1. Hydrochloride, Mianserin
2. Lerivon
3. Mianserin Hydrochloride
4. Mianserin Monohydrochloride
5. Monohydrochloride, Mianserin
6. Org Gb 94
7. Tolvon
1. Mianserine
2. 24219-97-4
3. Mianseryna [polish]
4. Mianserina
5. Mianserinum
6. Mianseryna
7. Norval
8. Mianserine [inn-french]
9. Mianserinum [inn-latin]
10. Mianserina [inn-spanish]
11. Tolvon
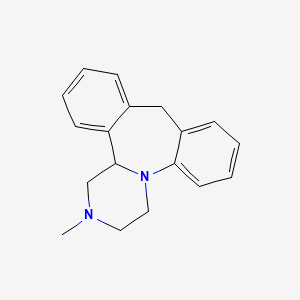
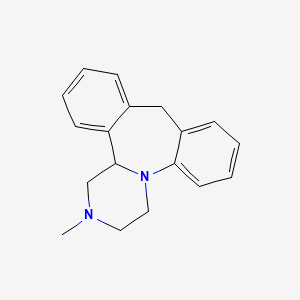
12. 2-methyl-1,2,3,4,10,14b-hexahydrodibenzo[c,f]pyrazino[1,2-a]azepine
13. Mianserin (inn)
14. 1,2,3,4,10,14b-hexahydro-2-methyldibenzo(c,f)pyrazino(1,2-a)azepine
15. Lerivon
16. Chebi:51137
17. Chembl6437
18. 250pji13lm
19. Dibenzo[c,f]pyrazino[1,2-a]azepine, 1,2,3,4,10,14b-hexahydro-2-methyl-
20. Ncgc00015656-06
21. J16.389i
22. Mianserin [inn]
23. Dsstox_cid_3317
24. Mianserin [inn:ban]
25. Dibenzo(c,f)pyrazino(1,2-a)azepine, 1,2,3,4,10,14b-hexahydro-2-methyl-
26. Dsstox_rid_76974
27. Dsstox_gsid_23317
28. 1,2,3,4,10,14b-hexahydro-2-methyldibenzo[c,f]pyrazino[1,2-a]azepine
29. Cas-24219-97-4
30. Tolvon (tn)
31. (+/-)-mianserin
32. Hsdb 7182
33. Einecs 246-088-6
34. Brn 0755346
35. Unii-250pji13lm
36. Lantanon
37. Depnon
38. Mianserin A
39. (+-)-athymil
40. Spectrum_001810
41. Mianserin [mi]
42. Mianserin [hsdb]
43. Prestwick0_000099
44. Prestwick1_000099
45. Prestwick2_000099
46. Prestwick3_000099
47. Spectrum2_001203
48. Spectrum3_001836
49. Spectrum4_001260
50. Spectrum5_001772
51. Mianserin [vandf]
52. Biomol-nt_000135
53. Mianserin [who-dd]
54. Lopac0_000744
55. Oprea1_703627
56. Schembl18020
57. Bspbio_000058
58. Bspbio_003511
59. Gtpl135
60. Kbiogr_001820
61. Kbioss_002303
62. Divk1c_000844
63. Spbio_000986
64. Spbio_001997
65. Bpbio1_000064
66. Bpbio1_000331
67. Dtxsid6023317
68. Kbio1_000844
69. Kbio2_002301
70. Kbio2_004869
71. Kbio2_007437
72. Kbio3_003016
73. Ninds_000844
74. Hms2089a04
75. Hy-b0188
76. Tox21_110191
77. Ac-631
78. Bdbm50222218
79. Pdsp1_001532
80. Pdsp2_001516
81. Akos005216268
82. Tox21_110191_1
83. Ccg-204829
84. Cs-2078
85. Db06148
86. Sdccgsbi-0050722.p004
87. Idi1_000844
88. Ncgc00015656-04
89. Ncgc00015656-05
90. Ncgc00015656-08
91. Ncgc00015656-09
92. Ncgc00015656-10
93. Ncgc00015656-12
94. Ncgc00015656-23
95. Ncgc00024926-03
96. Ncgc00024926-04
97. 5-methyl-2,5-diazatetracyclo[13.4.0.0^{2,7}.0^{8,13}]nonadeca-1(15),8(13),9,11,16,18-hexaene
98. Sbi-0050722.p003
99. Am20041174
100. Ft-0697022
101. D08216
102. L000736
103. Q416701
104. Brd-a19661776-001-01-5
105. Brd-a19661776-003-05-2
106. Brd-a19661776-003-16-9
107. 2-methyl-1,2,3,4,10,14b-hexahydrodibenzo[c,f]pyrazino[1,2-a]azepine #
108. 1,2,3,4,10,14b-hexahydro-2-methyldibenzo(c,f)-pyrazino(1,2-a)azepine
109. 5-methyl-2,5-diazatetracyclo[13.4.0.02,7.08,13]nonadeca-1(19),8,10,12,15,17-hexaene
110. 5-methyl-2,5-diazatetracyclo[13.4.0.0^{2,7}.0^{8,13}]nonadeca-1(19),8,10,12,15,17-hexaene
| Molecular Weight | 264.4 g/mol |
|---|---|
| Molecular Formula | C18H20N2 |
| XLogP3 | 3.4 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 2 |
| Rotatable Bond Count | 0 |
| Exact Mass | 264.162648646 g/mol |
| Monoisotopic Mass | 264.162648646 g/mol |
| Topological Polar Surface Area | 6.5 Ų |
| Heavy Atom Count | 20 |
| Formal Charge | 0 |
| Complexity | 342 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 1 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
EXPTL Therapy: 114 patients with chronic tension headache (more than 10 days per month for at least 6 months) were treated with placebo, clomipramine or mianserin in a double blind parallel group comparison. Eighty-two patients completed the study. Headache pain was scored weekly on visual analogue scales for the 6 weeks of treatment. Observer-rating of headache was made at entry, after 3 weeks and after 6 weeks of treatment. In all groups, headache complaints decreased significantly compared to baseline. With the main parameter the decrease on both clomipramine and mianserin was significant compared to placebo. Although the trend was the same for the other parameters, the changes relative to placebo did not reach statistical significance.
PMID:2182566 Langemark M et al; Headache 30 (3): 118-21 (1990)
Mianserin is a tetracyclic compound advocated for the treatment of depressive illness and depression associated with anxiety. It combines antidepressant activity with a sedative effect and has an EEG and clinical activity profile similar to that of amitriptyline. It has an overall efficacy comparable with amitriptyline and imipramine in depressive illness, but at dosages which have achieved a similar overall clinical improvement, mianserin causes significantly fewer anticholinergic side effects than amitriptyline or imipramine and also appears less likely than these drugs to cause serious cardiotoxicity on overdosage. Mianserin also has anti-anxiety activity, but its role in treating patients with anxiety associated with primary depression has still to be clarified. Mianserin appears to be well tolerated by the elderly and by patients with cardiovascular disease, including those recovering from a recent myocardial infarction, and does not appear to antagonise the action of adrenergic neurone blocking antihypertensive drugs or affect the anticoagulant action of phenprocoumon.
PMID:359311 Brogden RN et al; Drugs 16 (4): 273-301 (1978)
In a 6-week study the efficacy of combined treatment of imipramine plus mianserin was compared to combined treatment of desipramine plus mianserin in patients with post-stroke depression. Patients were required to have a minimum baseline total score of 15 on the 17-item Hamilton Depression Scale (HAMD). The Melancholia Scale (MES) was also used to measure severity of depressive states to show that somatic symptoms had little influence on the evaluation of depression. Out of 120 stroke patients screened, 20 patients fulfilled the inclusion criteria. The doses of the drugs were flexible, using side-effects as a guide during treatment. Both intention to treat analysis and efficacy data (excluding patients who had dropped out during the first 2 weeks of treatment) showed that imipramine (mean dose 75 mg daily) plus mianserin (mean dose 25 mg daily) was superior to desipramine (mean dose 66 mg daily) plus mianserin (27 mg daily). The MES was found to be more sensitive than the HAMD for measuring change in depressive states during treatment. The assessment of side-effects using the UKU /side effect rating scale/ scale showed good tolerance in general. The only difference between the two treatment groups was seen in micturition disturbances, where the imipramine treated patients had most complaints after 14 days of treatment, but the symptoms disappeared despite continuous treatment.
PMID:7846193 Lauritzen L et al; Psychopharmacology (Berl) 114 (1): 119-22 (1994)
Seizures were observed following the withdrawal of mianserin 60 mg/day for 2 years. To our knowledge, this is the first report of convulsions after suspension of an antidepressant. This phenomenon was observed in a young woman (with no history of epilepsy or other organic diseases that may induce seizures) 10 days after abrupt discontinuation of long-term treatment with mianserin.
PMID:3397273 De Leo D et al; Ital J Neurol Sci 9 (2): 167-9 (1988)
An alcoholic woman who was admitted to hospital for detoxification was prescribed thyroxine because of hypothyroidism and mianserin to alleviate severe depression. After several weeks' treatment she became unwell and was readmitted to hospital. Haematological examination indicated agranulocytosis. Further extensive investigations elicited no cause for this other than the mianserin, since no such disturbance has been reported for thyroxine after years of use. Thus mianserin is probably implicated in this case of agranulocytosis. Although the response may have been idiosyncratic, it highlights the need to monitor new drugs during the early phases of widespread use.
PMID:761018 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1597989 Curson DA, Hale AS; Br Med J 1 (6160): 378-9 (1979)
Forty patients have been reported to the Committee on Safety of Medicines (CSM) because of convulsions occurring during treatment with mianserin, suggesting that this drug is more epileptogenic than tricyclic antidepressants. Details concerning 83% of these cases were obtained in a questionnaire study carried out in collaboration with the CSM and compared with those of a control group. ... As the CSM data do not allow for a reliable assessment of the relative epileptogenic effects of antidepressants, a comparison has been made between unpublished work on seizures occurring during treatment with imipramine and amitriptyline and published research on mianserin. Factors that might predispose to seizures include relevant family and past medical history, starting treatment, a change in dose, benzodiazepine withdrawal and concomitant treatment with other drugs that have epileptogenic properties.
Edwards JG, Glen-Bott M; Br J Clin Pharmacol 15 (Suppl 2) :299S-311S (1983)
Our report concerns 2 patients who developed delirium after an epileptic attack during mianserin treatment. In both cases the EEG showed a change with periodic sharp slow complexes similar to that seen in Creutzfeldt-Jakob disease. The symptoms subsided, however, and the EEG normalized after the antidepressant was discontinued, suggesting a noxious response to mianserin. If Creutzfeldt-Jakob-like changes in the EEG occur, the possible effect of antidepressant medication should be considered.
Koponen H et al; Neuropsychobiology 23 (3): 164-8 (1990-91)
For more Drug Warnings (Complete) data for MIANSERIN (8 total), please visit the HSDB record page.
For the treatment of depression.
Mianserin is a tetracyclic antidepressant that has antihistaminic and hypnosedative, but almost no anticholinergic, effect. It is a weak inhibitor of norepinephrine reuptake and strongly stimulates the release of norepinephrine. Interactions with serotonin receptors in the central nervous system have also been found. Its effect is usually noticeable after one to three weeks. Mianserin may cause drowsiness and hematological problems.
Antidepressive Agents, Second-Generation
A structurally and mechanistically diverse group of drugs that are not tricyclics or monoamine oxidase inhibitors. The most clinically important appear to act selectively on serotonergic systems, especially by inhibiting serotonin reuptake. (See all compounds classified as Antidepressive Agents, Second-Generation.)
Histamine H1 Antagonists
Drugs that selectively bind to but do not activate histamine H1 receptors, thereby blocking the actions of endogenous histamine. Included here are the classical antihistaminics that antagonize or prevent the action of histamine mainly in immediate hypersensitivity. They act in the bronchi, capillaries, and some other smooth muscles, and are used to prevent or allay motion sickness, seasonal rhinitis, and allergic dermatitis and to induce somnolence. The effects of blocking central nervous system H1 receptors are not as well understood. (See all compounds classified as Histamine H1 Antagonists.)
Serotonin Antagonists
Drugs that bind to but do not activate serotonin receptors, thereby blocking the actions of serotonin or SEROTONIN RECEPTOR AGONISTS. (See all compounds classified as Serotonin Antagonists.)
Adrenergic alpha-Antagonists
Drugs that bind to but do not activate alpha-adrenergic receptors thereby blocking the actions of endogenous or exogenous adrenergic agonists. Adrenergic alpha-antagonists are used in the treatment of hypertension, vasospasm, peripheral vascular disease, shock, and pheochromocytoma. (See all compounds classified as Adrenergic alpha-Antagonists.)
N06AX03
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
N - Nervous system
N06 - Psychoanaleptics
N06A - Antidepressants
N06AX - Other antidepressants
N06AX03 - Mianserin
Absorption
Absorbed following oral administration.
A pharmacokinetic study with mianserin HCl was performed in six healthy male subjects. The subjects were treated on different occasions intravenously with a constant-rate infusion of 5 mg mianserin HCl in 1 hr, orally with a single dose of 60 mg as two tablets of 30 mg each and with 60 mg as an oral solution. The wash-out period between treatments was 1 month. Blood samples were taken at predetermined times over a period of 120 hr following dosing. The mianserin concentration in the plasma samples was determined and the results were pharmacokinetically analyzed. The intravenous data could be adequately described by a 3-compartment model and the oral data by a 2-compartment model, both with first-order transfer and elimination rate constants. The mean plasma clearance of mianserin was found to be 19 +/- 2 L/hr (mean +/- SEM), the kinetic volume of distribution 444 +/- 250 L, the steady-state volume of distribution 242 +/- 171 L and the elimination half-life 33 +/- 5 hr. The absolute bioavailability in terms of extent of absorption was 22 +/- 3% for the solution and 20 +/- 3% for the tablets. The mean peak level for the solution was 79 +/- 11 ng/mL and for the tablets 54 +/- 5 ng /mL; mean peak time for the solution was 1.1 +/- 0.2 hr and for the tablets 1.4 +/- 0.2 hr. The mean absorption half-life for the solution was 0.43 +/- 0.13 hr and for the tablets 0.39 +/- 0.11 hr.
PMID:3830718 Timmer CJ et al; Eur J Drug Metab Pharmacokinet 10 (4): 315-23 (1985)
We studied mianserin kinetics after a single (60 mg) dose in eight inpatients suffering from depression. There was a considerable interpatient variability in plasma levels. Mean peak plasma levels (+/- SEM) were 114 +/- 26 ng/ml and were reached between 1 and 3 hr. The decline of mianserin levels in plasma was biphasic. The mean elimination t 1/2 was 21.6 +/- 3.1 hr and ranged from 10.7 to 40.8 hr. The estimated first-pass loss ranged from 26% to 48% (mean, 37%) and was lower than that reported for tertiary amine tricyclic antidepressants. The mean apparent volume of distribution (15.7 +/- 2.2 L/kg; 9.7 to 28.8 L/kg) was in the range of that for imipramine but somewhat lower than for maprotiline. Apparent total body clearance ranged from 0.33 to 0.81 L/hr/kg (mean +/- SEM, 0.52 +/- 0.05 L/hr/kg) and was of the order of that after maprotiline. Our results indicate that mianserin kinetics are in most respects similar to those of tertiary amine tricyclic antidepressants (e.g., imipramine) and the tetracyclic maprotiline.
PMID:6851406 Hrdina PD et al; Clin Pharmacol Ther 33 (6): 757-62 (1983)
Hepatic.
Mianserin metabolism was studied in female humans, rabbits, and rats. ... In human females, unchanged mianserin, 8-hydroxymianserin and mianserin-2-oxide were isolated and identified in urine. The two metabolites were over 60 percent of the total urinary radioactivity; conjugated and unconjugated mianserin accounted for approximately 35 percent. In rabbits, mianserin was metabolized largely as 8-hydroxymianserin and an unidentified ester of 8-hydroxymianserin; only about 2.4 percent was unchanged mianserin. Small amounts of 2-formyldesmethylmianserin were isolated. The principal metabolite in rats was 8-hydroxydesmethylmianserin. Rats metabolized mianserin principally to 8-hydroxy compounds and to a lesser extent to demethylated metabolites. The authors conclude that mianserin is metabolized by three main pathways: 8-hydroxylation, demethylation, and 2-oxide formation. /Mianserin HCl/
De Jongh GD Drug Metabolism and Disposition 9 (1): 48-53 (1981)
To measure steady-state plasma concentrations of mianserin and its major active metabolite, desmethylmianserin, and to analyze the effects of various clinical factors on these plasma concentrations, steady-state plasma concentrations of mianserin and desmethylmianserin were measured in 76 depressed patients, ages 20-70 yr, receiving 30 mg/day mianserin at bedtime for 3 wk with doses increased up to 60 mg/day if needed. There were considerable interindividual variations in the steady-state plasma concentrations of these compounds; the plasma concentrations of mianserin plus desmethylmianserin were within the therapeutic range in only 43% of the patients. With advancing age, the plasma concentrations of mianserin increased significantly, while those of mianserin plus desmethylmianserin remained unchanged. Sex, smoking, and coadministration of benzodiazepines did not affect the drug's metabolism. There was no evidence that the kinetics of these compounds were nonlinear with increasing doses.
Otani K et al; Ther. Drug Monit 15 (2): 113-7 (1983)
Mianserine has known human metabolites that include 8-Hydroxymianserin, Desmethylmianserin, and Mianserin N-oxide.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
10-17 hours
The pharmacokinetics of mianserin hydrochloride have been determined in eight normal healthy volunteers, mean age 27, and 14 elderly patients, mean age 76. Mianserin was administered to volunteers by intravenous infusion (0.011 mg/kg/min for 15 min) and, on another occasion, by mouth, in a single dose of 30 mg. Elderly patients received a single oral dose of 40-60 mg. The terminal elimination half-life was significantly prolonged in the elderly. In young subjects it was 9.6 +/- 1.9 (s.d.) hr. In the elderly it was 27 +/- 13.1 (s.d.) hr. Apparent oral clearance was significantly reduced in the elderly. In young subjects it was 87.1 +/- 32 (s.d.) hr. In the elderly, it was 38.1 +/- 14.8 (s.d.) hr. These kinetic differences may have an important bearing on the sedative effects of mianserin.
Shami M et al; Br J Clin Pharmacol 15 (Suppl 2): 313S-322S (1983)
Mianserin's mechanism of therapeutic action is not well understood, although it apparently blocks alpha-adrenergic, histamine H1, and some types of serotonin receptors.