1. 5 L Isoleucine Angiotensin Ii
2. 5-l-isoleucine Angiotensin Ii
3. Ang-(1-8)octapeptide
4. Angiotensin Ii, 5-l-isoleucine
5. Angiotensin Ii, Ile(5)-
6. Angiotensin Ii, Isoleucine(5)-
7. Angiotensin Ii, Val(5)-
8. Angiotensin Ii, Valine(5)-
9. Angiotensin-(1-8) Octapeptide
10. Isoleucine(5)-angiotensin
11. Isoleucyl(5)-angiotensin Ii
12. Valyl(5)-angiotensin Ii
1. 4474-91-3
2. Angiotensin Ii Human
3. Hypertensin
4. Human Angiotensin Ii
5. Angiotensin Ii (human)
6. Ang Ii
7. Giapreza
8. 5-l-isoleucineangiotensin Ii
9. Angiotensin Ii (mouse)
10. 5-isoleucine-angiotensin Ii
11. Asp-arg-val-tyr-ile-his-pro-phe
12. Drvyihpf
13. 1-8-angiotensin I
14. Angiotensin Ii, Human
15. Ile(5)-angiotensin Ii
16. Isoleucine5-angiotensin Ii
17. Chebi:2719
18. Ang-(1-8)octapeptide
19. Isoleucine(5)-angiotensin Ii
20. Chembl408403
21. 1-l-aspasaginyl-5-l-valyl Angiotensin Octapeptide
22. 11128-99-7
23. Delivert
24. Angiotensin Ii (usan)
25. L-alpha-aspartyl-l-arginyl-l-valyl-l-tyrosyl-l-isoleucyl-l-histidyl-l-prolyl-l-phenylalanine
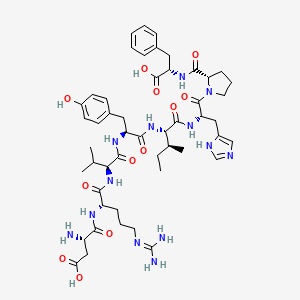
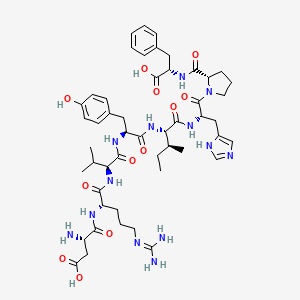
26. (2s,5s,8s,11s,14s,17s)-2-((1h-imidazol-5-yl)methyl)-17-amino-5-((s)-sec-butyl)-1-((s)-2-(((s)-1-carboxy-2-phenylethyl)carbamoyl)pyrrolidin-1-yl)-14-(3-((diaminomethylene)amino)propyl)-8-(4-hydroxybenzyl)-11-isopropyl-1,4,7,10,13,16-hexaoxo-3,6,9,12,15-pentaazanonadecan-19-oic Acid
27. N-(1-(n-(n-(n-(n-(n(2)-l-alpha-aspartyl-l-arginyl)-l-valyl)-l-tyrosyl)-l-isoleucyl)-l-histidyl)-l-prolyl)-l-phenylalanine
28. Angiotensinii,human
29. Ile5-angiotensin Ii
30. Angiotensin Ii, Ile(5)-
31. Angiotensin Ii [inn:jan]
32. Unii-m089efu921
33. Hypertensin Ii
34. Angiotensin 2
35. Angiotensin Ii, 5-l-isoleucine-
36. Delivert (tn)
37. C50h71n13o12
38. Angiotensin Ii Heavy
39. Angiotensin Ii (rat)
40. Angiotensin Ii (9ci)
41. Angiotensin Ii-human
42. Angiotensin Ii Acetate Salt
43. Schembl1189
44. Angiotensin Ii (human Type)
45. Gtpl2504
46. Ljpc-501
47. Schembl9013957
48. Schembl20502357
49. Dtxsid30196288
50. Chebi:131170
51. Ty-10721
52. M089efu921
53. Angiotensin Ii (human Type) (jan)
54. Bdbm50228195
55. Bdbm50236697
56. Akos016010178
57. Zinc169676920
58. Db11842
59. H-asp-arg-val-tyr-ile-his-pro-phe-oh
60. Ncgc00167130-01
61. Hy-13948
62. L-phenylalanine, N-(1-(n-(n-(n-(n-(n2-l-alpha-aspartyl-l-arginyl)-l-valyl)-l-tyrosyl)-l-isoleucyl)-l-histidyl)-l-prolyl)-
63. Asp1-arg2-val3-tyr4-ile5-his6-pro7-phe8
64. C02135
65. C75211
66. D02014
67. Drvy-i*-hpf [i*= I(13c6,15n)]
68. A872469
69. Q412999
70. Ang-(1-8)octapeptide, Hypertensin, 4474-91-3, Giapreza
71. Conalbumin (328-332), 1226776-54-0, Rvpsl Peptide
72. Proteomass(tm) Angiotensin Ii Maldi-ms Standard, Vial Of 10 Nmol
73. (3s)-3-amino-3-{[(1s)-1-{[(1s)-1-{[(1s)-1-{[(1s,2s)-1-{[(2s)-1-[(2s)-2-{[(1s)-1-carboxy-2-phenylethyl]carbamoyl}pyrrolidin-1-yl]-3-(1h-imidazol-5-yl)-1-oxopropan-2-yl]carbamoyl}-2-methylbutyl]carbamoyl}-2-(4-hydroxyphenyl)ethyl]carbamoyl}-2-methylpropyl]carbamoyl}-4-[(diaminomethylidene)amino]butyl]carbamoyl}propanoic Acid
74. Alanine, N-(1-(n-(n-(n-(n-(n2-l-alpha-aspartyl-l-arginyl)-l-valyl)-l-tyrosyl)-l-isoleucyl)-l-histidyl)-l-prolyl)-3-phenyl-, L-
75. L-phenylalanine, L-alpha-aspartyl-l-arginyl-l-valyl-l-tyrosyl-l-isoleucyl-l-histidyl-l-prolyl-
| Molecular Weight | 1046.2 g/mol |
|---|---|
| Molecular Formula | C50H71N13O12 |
| XLogP3 | -1.7 |
| Hydrogen Bond Donor Count | 13 |
| Hydrogen Bond Acceptor Count | 15 |
| Rotatable Bond Count | 29 |
| Exact Mass | 1045.53451475 g/mol |
| Monoisotopic Mass | 1045.53451475 g/mol |
| Topological Polar Surface Area | 409 Ų |
| Heavy Atom Count | 75 |
| Formal Charge | 0 |
| Complexity | 1980 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 9 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Angiotensin II is a vasoconstrictor indicated for increasing blood pressure in adults with septic or other distributive shock.
FDA Label
Giapreza is indicated for the treatment of refractory hypotension in adults with septic or other distributive shock who remain hypotensive despite adequate volume restitution and application of catecholamines and other available vasopressor therapies.
Angiotensin II is a naturally occurring peptide hormone of the renin-angiotensin-aldosterone-system (RAAS) that has the capacity to cause vasoconstriction and an increase in blood pressure in the human body. In the RAAS, juxtaglomerular cells of the renal afferent arteriole synthesize the proteolytic enzyme renin. Although stored in an inactive form called pro-renin, decreases in arterial blood pressure or extracellular fluid volume depletion can cause various enzymatic reactions to release active renin into the systemic circulation and surrounding tissues. Such renin release allows for the production of the alpha-2-globulin angiotensinogen predominantly in the liver and to some extent, the kidneys and other organs. Angiotensin I, itself a decapeptide with weak biological activity, is produced from angiotensinogen and then quickly converted to angiotensin II by angiotensin converting enzymes (ACE). Consequently, angiotensin II demonstrates its strong vasopressor activity when it is rapidly degraded by aminopeptidases A and M into further entities like angiotensin III and angiotensin IV, respectively. Such species like angiotensin III can then bind and interact with specific G protein coupled receptors like angiotensin receptor 1, or AT-1 where strong vasoconstricson can occur. Furthermore, in the ATHOS-3 clinical trial, for the 114 (70%) patient subjects in the angiotensin II arm who reached the target mean arterial pressure (MAP) at Hour 3, the median time to reach the target MAP endpoint was approximately 5 minutes. The angiotensin II was titrated to effect for each individual patient..
Vasoconstrictor Agents
Drugs used to cause constriction of the blood vessels. (See all compounds classified as Vasoconstrictor Agents.)
C09
C - Cardiovascular system
C01 - Cardiac therapy
C01C - Cardiac stimulants excl. cardiac glycosides
C01CX - Other cardiac stimulants
C01CX09 - Angiotensin II
Absorption
Following the intravenous infusion of angiotensin II in adult patients with septic or other distributive shock, the serum levels of angiotensin II observed were similar at baseline and hour 3 after the intravenous infusion. After 3 hours of treatment, the serum level of angiotensin I (the angiotensin II precursos peptide) is however, reduced by about 40%.
Route of Elimination
The official prescribing information notes that no specific studies have been conducted that examine the elimination of angiotensin II.
Volume of Distribution
The official prescribing information for angiotensin II notes that no specific studies have yet been conducted that examine the distribution of angiotensin II.
Clearance
The official prescribing information notes that the clearnace of angiotensin II is not dependent on hepatic function or renal function.
It is metabolized by aminopeptidase A and angiotensin converting enzyme 2 to angiotensin-(2-8) [angiotensin III] and angiotensin-(1-7), respectively in plasma, erythrocytes and many of the major organs (i.e. intestine, kidney, liver and lung). Angiotensin II type 1 receptor (AT1) mediated activity of angiotensin III is approximately 40% of angiotensin II; however, aldosterone synthesis activity is similar to angiotensin II. Angiotensin-(1-7) exerts the opposite effects of angiotensin II on AT1 receptors and causes vasodilation. Nevertheless, the official prescribing information also notes that no formal studies have been conducted that examine the metabolism of angiotensin II.
The plasma half-life of intravenously administered angiotensin II is less than one minute.
As part of the renin-angiotensin-aldosterone-system (RAAS), angiotensin II raises blood pressure by vasoconstriction, increased aldosterone release by the adrenal zona glomerulosa, sodium and water reabsorption in the proximal tubular cells, and vasopressin secretion The direct action of angiotensin II on surrounding vessel walls is facilitated by binding to the G-protein-coupled angiotensin II receptor type 1 (AT-1) on vascular smooth muscle cells, which stimulates Ca2+/calmodulin-dependent phosphorylation of myosin and causes smooth muscle contraction that results in vasoconstriction. The RAAS is ultimately regulated by a negative feedback effect of angiotensin II on renin production by the juxtaglomerular cells of the renal afferent arteriole. Unresuscitated septic shock associated with marked hypovolemia, extracellular fluid volume depletion, decreased cardiac output, low arterial blood pressure and decreased systemic vascular resistance causes an increase in renin secretion by the juxtaglomerular cells, resulting in elevated angiotensin II plasma levels and an increased secretion of aldosterone from the adrenal cortex. Angiotensin II binding to AT-1 receptors causes dose-dependent vasoconstriction of both afferent and efferent glomerular arterioles. The most pronounced effect of angiotensin II results on efferent arterioles, resulting in reduced renal blood flow and increased glomerular filtration pressure.