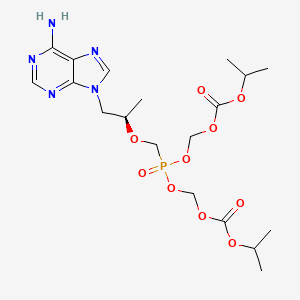
1. (r)-9-(2-phosphonylmethoxypropyl)adenine
2. 9-(2-phosphonomethoxypropyl)adenine
3. 9-(2-phosphonylmethoxypropyl)adenine
4. 9-(2-phosphonylmethoxypropyl)adenine, (+-)-isomer
5. 9-(2-phosphonylmethoxypropyl)adenine, (r)-isomer - T357098
6. 9-(2-phosphonylmethoxypropyl)adenine, (s)-isomer
7. 9-pmpa (tenofovir)
8. Disoproxil Fumarate, Tenofovir
9. Disoproxil, Tenofovir
10. Fumarate, Tenofovir Disoproxil
11. Tenofovir
12. Tenofovir Disoproxil Fumarate
13. Viread
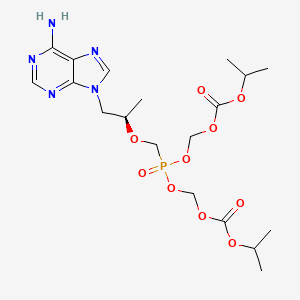
1. 201341-05-1
2. Pmpa Prodrug
3. Bis(poc)pmpa
4. 9-((r)-2-((bis(((isopropoxycarbonyl)oxy)methoxy)phosphinyl)methoxy)propyl)adenine
5. (r)-bis(poc)pmpa
6. Bis-poc-pmpa
7. Tenofovir Bis(isopropyloxycarbonyloxymethyl) Ester
8. Tenofovir Disoproxil Fumarate
9. F4yu4lon7i
10. Chebi:63717
11. [[(2r)-1-(6-aminopurin-9-yl)propan-2-yl]oxymethyl-(propan-2-yloxycarbonyloxymethoxy)phosphoryl]oxymethyl Propan-2-yl Carbonate
12. Gs-4331
13. Tenofovirdisoproxil
14. Bis({[(propan-2-yloxy)carbonyl]oxy}methyl) ({[(2r)-1-(6-amino-9h-purin-9-yl)propan-2-yl]oxy}methyl)phosphonate
15. Unii-f4yu4lon7i
16. 9-[(r)-2-[[bis[[(isopropoxycarbonyl)oxy]methoxy]phosphinyl]methoxy]propyl]adenine
17. Tenofovir-disoproxil
18. 2,4,6,8-tetraoxa-5-phosphanonanedioic Acid, 5-(((1r)-2-(6-amino-9h-purin-9-yl)-1-methylethoxy)methyl)-, 1,9-bis(1-methylethyl) Ester, 5-oxide
19. 2,4,6,8-tetraoxa-5-phosphanonanedioic Acid, 5-[[(1r)-2-(6-amino-9h-purin-9-yl)-1-methylethoxy]methyl]-, 1,9-bis(1-methylethyl) Ester, 5-oxide
20. Tenofovir (disoproxil)
21. Chembl1538
22. Schembl52793
23. Mls006010919
24. Dtxsid5052757
25. Bdbm77145
26. Bis(poc)-pmpa;gs 4331
27. Bis(isopropyloxymethylcarbonyl)pmpa
28. Amy11134
29. Zinc3929022
30. Hy-13782a
31. Mfcd00952920
32. S5959
33. Tenofovir Disoproxil [who-dd]
34. Akos015895093
35. Viread(tm) (*1:1 Fumarate Salt*)
36. Cs-5922
37. Db00300
38. Tenofovir Disoproxil [ema Epar]
39. Ncgc00183876-02
40. Tenofovir Disoproxil (gs 4331)
41. [[(1r)-2-(6-aminopurin-9-yl)-1-methyl-ethoxy]methyl-(isopropoxycarbonyloxymethoxy)phosphoryl]oxymethyl Isopropyl Carbonate
42. Smr004701787
43. Gs 4331-05 (*1:1 Fumarate Salt*)
44. Stribild Component Tenofovir Disoproxil
45. Telura Component Of Tenofovir Disoproxil
46. Ab01568241_01
47. 138t509
48. A814272
49. J-519478
50. Q27132753
51. Tenofovir Bis(isopropyloxycarbonyloxymethyl) Ester [mi]
52. 9-[(r)-2-[[bis[[(isopropoxycarbonyl)oxy] Methoxy]phosphinyl]methoxy]propyl]adenine
53. (r)-(((((1-(6-amino-9h-purin-9-yl)propan-2-yl)oxy)methyl)phosphoryl)bis(oxy))bis(methylene) Diisopropyl Bis(carbonate)
54. (r)-(((((1-(6-amino-9h-purin-9-yl)propan-2-yl)oxy)methyl)phosphoryl)bis(oxy))bis(methylene)diisopropyldicarbonate
55. (r)-(((1-(6-amino-9h-purin-9-yl)propan-2-yloxy)methyl)phosphoryl)bis(oxy)bis(methylene) Isopropyl Dicarbonate
| Molecular Weight | 519.4 g/mol |
|---|---|
| Molecular Formula | C19H30N5O10P |
| XLogP3 | 1.6 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 14 |
| Rotatable Bond Count | 17 |
| Exact Mass | 519.17302917 g/mol |
| Monoisotopic Mass | 519.17302917 g/mol |
| Topological Polar Surface Area | 185 Ų |
| Heavy Atom Count | 35 |
| Formal Charge | 0 |
| Complexity | 698 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 1 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Anti-HIV Agents, Reverse Transcriptase Inhibitors
National Library of Medicine's Medical Subject Headings online file (MeSH, 2012)
Tenofovir disoproxil fumarate is used in conjunction with other antiretroviral agents for the treatment of human immunodeficiency virus type 1 (HIV-1) infections in adults. /Included in US product labeling/
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 747
Tenofovir is used for the management of chronic hepatitis B virus (HBV) infection in adults. This indication is based on histologic, virologic, biochemical, and serologic responses in adults with hepatitis B e antigen (HBeAg)-positive or -negative chronic HBV with compensated liver function.
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 748
Tenofovir disoproxil fumarate (TDF), emtricitabine (FTC), and efavirenz (EFV) are the three components of the once-daily, single tablet regimen (Atripla) for treatment of HIV-1 infection. Previous cell culture studies have demonstrated that the double combination of tenofovir (TFV), the parent drug of TDF, and FTC were additive to synergistic in their anti-HIV activity, which correlated with increased levels of intracellular phosphorylation of both compounds. In this study, /researchers/ demonstrated the combinations of TFV+FTC, TFV+EFV, FTC+EFV, and TFV+FTC+EFV synergistically inhibit HIV replication in cell culture and synergistically inhibit HIV-1 reverse transcriptase (RT) catalyzed DNA synthesis in biochemical assays. Several different methods were applied to define synergy including median-effect analysis, MacSynergyII and quantitative isobologram analysis. We demonstrated that the enhanced formation of dead-end complexes (DEC) by HIV-1 RT and TFV-terminated DNA in the presence of FTC-triphosphate (TP) could contribute to the synergy observed for the combination of TFV+FTC, possibly through reduced terminal NRTI excision. Furthermore, /researchers/ showed that EFV facilitated efficient formation of stable, DEC-like complexes by TFV- or FTC-monophosphate (MP)-terminated DNA and this can contribute to the synergistic inhibition of HIV-1 RT by TFV-diphosphate (DP)+EFV and FTC-TP+EFV combinations. This study demonstrated a clear correlation between the synergistic antiviral activities of TFV+FTC, TFV+EFV, FTC+EFV, and TFV+FTC+EFV combinations and synergistic HIV-1 RT inhibition at the enzymatic level. /Researchers/ propose the molecular mechanisms for the TFV+FTC+EFV synergy to be a combination of increased levels of the active metabolites TFV-DP and FTC-TP and enhanced DEC formation by a chain-terminated DNA and HIV-1 RT in the presence of the second and the third drug in the combination. This study furthers the understanding of the longstanding observations of synergistic anti-HIV-1 effects of many NRTI+NNRTI and certain NRTI+NRTI combinations in cell culture, and provides biochemical evidence that combinations of anti-HIV agents can increase the intracellular drug efficacy, without increasing the extracellular drug concentrations.
PMID:19439089 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2693498 Feng JY et al; Retrovirology 6: 44 (2009)
/BOXED WARNING/ WARNING: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH STEATOSIS and POST TREATMENT EXACERBATION OF HEPATITIS. Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogs, including Viread, in combination with other antiretrovirals. Severe acute exacerbations of hepatitis have been reported in HBV-infected patients who have discontinued anti-hepatitis B therapy, including Viread. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue anti-hepatitis B therapy, including Viread. If appropriate, resumption of anti-hepatitis B therapy may be warranted.
US Natl Inst Health; DailyMed. Current Medication Information for VIREAD (tenofovir disoproxil fumarate) tablet, coated VIREAD (tenofovir disoproxil fumarate) powder (November 2012). Available from, as of November 14, 2012: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
Lactic acidosis and severe hepatomegaly with steatosis (sometimes fatal) have been reported rarely in patients receiving nucleoside reverse transcriptase inhibitors alone or in conjunction with other antiretroviral agents. Most reported cases have involved women; obesity and long-term therapy with a nucleoside reverse transcriptase inhibitor also may be risk factors. Caution should be observed when nucleoside analogs are used in patients with known risk factors for liver disease; however, lactic acidosis and severe hepatomegaly with steatosis have been reported in patients with no known risk factors. Tenofovir therapy should be interrupted in any patient with clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (signs of hepatotoxicity include hepatomegaly and steatosis even in the absence of marked increases in serum aminotransferase concentrations).
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 749
Redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and general cushingoid appearance, has been reported with antiretroviral therapy.
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 750
The most common adverse effects in HIV-infected patients receiving tenofovir disoproxil fumarate are rash, diarrhea, headache, pain, depression, asthenia, and nausea. The most common adverse effect in HIV-infected patients receiving tenofovir disoproxil fumarate is nausea.
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 750
For more Drug Warnings (Complete) data for TENOFOVIR DISOPROXIL FUMARATE (14 total), please visit the HSDB record page.
Tenofovir is indicated in combination with other antiretroviral agents for the management of HIV-1 infection in adults and pediatric patients 2 years of age and older. It is also indicated for the treatment of chronic hepatitis B in adults and pediatric patients 12 years of age and older. This drug is also a component of multiple products used for the management of HIV-1 infection,. Safety and effectiveness of tenofovir disoproxil in pediatric patients younger than 2 years of age has not been established to this date.
* HIV1 infection:
Tenofovir disoproxil Zentiva is indicated in combination with other antiretroviral medicinal products for the treatment of HIV1 infected adults.
In adults, the demonstration of the benefit of tenofovir disoproxil in HIV1 infection is based on results of one study in treatmentnave patients, including patients with a high viral load (> 100,000 copies/ml) and studies in which tenofovir disoproxil was added to stable background therapy (mainly tritherapy) in antiretroviral pretreated patients experiencing early virological failure (< 10,000 copies/ml, with the majority of patients having < 5,000 copies/ml).
Tenofovir disoproxil Zentiva is also indicated for the treatment of HIV1 infected adolescents, with NRTI (nucleotide reverse transcriptase inhibitor) resistance or toxicities precluding the use of first line agents, aged 12 to < 18 years.
The choice of Tenofovir disoproxil Zentiva to treat antiretroviralexperienced patients with HIV1 infection should be based on individual viral resistance testing and/or treatment history of patients.
* Hepatitis B infection:
Tenofovir disoproxil Zentiva is indicated for the treatment of chronic hepatitis B in adults with:
- compensated liver disease, with evidence of active viral replication, persistently elevated serum alanine aminotransferase (ALT) levels and histological evidence of active inflammation and/or fibrosis (see section 5. 1);
- evidence of lamivudine-resistant hepatitis B virus (see sections 4. 8 and 5. 1);
- decompensated liver disease (see sections 4. 4, 4. 8 and 5. 1).
Tenofovir disoproxil Zentiva is indicated for the treatment of chronic hepatitis B in adolescents 12 to < 18 years of age with:
- compensated liver disease and evidence of immune active disease, i. e. active viral replication, persistently elevated serum ALT levels and histological evidence of active inflammation and/or fibrosis (see sections 4. 4, 4. 8 and 5. 1).
* HIV 1 infection:
Viread 123 mg film coated tablets are indicated in combination with other antiretroviral medicinal products for the treatment of HIV 1 infected paediatric patients, with NRTI resistance or toxicities precluding the use of first line agents, aged 6 to < 12 years who weigh from 17 kg to less than 22 kg.
The choice of Viread to treat antiretroviral experienced patients with HIV 1 infection should be based on individual viral resistance testing and/or treatment history of patients.
* Hepatitis B infection:
Viread 123 mg film coated tablets are indicated for the treatment of chronic hepatitis B in paediatric patients aged 6 to < 12 years who weigh from 17 kg to less than 22 kg, with
compensated liver disease and evidence of immune active disease, i. e. active viral replication and persistently elevated serum ALT levels, or histological evidence of moderate to severe inflammation and/or fibrosis. With respect to the decision to initiate treatment in paediatric patients, see sections 4. 2, 4. 4, 4. 8 and 5. 1.
* HIV 1 infection:
Viread 163 mg film coated tablets are indicated in combination with other antiretroviral medicinal products for the treatment of HIV 1 infected paediatric patients, with NRTI resistance or toxicities precluding the use of first line agents, aged 6 to < 12 years who weigh from 22 kg to less than 28 kg.
The choice of Viread to treat antiretroviral experienced patients with HIV 1 infection should be based on individual viral resistance testing and/or treatment history of patients.
* Hepatitis B infection:
Viread 163 mg film coated tablets are indicated for the treatment of chronic hepatitis B in paediatric patients aged 6 to < 12 years who weigh from 22 kg to less than 28 kg, with:
compensated liver disease and evidence of immune active disease, i. e. active viral replication and persistently elevated serum ALT levels, or histological evidence of moderate to severe inflammation and/or fibrosis. With respect to the decision to initiate treatment in paediatric patients, see sections 4. 2, 4. 4, 4. 8 and 5. 1.
* HIV 1 infection:
Viread 204 mg film coated tablets are indicated in combination with other antiretroviral medicinal products for the treatment of HIV 1 infected paediatric patients, with NRTI resistance or toxicities precluding the use of first line agents, aged 6 to < 12 years who weigh from 28 kg to less than 35 kg.
The choice of Viread to treat antiretroviral experienced patients with HIV 1 infection should be based on individual viral resistance testing and/or treatment history of patients.
* Hepatitis B infection:
Viread 204 mg film coated tablets are indicated for the treatment of chronic hepatitis B in paediatric patients aged 6 to < 12 years who weigh from 28 kg to less than 35 kg, with:
compensated liver disease and evidence of immune active disease, i. e. active viral replication and persistently elevated serum ALT levels or histological evidence of moderate to severe inflammation and/or fibrosis. With respect to the decision to initiate treatment in paediatric patients, see sections 4. 2, 4. 4, 4. 8 and 5. 1.
* HIV 1 infection:
Viread 245 mg film coated tablets are indicated in combination with other antiretroviral medicinal products for the treatment of HIV 1 infected adults.
In adults, the demonstration of the benefit of Viread in HIV 1 infection is based on results of one study in treatment nave patients, including patients with a high viral load (> 100,000 copies/ml) and studies in which Viread was added to stable background therapy (mainly tritherapy) in antiretroviral pre-treated patients experiencing early virological failure (< 10,000 copies/ml, with the majority of patients having < 5,000 copies/ml).
Viread 245 mg film coated tablets are also indicated for the treatment of HIV 1 infected adolescents, with NRTI resistance or toxicities precluding the use of first line agents, aged 12 to < 18 years.
The choice of Viread to treat antiretroviral experienced patients with HIV 1 infection should be based on individual viral resistance testing and/or treatment history of patients.
* Hepatitis B infection:
Viread 245 mg film coated tablets are indicated for the treatment of chronic hepatitis B in adults with:
compensated liver disease, with evidence of active viral replication, persistently elevated serum alanine aminotransferase (ALT) levels and histological evidence of active inflammation and/or fibrosis (see section 5. 1). evidence of lamivudine resistant hepatitis B virus (see sections 4. 8 and 5. 1). decompensated liver disease (see sections 4. 4, 4. 8 and 5. 1). Viread 245 mg film coated tablets are indicated for the treatment of chronic hepatitis B in adolescents 12 to < 18 years of age with:
compensated liver disease and evidence of immune active disease, i. e. active viral replication and persistently elevated serum ALT levels, or histological evidence of moderate to severe inflammation and/or fibrosis. With respect to the decision to initiate treatment in paediatric patients, see sections 4. 2, 4. 4, 4. 8 and 5. 1.
* HIV 1 infection:
Viread 33 mg/g granules are indicated in combination with other antiretroviral medicinal products for the treatment of HIV 1 infected paediatric patients, with NRTI resistance or toxicities precluding the use of first line agents, from 2 to < 6 years of age, and above 6 years of age for whom a solid dosage form is not appropriate.
Viread 33 mg/g granules are also indicated in combination with other antiretroviral medicinal products for the treatment of HIV 1 infected adults for whom a solid dosage form is not appropriate.
In adults, the demonstration of the benefit of Viread in HIV 1 infection is based on results of one study in treatment nave patients, including patients with a high viral load (> 100,000 copies/ml) and studies in which Viread was added to stable background therapy (mainly tritherapy) in antiretroviral pre-treated patients experiencing early virological failure (< 10,000 copies/ml, with the majority of patients having < 5,000 copies/ml).
The choice of Viread to treat antiretroviral experienced patients with HIV 1 infection should be based on individual viral resistance testing and/or treatment history of patients.
Hepatitis B infectionViread 33 mg/g granules are indicated for the treatment of chronic hepatitis B in adults for whom a solid dosage form is not appropriate with:
compensated liver disease, with evidence of active viral replication, persistently elevated serum alanine aminotransferase (ALT) levels and histological evidence of active inflammation and/or fibrosis (see section 5. 1). evidence of lamivudine resistant hepatitis B virus (see sections 4. 8 and 5. 1). decompensated liver disease (see sections 4. 4, 4. 8 and 5. 1).
Viread 33 mg/g granules are also indicated for the treatment of chronic hepatitis B in paediatric patients2 to < 18 years of age for whom a solid dosage form is not appropriate with:
compensated liver disease and evidence of immune active disease, i. e. active viral replication, and persistently elevated serum ALT levels, or histological evidence of moderate to severe inflammation and/or fibrosis. With respect to the decision to initiate treatment in paediatric patients, see sections 4. 2, 4. 4, 4. 8 and 5. 1.
HIV-1 infection
Tenofovir disoproxil 245 mg film-coated tablets are indicated in combination with other antiretroviral medicinal products for the treatment of HIV-1 infected adults.
In adults, the demonstration of the benefit of tenofovir disoproxil in HIV-1 infection is based on results of one study in treatment-nave patients, including patients with a high viral load (> 100,000 copies/ml) and studies in which tenofovir disoproxil was added to stable background therapy (mainly tritherapy) in antiretroviral pre-treated patients experiencing early virological failure (< 10,000 copies/ml, with the majority of patients having < 5,000 copies/ml).
Tenofovir disoproxil 245 mg film-coated tablets are also indicated for the treatment of HIV-1 infected adolescents, with NRTI resistance or toxicities precluding the use of first line agents, aged 12 to < 18 years.
The choice of tenofovir disoproxil to treat antiretroviral-experienced patients with HIV-1 infection should be based on individual viral resistance testing and/or treatment history of patients.
Hepatitis B infection
Tenofovir disoproxil 245 mg film-coated tablets are indicated for the treatment of chronic hepatitis B in adults with:
- compensated liver disease, with evidence of active viral replication, persistently elevated serum alanine aminotransferase (ALT) levels and histological evidence of active inflammation and/or fibrosis.
- evidence of lamivudine-resistant hepatitis B virus.
- decompensated liver disease.
Tenofovir disoproxil 245 mg film-coated tablets are indicated for the treatment of chronic hepatitis B in adolescents 12 to < 18 years of age with:
- compensated liver disease and evidence of immune active disease, i. e. active viral replication, persistently elevated serum ALT levels and histological evidence of active inflammation and/or fibrosis.
Treatment of chronic viral hepatitis B, Treatment of human immunodeficiency virus (HIV-1) infection
This drug prevents viral DNA chain elongation through inhibition of enzymes necessary for host cell infection viral replication in HIV-1 and Hepatitis B infections,. **In vitro effects** The antiviral activity of tenofovir against in laboratory and clinical isolates of HIV-1 was studied in lymphoblastoid cell lines, primary monocyte/macrophage cells, in addition to peripheral blood lymphocytes. The EC50 (50% effective concentration) values of tenofovir against HIV-1 virus ranged between 0.04 M to 8.5 M. **Combination of tenofovir disoproxil with other drugs** In drug combination studies of tenofovir with nucleoside reverse transcriptase inhibitors (abacavir, didanosine, lamivudine, stavudine, zalcitabine, zidovudine), non-nucleoside reverse transcriptase inhibitors (delavirdine, efavirenz, nevirapine), and protease inhibitors (amprenavir, indinavir, nelfinavir, ritonavir, saquinavir), additive and synergistic effects were seen. Tenofovir demonstrated antiviral activities in cell cultures against HIV-1.
Antiviral Agents
Agents used in the prophylaxis or therapy of VIRUS DISEASES. Some of the ways they may act include preventing viral replication by inhibiting viral DNA polymerase; binding to specific cell-surface receptors and inhibiting viral penetration or uncoating; inhibiting viral protein synthesis; or blocking late stages of virus assembly. (See all compounds classified as Antiviral Agents.)
Anti-HIV Agents
Agents used to treat AIDS and/or stop the spread of the HIV infection. These do not include drugs used to treat symptoms or opportunistic infections associated with AIDS. (See all compounds classified as Anti-HIV Agents.)
Reverse Transcriptase Inhibitors
Inhibitors of reverse transcriptase (RNA-DIRECTED DNA POLYMERASE), an enzyme that synthesizes DNA on an RNA template. (See all compounds classified as Reverse Transcriptase Inhibitors.)
J05AF07
J05AF07
J05AF07
J05AF13
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
J - Antiinfectives for systemic use
J05 - Antivirals for systemic use
J05A - Direct acting antivirals
J05AF - Nucleoside and nucleotide reverse transcriptase inhibitors
J05AF07 - Tenofovir disoproxil
Absorption
After oral administration of tenofovir disoproxil to patients with HIV infection, tenofovir disoproxil is quickly absorbed and metabolized to tenofovir. Administration of tenofovir disoproxil 300 mg tablets after a high-fat meal increases the oral bioavailability of this drug, as demonstrated by an increase in tenofovir AUC0- of about 40% as well as an increase in Cmax of about 14%. On the contrary, the administration of tenofovir disoproxil with a light meal did not exert a relevant effect on the pharmacokinetics of tenofovir when compared to administration under fasting conditions. The presence of ingested food slows the time to tenofovir Cmax by approximately 1 hour. Cmax and AUC of tenofovir are 0.33 0.12 g/mL and 3.32 1.37 ghr/mL after several doses of tenofovir disoproxil 300 mg once daily in the fed state when meal content is not controlled.
Route of Elimination
Following IV administration of tenofovir, approximately 7080% of the dose is recovered in the urine as unchanged tenofovir within 72 hours of dosing. Tenofovir is eliminated by a combination of glomerular filtration and active tubular secretion. There may be competition for elimination with other compounds that are also eliminated by the kidneys.
Volume of Distribution
The volume of distribution at steady-state is 1.3 0.6 L/kg and 1.2 0.4 L/kg, following intravenous administration of tenofovir 1.0 mg/kg and 3.0 mg/kg. After oral administration of tenofovir disoproxil, tenofovir is distributed to the majority tissues with the highest concentrations measured in the kidney, liver and the intestinal contents (based on data from preclinical studies).
Clearance
The clearance of tenofovir is highly dependent on renal function and may vary greatly. Total clearance has been estimated to be approximately 230 ml/h/kg (approximately 300 ml/min). On average, renal clearance has been estimated to be approximately 160 ml/h/kg (approximately 210 ml/min), which is in excess of the glomerular filtration rate. This shows that active tubular secretion is an essential part of the elimination of tenofovir. The FDA label provides specific guidelines for dosing according to renal function. It is important to consult product labeling before administering tenofovir to individuals with renal dysfunction, as the clearance of this drug may vary greatly among these patients.
Following IV administration of tenofovir, approximately 70-80% of the dose is recovered in the urine as unchanged tenofovir within 72 hours of dosing. Following single dose, oral administration of tenofovir, the terminal elimination half-life of tenofovir is approximately 17 hours. After multiple oral doses of tenofovir 300 mg once daily (under fed conditions), 32 + or - 10% of the administered dose is recovered in urine over 24 hours. Tenofovir is eliminated by a combination of glomerular filtration and active tubular secretion. There may be competition for elimination with other compounds that are also renally eliminated.
US Natl Inst Health; DailyMed. Current Medication Information for VIREAD (tenofovir disoproxil fumarate) tablet, coated VIREAD (tenofovir disoproxil fumarate) powder (November 2012). Available from, as of November 14, 2012: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
In vitro binding of tenofovir to human plasma or serum proteins is less than 0.7 and 7.2%, respectively, over the tenofovir concentration range 0.01 to 25 ug/mL. The volume of distribution at steady-state is 1.3 + or - 0.6 L/kg and 1.2 + or - 0.4 L/kg, following intravenous administration of tenofovir 1.0 mg/kg and 3.0 mg/kg.
US Natl Inst Health; DailyMed. Current Medication Information for VIREAD (tenofovir disoproxil fumarate) tablet, coated VIREAD (tenofovir disoproxil fumarate) powder (November 2012). Available from, as of November 14, 2012: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
Viread is a water soluble diester prodrug of the active ingredient tenofovir. The oral bioavailability of tenofovir from Viread in fasted subjects is approximately 25%. Following oral administration of a single dose of Viread 300 mg to HIV-1 infected subjects in the fasted state, maximum serum concentrations (Cmax) are achieved in 1.0 + or - 0.4 hr. Cmax and AUC values are 0.30 + or - 0.09 ug/mL and 2.29 + or - 0.69 ug hr/mL, respectively.
US Natl Inst Health; DailyMed. Current Medication Information for VIREAD (tenofovir disoproxil fumarate) tablet, coated VIREAD (tenofovir disoproxil fumarate) powder (November 2012). Available from, as of November 14, 2012: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
Administration of Viread 300 mg tablets following a high-fat meal (approximately 700 to 1000 kcal containing 40 to 50% fat) increases the oral bioavailability, with an increase in tenofovir AUC of approximately 40% and an increase in Cmax of approximately 14%. However, administration of Viread with a light meal did not have a significant effect on the pharmacokinetics of tenofovir when compared to fasted administration of the drug. Food delays the time to tenofovir Cmax by approximately 1 hour. Cmax and AUC of tenofovir are 0.33 + or - 0.12 ug/mL and 3.32 + or - 1.37 ug hr/mL following multiple doses of Viread 300 mg once daily in the fed state, when meal content was not controlled.
US Natl Inst Health; DailyMed. Current Medication Information for VIREAD (tenofovir disoproxil fumarate) tablet, coated VIREAD (tenofovir disoproxil fumarate) powder (November 2012). Available from, as of November 14, 2012: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
For more Absorption, Distribution and Excretion (Complete) data for TENOFOVIR DISOPROXIL FUMARATE (6 total), please visit the HSDB record page.
Tenofovir disoproxil fumarate is the fumarate salt of the prodrug _tenofovir disoproxil_. Tenofovir disoproxil is absorbed and converted to its active form, _tenofovir_, a nucleoside monophosphate (nucleotide) analog. Tenofovir is then converted to the active metabolite, _tenofovir diphosphate_, a chain terminator, by constitutively expressed enzymes in the cell. Two phosphorylation steps are required to convert tenofovir disoproxil to the active drug form. The cytochrome P450 enzyme system is not involved with the metabolism of tenofovir disoproxil or tenofovir.
Tenofovir disoproxil fumarate is a prodrug and is not active until it undergoes diester hydrolysis in vivo to tenofovir and subsequently is metabolized to the active metabolite (tenofovir diphosphate).
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 751
When a single oral dose is given, the terminal elimination half-life is approximately 17 hours.
Following single dose, oral administration of Viread, the terminal elimination half-life of tenofovir is approximately 17 hours.
US Natl Inst Health; DailyMed. Current Medication Information for VIREAD (tenofovir disoproxil fumarate) tablet, coated VIREAD (tenofovir disoproxil fumarate) powder (November 2012). Available from, as of November 14, 2012: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
Tenofovir belongs to a class of antiretroviral drugs known as nucleotide analog reverse transcriptase inhibitors (NtRTIs), which block reverse transcriptase, an enzyme necessary for viral production in HIV-infected individuals. This enables the management of HIV viral load through decreased viral replication. Tenofovir disoproxil fumarate is the fumarate salt of the prodrug _tenofovir disoproxil_. Tenofovir disoproxil is absorbed and converted to its active form, _tenofovir_, a nucleoside monophosphate (nucleotide) analog. Tenofovir is then converted to the active metabolite, _tenofovir diphosphate_, a chain terminator, by constitutively expressed enzymes in the cell. Tenofovir diphosphate inhibits HIV-1 reverse transcriptase and the Hepatitis B polymerase by direct binding competition with the natural deoxyribonucleotide substrate (deoxyadenosine 5-triphosphate) and, after integration into DNA, causes viral DNA chain termination,. **A note on resistance** HIV-1 isolates with decreased susceptibility to tenofovir have been identified in cell culture studies. These viruses expressed a _K65R_ substitution in reverse transcriptase and showed a 2 4 fold decrease in susceptibility to treatment with tenofovir.
Like nucleoside reverse transcriptase inhibitors, the antiviral activity of tenofovir depends on intracellular conversion to an active metabolite; however, tenofovir is a nucleotide containing a phosphonate group and the steps and enzymes involved in enzymatic conversion to the active metabolite differ from those involved in the conversion of nucleoside reverse transcriptase inhibitors. Tenofovir is phosphorylated by cellular nucleotide kinases to tenofovir diphosphate; tenofovir diphosphate is a structural analog of deoxyadenosine-5-triphosphate, the usual substrate for viral RNA-directed DNA polymerase. Although other mechanisms may be involved in the antiretroviral activities of the drug, tenofovir diphosphate appears to compete with deoxyadenosine-5-triphosphate for viral RNA-directed DNA polymerase and for incorporation into viral DNA. Following incorporation of tenofovir diphosphate into the viral DNA chain, DNA synthesis is prematurely terminated because the absence of the 3-hydroxy group on the drug prevents further 5 to 3 phosphodiester linkages.
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 751
Tenofovir disoproxil fumarate, a synthetic antiretroviral agent, is a nucleotide reverse transcriptase inhibitor. Tenofovir disoproxil fumarate is a prodrug and is not active until it undergoes diester hydrolysis in vivo to tenofovir and subsequently is metabolized to the active metabolite (tenofovir diphosphate). Following conversion to the pharmacologically active metabolite, tenofovir apparently inhibits replication of retroviruses, including human immunodeficiency virus type 1 (HIV-1), by interfering with viral RNA-directed DNA polymerase (reverse transcriptase). In vitro studies indicate that tenofovir is active against HIV-1, HIV-2, and hepatitis B virus (HBV); the drug also has some activity against HIV-2.
American Society of Health-System Pharmacists 2012; Drug Information 2012. Bethesda, MD. 2012, p. 751
Tenofovir disoproxil fumarate (TDF) is an oral prodrug and acyclic nucleotide analog of adenosine monophosphate that inhibits HIV-1 (HIV) reverse transcriptase. A growing subset of TDF-treated HIV(+) individuals presented with acute renal failure, suggesting tenofovir-associated kidney-specific toxicity. ... Previous studies using an HIV transgenic mouse model (TG) demonstrated specific changes in renal proximal tubular mitochondrial DNA (mtDNA) abundance. Nucleosides are regulated in biological systems via transport and metabolism in cellular compartments. In this study, the role(s) of organic anion transporter type 1 (OAT1) and multidrug-resistant protein type 4 (MRP4) in transport and regulation of tenofovir in proximal tubules were assessed. Renal toxicity was assessed in kidney tissues from OAT1 knockout (KO) or MRP4 KO compared with wild-type (WT, C57BL/6) mice following treatment with TDF (0.11 mg/day), didanosine (ddI, a related adenosine analog, 0.14 mg/day) or vehicle (0.1 M NaOH) daily gavage for 5 weeks. Laser-capture microdissection (LCM) was used to isolate renal proximal tubules for molecular analyses. mtDNA abundance and ultrastructural pathology were analyzed. mtDNA abundance in whole kidneys from both KO and WT was unchanged regardless of treatment. Renal proximal tubular mtDNA abundance from OAT1 KO also remained unchanged, suggesting prevention of TDF toxicity due to loss of tenofovir transport into proximal tubules. In contrast, renal proximal tubules from MRP4 KO exhibited increased mtDNA abundance following TDF treatment compared with WT littermates, suggesting compensation. Renal proximal tubules from TDF-treated WT and MRP4 KO exhibited increased numbers of irregular mitochondria with sparse, fragmented cristae compared with OAT1 KO. Treatment with ddI had a compensatory effect on mtDNA abundance in OAT1 KO but not in MRP4 KO. Both OAT1 and MRP4 have a direct role in transport and efflux of tenofovir, regulating levels of tenofovir in proximal tubules. Disruption of OAT1 activity prevents tenofovir toxicity but loss of MRP4 can lead to increased renal proximal tubular toxicity. These data help to explain mechanisms of human TDF renal toxicity.
PMID:21403643 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3103636 Kohler JJ et al; Lab Invest 91 (6): 852-8 (2011)a
Tenofovir disoproxil fumarate (tenofovir DF) use has been associated with renal dysfunction and Fanconi syndrome. Tenofovir is taken up into renal tubules by anion transporters where high intracellular drug concentration may induce a functionally relevant depletion of mitochondrial DNA (mtDNA). /The researchers/ investigated if tenofovir may induce renal mtDNA depletion and respiratory chain dysfunction. Rats (n = 8) were gavaged daily with 100 mg x kg(-1) x d(-1) of tenofovir DF or didanosine. Kidneys and livers were examined after 8 weeks of treatment. The tenofovir group had significantly lower body and kidney weights than rats exposed to water or didanosine. Proximal but not distal tubules were of increased diameter and contained small lipid droplets. Tubular mitochondria were enlarged, and their crystal architecture was disrupted. Tenofovir-exposed kidneys contained low mtDNA copy numbers and impaired expression of mtDNA-encoded cytochrome c oxidase (COX) I but not nucleus-encoded COX IV subunits. Histochemistry demonstrated low tubular COX and nicotinamide adenine dinucleotide dehydrogenase (NADH-DH) activities, whereas succinate dehydrogenase activity was preserved. COX activity was preserved in the glomeruli of tenofovir-exposed rats. Didanosine did not elicit renal effects but, unlike tenofovir, depleted mtDNA in liver (by 52%). Tenofovir DF induces an organ-specific nephrotoxicity with mtDNA depletion and dysfunction of mtDNA-encoded respiratory chain subunits. The data do not support nephrotoxicity of didanosine.
PMID:19582894 Lebrecht D et al; J Acquir Immune Defic Syndr 51 (3): 258-63 (2009)