder function and was considered by investigators and patients to have greater overall efficacy than diclofenac. In addition, oxaprozin showed a trend toward superior results in improving patients' quality of life compared with diclofenac. A trend towards better tolerability results for oxaprozin compared with diclofenac was also noted.
PMID:15324531 Heller B, Tarricone R; Curr Med Res Opin 20 (8): 1279-90 (2004)
/EXPL THER/: The effects of eye drops containing a propionic acid derivative (oxaprozin) at 0.1% concentration on ocular inflammation produced by sodium arachidonate in the rabbit's eye were evaluated. Furthermore, the aqueous bioavailability of the drug formulation in the uninflamed and inflamed eyes was evaluated. Oxaprozin eye drops significantly reduced the signs of ocular inflammation elicited by sodium arachidonate on conjunctiva and iris. Oxaprozin treatment significantly reduced the levels of polymorphonuclear leukocytes and protein concentration in aqueous samples obtained from the eyes treated with arachidonate. Present data suggest, for the first time, that oxaprozin may be employed topically to prevent ocular reactions where the arachidonic acid cascade is activated.
PMID:11858617 Bucolo C, Maltese A; J Ocul Pharmacol Ther 18 (1): 75-81 (2002)
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. To minimize the potential risk for an adverse cardiovascular event in patients treated with a NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous cardiovascular symptoms. Patients should be informed about the signs and/or symptoms of serious cardiovascular events and the steps to take if they occur. /Nonsteroidal anti-inflammatory drugs/
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
NSAIDs, including Daypro, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3-6 months, and in about 2-4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
NSAIDs should be prescribed with extreme caution in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients treated with neither of these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population. To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulcerations and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI event is suspected. This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high risk patients, alternate therapies that do not involve NSAIDs should be considered. /Nonsteroidal anti-inflammatory drugs/
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
As with other NSAIDs, anaphylactoid reactions may occur in patients without known prior exposure to Daypro. Daypro should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
For more Drug Warnings (Complete) data for OXAPROZIN (18 total), please visit the HSDB record page.
Used to relieve the inflammation, swelling, stiffness, and joint pain associated with rheumatoid arthritis and osteoarthritis.
FDA Label
Oxaprozin is a nonsteroidal anti-inflammatory drug (NSAID) with analgesic and antipyretic properties. Oxaprozin is used to treat rheumatoid arthritis, osteoarthritis, dysmenorrhea, and to alleviate moderate pain.
Anti-Inflammatory Agents, Non-Steroidal
Anti-inflammatory agents that are non-steroidal in nature. In addition to anti-inflammatory actions, they have analgesic, antipyretic, and platelet-inhibitory actions. They act by blocking the synthesis of prostaglandins by inhibiting cyclooxygenase, which converts arachidonic acid to cyclic endoperoxides, precursors of prostaglandins. Inhibition of prostaglandin synthesis accounts for their analgesic, antipyretic, and platelet-inhibitory actions; other mechanisms may contribute to their anti-inflammatory effects. (See all compounds classified as Anti-Inflammatory Agents, Non-Steroidal.)
Cyclooxygenase Inhibitors
Compounds or agents that combine with cyclooxygenase (PROSTAGLANDIN-ENDOPEROXIDE SYNTHASES) and thereby prevent its substrate-enzyme combination with arachidonic acid and the formation of eicosanoids, prostaglandins, and thromboxanes. (See all compounds classified as Cyclooxygenase Inhibitors.)
M - Musculo-skeletal system
M01 - Antiinflammatory and antirheumatic products
M01A - Antiinflammatory and antirheumatic products, non-steroids
M01AE - Propionic acid derivatives
M01AE12 - Oxaprozin
Absorption
Oxaprozin is 95% absorbed after oral administration. Food may reduce the rate of absorption of oxaprozin, but the extent of absorption is unchanged. Antacids do not significantly affect the extent and rate of oxaprozin absorption.
Route of Elimination
Oxaprozin is expected to be excreted in human milk based on its physical-chemical properties; however, the amount of oxaprozin excreted in breast milk has not been evaluated. Approximately 95% of oxaprozin is metabolized by the liver. Approximately 5% of the oxaprozin dose is excreted unchanged in the urine. Sixty-five percent (65%) of the dose is excreted in the urine and 35% in the feces as metabolite. Biliary excretion of unchanged oxaprozin is a minor pathway. Several oxaprozin metabolites have been identified in human urine or feces.
Volume of Distribution
11 to 17 L/70 kg
In dose proportionality studies utilizing 600, 1200 and 1800 mg doses, the pharmacokinetics of oxaprozin in healthy subjects demonstrated nonlinear kinetics of both the total and unbound drug in opposite directions, i.e., dose exposure related increase in the clearance of total drug and decrease in the clearance of the unbound drug. Decreased clearance of the unbound drug was related predominantly to a decrease in the volume of distribution and not an increase in the half-life. This phenomenon is considered to have minimal impact on drug accumulation upon multiple dosing. The apparent volume of distribution (Vd/F) of total oxaprozin is approximately 11-17 L/70 kg. Oxaprozin is 99% bound to plasma proteins, primarily to albumin. At therapeutic drug concentrations, the plasma protein binding of oxaprozin is saturable, resulting in a higher proportion of the free drug as the total drug concentration is increased. With increases in single doses or following repetitive once-daily dosing, the apparent volume of distribution and clearance of total drug increased, while that of unbound drug decreased due to the effects of nonlinear protein binding. Oxaprozin penetrates into synovial tissues of rheumatoid arthritis patients with oxaprozin concentrations 2-fold and 3-fold greater than in plasma and synovial fluid, respectively. Oxaprozin is expected to be excreted in human milk based on its physical-chemical properties; however, the amount of oxaprozin excreted in breast milk has not been evaluated.
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
Daypro is 95% absorbed after oral administration. Food may reduce the rate of absorption of oxaprozin, but the extent of absorption is unchanged. Antacids do not significantly affect the extent and rate of Daypro absorption.
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
It is not known whether oxaprozin is distributed into human breast milk. However, it is distributed into the milk of lactating rats.
Thomson/Micromedex. Drug Information for the Health Care Professional. Volume 1, Greenwood Village, CO. 2007., p. 382
Approximately 5% of the oxaprozin dose is excreted unchanged in the urine. Sixty-five percent (65%) of the dose is excreted in the urine and 35% in the feces as metabolite. Biliary excretion of unchanged oxaprozin is a minor pathway, and enterohepatic recycling of oxaprozin is insignificant. Upon chronic dosing the accumulation half-life is approximately 22 hours. The elimination half-life is approximately twice the accumulation half-life due to increased binding and decreased clearance at lower concentrations.
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
For more Absorption, Distribution and Excretion (Complete) data for OXAPROZIN (8 total), please visit the HSDB record page.
Hepatic. Ester and ether glucuronide are the major conjugated metabolites of oxaprozin, and do not have significant pharmacologic activity.
Several oxaprozin metabolites have been identified in human urine or feces. Oxaprozin is primarily metabolized by the liver, by both microsomal oxidation (65%) and glucuronic acid conjugation (35%). Ester and ether glucuronide are the major conjugated metabolites of oxaprozin. On chronic dosing, metabolites do not accumulate in the plasma of patients with normal renal function. Concentrations of the metabolites in plasma are very low. Oxaprozin's metabolites do not have significant pharmacologic activity. The major ester and ether glucuronide conjugated metabolites have been evaluated along with oxaprozin in receptor binding studies and in vivo animal models and have demonstrated no activity. A small amount (<5%) of active phenolic metabolites are produced, but the contribution to overall activity is limited.
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
54.9 hours
Upon chronic dosing the accumulation half-life is approximately 22 hours. The elimination half-life is approximately twice the accumulation half-life due to increased binding and decreased clearance at lower concentrations.
Prescribing Information for Daypro (Oxaprozin); G.D. Searle LLC, Div. of Pfizer Inc, USA; (January 2007). Available from, as of February 12, 2008: https://media.pfizer.com/files/products/uspi_daypro.pdf
Anti-inflammatory effects of Oxaprozin are believed to be due to inhibition of cylooxygenase in platelets which leads to the blockage of prostaglandin synthesis. Antipyretic effects may be due to action on the hypothalamus, resulting in an increased peripheral blood flow, vasodilation, and subsequent heat dissipation. Oxaprozin is a non-selective NSAID, with a cell assay system showing lower COX-2 selectivity implying higher COX-1 selectivity.
This study was undertaken to evaluate the scavenging activity for reactive oxygen species (ROS) and reactive nitrogen species (RNS) by several nonsteroidal anti-inflammatory drugs (NSAIDs), namely indole derivatives (indomethacin, acemetacin, etodolac), pyrrole derivatives (tolmetin and ketorolac), and an oxazole derivative (oxaprozin). The inhibition of prostaglandin synthesis constitutes the primary mechanism of the anti-inflammatory action of these drugs. Nevertheless, it has been suggested that the anti-inflammatory activity of NSAIDs may be also partly due to their ability to scavenge ROS and RNS and to inhibit the respiratory burst of neutrophils triggered by various activator agents. Thus, the scavenging activity of these NSAIDs was evaluated against an array of ROS (O(2)(-), HO, HOCl, and ROO) and RNS (NO and ONOO(-)) using noncellular in vitro systems. The results obtained demonstrated that tolmetin, ketorolac, and oxaprozin were not active against O(2)(-), while acemetacin, indomethacin, and etodolac exhibited concentration-dependent effects. Oxaprozin was also the least active scavenger for HO, among all the tested NSAIDs shown to be active. The scavenging effect for HOCl was not observed for any of the tested NSAIDs. The ROO was effectively scavenged by etodolac, with the other tested NSAIDs being much less active. NO and ONOO(-) were scavenged by all the tested NSAIDs.
PMID:15528048 Fernandes E et al; Free Radic Biol Med 37 (11): 1895-905 (2004)
Oxaprozin is a nonsteroidal anti-inflammatory drug characterised by a propionic acid-based structure. It is able to diffuse easily into inflamed synovial tissues after oral administration. Although discovered > 20 years ago, it is now under intensive investigation because of its unusual pharmacodynamic properties. Other than being a nonselective cyclooxygenase inhibitor, the drug is capable of inhibiting both anandamide hydrolase in neurons (median inhibitory concentration [IC50] = 85 umol/L), with consequent potent analgesic activity, and NF-kappaB activation in inflammatory cells (IC50 = 50 umol/L). Moreover, oxaprozin induces apoptosis of activated monocytes in a dose-dependent manner, with the effect being detectable at a concentration of 5 micromol/L and reaching the maximum activity at 50 umol/L. As monocyte-macrophages and NF-kappaB pathways are crucial for synthesis of proinflammatory and histotoxic mediators in inflamed joints, oxaprozin appears to be endowed with pharmacodynamic properties exceeding those presently assumed as markers of classical nonsteroidal anti-inflammatory drug.
PMID:15934904 Dallegri F et al; Expert Opin Pharmacother 6 (5): 777-85 (2005)