1. Cantharides
2. Cantharidine
1. 56-25-7
2. Cantharidine
3. Cantharone
4. Kantaridin
5. Cantharides Camphor
6. Kantharidin
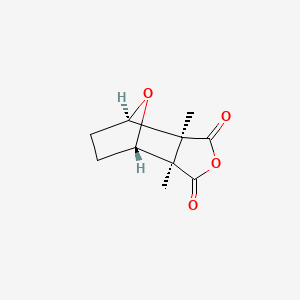
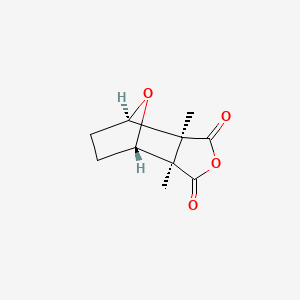
7. 1,2-dimethyl-3,6-epoxyperhydrophthalic Anhydride
8. Cantaridina
9. Cantharidinum
10. Exo-1,2-cis-dimethyl-3,6-epoxyhexahydrophthalic Anhydride
11. Hexahydro-3a,7a-dimethyl-4,7-epoxyisobenzofuran-1,3-dione
12. Nsc61805
13. Brn 0085302
14. Cantharidin [usan]
15. Ai3-04021
16. (3ar,4s,7r,7as)-3a,7a-dimethylhexahydro-4,7-epoxy-2-benzofuran-1,3-dione
17. Nsc-61805
18. Igl471wq8p
19. Chembl48449
20. 4,7-epoxyisobenzofuran-1,3-dione, Hexahydro-3a,7a-dimethyl-, (3ar,4s,7r,7as)-rel-
21. Chebi:64213
22. 2,3-dimethyl-7-oxabicyclo(2.2.1)heptane-2,3-dicarboxylic Anhydride
23. Can [alkaloid]
24. Mfcd00134968
25. Cantharidin (usan)
26. Nsc 61805
27. Kantharidin [german]
28. Caswell No. 157
29. (3a?,4?,7?,7a?)-hexahydro-3a,7a-dimethyl-4,7-epoxyisobenzofuran-1,3-dione
30. 4,7-epoxyisobenzofuran-1,3-dione, Hexahydro-3a,7a-dimethyl-,(3ar,4s,7r,7as)-rel-
31. Ccris 635
32. 4,7-epoxyisobenzofuran-1,3-dione, Hexahydro-3a,7a-dimethyl-
33. 7-oxabicyclo(2.2.1)heptane-2,3-dicarboxylic Anhydride, 2,3-dimethyl-
34. Hsdb 2181
35. Einecs 200-263-3
36. Unii-igl471wq8p
37. Epa Pesticide Chemical Code 013101
38. 7a-dimethylhexahydro-3a,4,7-epoxyisobenzofuran
39. Cas-56-25-7
40. Ncgc00016247-01
41. 3a,7a-dimethylhexahydro-4,7-epoxyisobenzofuran-1,3-dione
42. Cantharidin [mi]
43. Prestwick3_000885
44. Cantharidin [inn]
45. Cantharidin [iarc]
46. (1r,2s,3r,6s)-1,2-dimethyl-3,6-epoxycyclohexane-1,2-dicarboxylic Anhydride
47. 2,3-dicarboxylic Anhydride
48. Cantharidin [vandf]
49. Cantharidine [hsdb]
50. Hexahydro-3aalpha,7aalpha-dimethyl-4beta,7beta-epoxyisobenzofuran-1,3-dione
51. Ncimech_000301
52. Cantharidin [mart.]
53. Cantharidinum [hpus]
54. Bspbio_000670
55. Cantharidin [who-dd]
56. 4,7-epoxyisobenzofuran-1,3-dione, Hexahydro-3a,7a-dimethyl-, (3a-alpha,4-beta,7-beta,7a-alpha)
57. 5-19-05-00051 (beilstein Handbook Reference)
58. Schembl152262
59. Bpbio1_000738
60. Cantharides Camphor, Cantharone
61. Cid_6708701
62. Hms2097b12
63. Hms3412j13
64. Hms3676j13
65. 1,6-epoxyperhydrophthalic Anhydride
66. 4,7-epoxyisobenzofuran-1,3-dione, Hexahydro-3a,7a-dimethyl-, (3a.alpha.,4.beta.,7.beta.,7a.alpha.)-
67. Act03236
68. Amy33451
69. Bcp09819
70. Hy-n0209
71. Bdbm50090505
72. Ccg-35382
73. Ccg-36082
74. Who 11470
75. Zinc17611186
76. Akos015895930
77. Ac-7967
78. Cs-4979
79. Db12328
80. 4,3-dione, Hexahydro-3a,7a-dimethyl-
81. Exo-1,6-epoxyhexahydrophthalic Anhydride
82. Ncgc00025212-02
83. Ncgc00025212-03
84. Ncgc00025212-04
85. Ncgc00025212-05
86. Ncgc00025212-31
87. As-18735
88. Nci60_005413
89. Wln: T C555 A Ao Dvovtj C1 G1
90. Ab00513946
91. Hexahydro-3a,7-epoxyisobenzofuran-1,3-dione
92. D11745
93. 7-oxabicyclo[2.2.1]heptane-2, 2,3-dimethyl-
94. 134c968
95. Q410884
96. Sr-01000597585
97. Sr-01000597585-1
98. Brd-k80684056-001-01-0
99. Hexahydro-3a,7a-dimethyl-4,7-epoxyisobenzo-furan-1,3-dione
100. (3ar,4s,7r,7as)-3a,7a-dimethylhexahydro-4,7-epoxyisobenzofuran-1,3-dione
101. (1r,2s,6r,7s)-2,6-dimethyl-4,10-dioxa-tricyclo[5.2.1.0*2,6*]decane-3,5-dione
102. (1r,5s,6r,9s)-rel-1,5-dimethyl-3,10-dioxatricyclo(3.2.1.01,5)decane-2,4-dione
103. (1r,7s)-2,6-dimethyl-4,10-dioxa-tricyclo[5.2.1.0*2,6*]decane-3,5-dione
104. (1s,2r,6s,7r)-2,6-dimethyl-4,10-dioxa-tricyclo[5.2.1.0*2,6*]decane-3,5-dione
105. (1s,2r,6s,7r)-2,6-dimethyl-4,10-dioxatricyclo[5.2.1.02,6]decane-3,5-dione
106. (1s,3s,4r,7r)-2,6-dimethyl-4,10-dioxa-tricyclo[5.2.1.0-2,6]decane-3,5-dione
107. 4,3-dione, Hexahydro-3a,7a-dimethyl-, (3a.alpha.,4.beta.,7.beta.,7a.alpha.)-
108. Cantharidin:4,7-epoxyisobenzofuran-1,3-dione,hexahydro-3a,7a- Dimethyl-, (3a,4,7,7a)-,
109. Hexahydro-3a.alpha.,7a.alpha.-dimethyl-4.beta.,7.beta.-epoxyisobenzofuran-1,3-dione
| Molecular Weight | 196.20 g/mol |
|---|---|
| Molecular Formula | C10H12O4 |
| XLogP3 | 0.6 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 0 |
| Exact Mass | 196.07355886 g/mol |
| Monoisotopic Mass | 196.07355886 g/mol |
| Topological Polar Surface Area | 52.6 Ų |
| Heavy Atom Count | 14 |
| Formal Charge | 0 |
| Complexity | 318 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 4 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Enzyme Inhibitors; Irritants
National Library of Medicine's Medical Subject Headings online file (MeSH, 1999)
EXPTL USE: CANTHARIDIN AS ANTICANCER AGENTS.
PMID:7246474 HSU B; AM J CHIN MED 8 (4): 301 (1980)
EXPTL USE: APPLICATION OF MYLABRIS CANTHARIDIN IS AN ACTIVE COMPONENT OF MYLABRIS IN CANCER TREATMENT.
WANG K; YAO HSUEH T'UNG PAO 15 (3): 23 (1980)
EXPTL USE: IN MICE INOCULATED WITH 2 MILLION CELLS OF ASCITES HEPATOMA, ADMIN OF CANTHARIDIN (1.25 MG/KG/DAY FOR 7 DAYS, IP) PROLONGED SURVIVAL PERIOD BY 20.8-61.5%. CANTHARIDIN HAD NO THERAPEUTIC ACTION ON SARCOMA 180 IN MICE OR WALKER TUMOR IN RATS.
CHEN R ET AL; CHIN MED J (PEKING, ENGL ED) 93 (3): 183 (1980)
For more Therapeutic Uses (Complete) data for CANTHARIDINE (9 total), please visit the HSDB record page.
The only therapeutic use for which cantharidin is currently primarily indicated for is as an active ingredient in topical agents for treating common warts (verruca vulgaris), periungual warts, plantar warts, and molluscum contagiosum. At the same time, such topical cantharidin applications have also been used for a number of off-label indications like callus removal, cutaneous leishmaniasis, herpes zoster, and acquired perforating dermatosis. Furthermore, since most topical cantharidin applications are most commonly available in a 0.7% formulation or a more potent 1% mixture, the 0.7% formulation is most commonly indicated for the treatment of common warts, periungual warts, and molluscum contagiosum while the more potent 1% mixture is typically limited only for use by healthcare professionals in a clinical setting for treating plantar warts and other more specialized off-label conditions. Moreover, there have also been studies into whether or not cantharidin could be effective at being used as an inflammatory model or in cancer treatment - either of which has yet to formally elucidate any results.
Cantharidin is a natural toxin produced by the blistering beetle that possesses both vesicant (blistering) and keratolytic effects. The substance elicits these effects by inducing acantholysis (loss of intercellular connections) through the targeting of the desmosomal dense plaque, resulting in the detachment of the desmosomes from the tonofilaments. Cantharidin's effectiveness against warts is proposed to be a result of the exfoliation of the wart body as a consequence of the compound's acantholytic action. This acantholytic action generally does not go beyond the epidermal cells so that the basal layer remains intact and minimal effect occurs on the corium. There is consequently no scarring from the topical application of cantharidin.
Irritants
Drugs that act locally on cutaneous or mucosal surfaces to produce inflammation; those that cause redness due to hyperemia are rubefacients; those that raise blisters are vesicants and those that penetrate sebaceous glands and cause abscesses are pustulants; tear gases and mustard gases are also irritants. (See all compounds classified as Irritants.)
Enzyme Inhibitors
Compounds or agents that combine with an enzyme in such a manner as to prevent the normal substrate-enzyme combination and the catalytic reaction. (See all compounds classified as Enzyme Inhibitors.)
Absorption
Cantharidin is absorbed from the gastrointestinal tract, and, to a limited extent from the skin as well. Little pharmacodynamic and pharmacokinetic data regarding cantharidin in the human body currently exists; recruitment for First-Time-In-Human clinical trials regarding such information have been ongoing in 2018. There are however some studies regarding such data in animal models like beagle dogs.
Route of Elimination
It has been observed that absorbed cantharidin is excreted by the kidney. Little pharmacodynamic and pharmacokinetic data regarding cantharidin in the human body currently exists; recruitment for First-Time-In-Human clinical trials regarding such information have been ongoing in 2018. There are however some studies regarding such data in animal models like beagle dogs.
Volume of Distribution
After oral or IP injection of (3)H-labeled cantharidin, high levels of radioactivity distributed to and were exhibited in the bile, kidney, liver, stomach, and tumor cells of ascites hepatoma-bearing mice. Such distribution suggests the agent has an affinity for liver and tumor tissues. Little pharmacodynamic and pharmacokinetic data regarding cantharidin in the human body currently exists; recruitment for First-Time-In-Human clinical trials regarding such information have been ongoing in 2018. There are however some studies regarding such data in animal models like beagle dogs.
Clearance
Little pharmacodynamic and pharmacokinetic data regarding cantharidin in the human body currently exists; recruitment for First-Time-In-Human clinical trials regarding such information have been ongoing in 2018. There are however some studies regarding such data in animal models like beagle dogs.
THE DRUG IS ABSORBED FROM GI TRACT AND, TO LIMITED EXTENT, FROM SKIN. IT IS EXCRETED BY KIDNEY.
Goodman, L.S., and A. Gilman. (eds.) The Pharmacological Basis of Therapeutics. 5th ed. New York: Macmillan Publishing Co., Inc., 1975., p. 952
BILE, KIDNEY, LIVER, STOMACH & TUMOR CELLS OF ASCITES HEPATOMA-BEARING MICE EXHIBITED A HIGH LEVEL OF RADIOACTIVITY AFTER ORAL OR IP INJECTION OF (3)H-LABELED CANTHARIDIN. DISTRIBUTION SUGGESTS IT HAS AFFINITY TO LIVER & TUMOR TISSUES.
CHEN R ET AL; CHIN MED J (PEKING, ENGL ED) 93 (3): 183 (1980)
Little pharmacodynamic and pharmacokinetic data regarding cantharidin in the human body currently exists; recruitment for First-Time-In-Human clinical trials regarding such information have been ongoing in 2018. There are however some studies regarding such data in animal models like beagle dogs.
Little pharmacodynamic and pharmacokinetic data regarding cantharidin in the human body currently exists; recruitment for First-Time-In-Human clinical trials regarding such information have been ongoing in 2018. There are however some studies regarding such data in animal models like beagle dogs.
Cantharidin is specifically absorbed by lipids in the membrane of epidermal keratinocytes, where it activates the release of neutral serine proteases. These enzymes subsequently break the peptide bonds in surrounding proteins, leading to the progressive degeneration of desmosomal dense plaques, which are important cellular structures that participate in cell-to-cell adhesion. Such degeneration results in the detachment of the tonofilaments that hold cells together. This process as a whole leads to the selective acantholysis (loss of cellular connections) and blistering of the skin when the cantharidin topical application is applied upon specific topical developments like warts. A blister(s) at the application site develop within 24 to 48 hours of application and typically resolve within 4 to 7 days. Factors that can modify this proposed time frame include the volume or concentration of cantharidin used, physical contact time of the applied compound (usually between 4 to 24 hours), the presence of any occlusive dressings, or even patient sensitivity to cantharidin. The blistered lesions ultimately heal without scarring. Finally, there are some studies that suggest cantharidin's chemical profile as a potent and selective inhibitor of protein phosphatase 2A confers upon it an oxidative stress-independent growth inhibition of pancreatic cancer cells through cancer cell-cycle arrest and apoptosis. Nevertheless, the fact that little data regarding the pharmacodynamics and pharmacokinetics of cantharidin in the human body exists and certain toxic effects of cantharidin that have been observed following oral ingestion in humans like ulceration of the gastrointestinal and genitourinary tracts, along with electrolyte and renal function disturbance are strong reasons as to why the compound currently lacks FDA approval is used fairly limitedly for formal therapeutic indications.
Cantharidine totally inhibits the phosphorylase a phosphatase activity in mouse liver, muscle, and skin cytosol at 5000 nM, with IC50s of 110-250 nM. About 50% of the phosphorylase a phosphatase activity of brain cytosol is sensitive to cantharidine with an IC50 of approximately 80 nM and the remaining half is not inhibited even at 5000 nM.
PMID:7839375 Eldridge R, Casida JE; Toxicol Appl Pharmacol 130 (1): 95-100 (1995)