1. Chloride, Morphine
2. Contin, Ms
3. Duramorph
4. Morphia
5. Morphine Chloride
6. Morphine Sulfate
7. Morphine Sulfate (2:1), Anhydrous
8. Morphine Sulfate (2:1), Pentahydrate
9. Ms Contin
10. Oramorph Sr
11. Sdz 202 250
12. Sdz 202-250
13. Sdz 202250
14. Sdz202 250
15. Sdz202-250
16. Sdz202250
17. Sulfate, Morphine
1. Morphia
2. Morphium
3. Morphinum
4. Morphin
5. (-)-morphine
6. Ospalivina
7. Morphina
8. 57-27-2
9. Duromorph
10. Meconium
11. Morphinism
12. Moscontin
13. Nepenthe
14. Ms Contin
15. L-morphine
16. Depodur
17. Dulcontin
18. Morfina
19. Roxanol
20. Morphine Sulfate
21. Dreamer
22. Morpho
23. Avinza
24. Hocus
25. Kadian
26. Unkie
27. Cube Juice
28. Hard Stuff
29. Statex Sr
30. Ms Emma
31. Morphin [german]
32. Morfina [italian]
33. Infumorph
34. Morphina [italian]
35. M-eslon
36. Anhydrous Morphine
37. Morphine [ban]
38. Ccris 5762
39. Hsdb 2134
40. Morphine Anhydrous
41. (5r,6s,9r,13s,14r)-4,5-epoxy-n-methyl-7-morphinen-3,6-diol
42. Sevredol
43. Morphine (anhydrous)
44. Chebi:17303
45. N02aa01
46. Morphine Extended Release
47. Chembl70
48. (5alpha,6alpha)-17-methyl-7,8-didehydro-4,5-epoxymorphinan-3,6-diol
49. 4,5alpha-epoxy-17-methyl-7-morphinen-3,6alpha-diol
50. 7,8-didehydro-4,5-epoxy-17-methyl-morphinan-3,6-diol
51. Ids-nm-009
52. (7r,7as,12bs)-3-methyl-2,3,4,4a,7,7a-hexahydro-1h-4,12-methano[1]benzofuro[3,2-e]isoquinoline-7,9-diol
53. Morphine Anhydrate
54. 76i7g6d29c
55. Morphine (ban)
56. Oramorph
57. Rms
58. (5alpha,6alpha)-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol
59. Morphinan-3,6-alpha-diol, 7,8-didehydro-4,5-alpha-epoxy-17-methyl-
60. Morphinan-3,6-diol, 7,8-didehydro-4,5-epoxy-17-methyl-, (5alpha,6alpha)-
61. (4r,4ar,7s,7ar,12bs)-3-methyl-2,4,4a,7,7a,13-hexahydro-1h-4,12-methanobenzofuro[3,2-e]isoquinoline-7,9-diol
62. Methyl[?]diol
63. Aguettant
64. Dinamorf
65. Dimorf
66. (5alpha,6alpha)-7,8-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol
67. Moi
68. D-(-)-morphine
69. 9h-9,9c-iminoethanophenanthro(4,5-bcd)furan-3,5-diol, 4a,5,7a,8-tetrahydro-12-methyl-
70. Einecs 200-320-2
71. Unii-76i7g6d29c
72. Dea No. 9300
73. (morphine)
74. Morphine Polistirex
75. Substitol (tn)
76. Mor
77. (-)-(etorphine)
78. (-)morphine Sulfate
79. Morfina Dosa (tn)
80. Nsc11441
81. Morphine [hsdb]
82. Morphine [mi]
83. Morphine [vandf]
84. Morphine [mart.]
85. Epitope Id:116646
86. Morphine [who-dd]
87. Schembl2997
88. Bidd:gt0147
89. Gtpl1627
90. (5.alpha.,6.alpha.)-7,8-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol
91. Dtxsid9023336
92. Morphine 0.1 Mg/ml In Methanol
93. Morphine 1.0 Mg/ml In Methanol
94. Zinc3812983
95. Bdbm50000092
96. Morphine (anhydrous) [vandf]
97. Akos015966554
98. Db00295
99. C01516
100. D08233
101. Hydromorphone Hydrochloride Impurity, Morphine-
102. Q81225
103. Codeine Monohydrate Impurity B [ep Impurity]
104. 7,8-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol
105. Hydromorphone Hydrochloride Impurity C [ep Impurity]
106. 17-methyl-7,8-didehydro-4,5alpha-epoxymorphinan-3,6alpha-diol
107. Codeine Hydrochloride Dihydrate Impurity B [ep Impurity]
108. Codeine Phosphate Hemihydrate Impurity B [ep Impurity]
109. Codeine Phosphate Sesquihydrate Impurity B [ep Impurity]
110. 7,8-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol(morphine)
111. Dihydrocodeine Hydrogen Tartrate Impurity B [ep Impurity]
112. (5alpha,6beta)-17-methyl-7,8-didehydro-4,5-epoxymorphinan-3,6-diol
113. 3-(4-hydroxy-phenyl)-1-propyl-piperidine-3-carboxylic Acid Ethyl Ester
114. 4,5.alpha.-epoxy-17-methyl-7,8-didehydromorphinan-3,6.alpha.-dio
115. 6-tert-butyl-3-methyl-1,2,3,4,5,6-hexahydro-2,6-methano-benzo[d]azocine
116. 7,8-didehydro-4,5.alpha.-epoxy-17-methylmorphinan-3,6.alpha.-diol
117. Apomorphine Hydrochloride Hemihydrate Impurity B [ep Impurity]
118. Hydrocodone Hydrogen Tartrate 2.5-hydrate Impurity A [ep Impurity]
119. Hydromorphone Hydrochloride Impurity, Morphine- [usp Impurity]
120. (-)(5.alpha.,6.alpha.)-7,8-didehydro-4,5-epoxy-17-methylmorphinan-3,6-diol
121. Morphinan-3,6-diol, 7,8-didehydro-4,5-epoxy-17-methyl, (5.alpha.,6.alpha.)-
122. Morphinan-3,6-diol, 7,8-didehydro-4,5-epoxy-17-methyl- (5..alpha.,6.alpha.)-
123. Morphine Solution, 1.0 Mg/ml In Methanol, Ampule Of 1 Ml, Certified Reference Material
124. (1s,5r,13r,14s)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol
125. (1s,5r,13r,14s,17r)-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0?,??.0?,??.0?,??]octadeca-7,9,11(18),15-tetraene-10,14-diol
126. (1s,5r,13r,14s,17r)-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0^{1,13}.0^{5,17}.0^{7,18}]octadeca-7(18),8,10,15-tetraene-10,14-diol
127. (1s,5r,13r,14s,17r)-4-methyl-12-oxa-4-azapentacyclo[9.6.1.0^{1,13}.0^{5,17}.0^{7,18}]octadeca-7,9,11(18),15-tetraene-10,14-diol
128. (morphine) 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol
129. 2-{4-[2,4-diamino-6-pteridinylmethyl(methyl)amino]phenylcarboxamido}pentanedioic Acid(morphine)
130. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol
131. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol ; Hydrochloride
132. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol ;sulphate Salt(morphine)
133. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol((morphine))
134. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol(morphine Sulfate)
135. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol(morphine)
136. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol(morphine)(hcl)
137. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol,sulfate(morphinesulfate)
138. 4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diolmorphine
139. 4-methyl-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol
140. 4-methyl-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol (morphine)
141. 4-methyl-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol(morphine)
142. 6,11-dimethyl-3-(3-methyl-but-2-enyl)-1,2,3,4,5,6-hexahydro-2,6-methano-benzo[d]azocin-8-ol(morphine)
143. 9h-9,9c-iminoethanophenanthro(4,5-bcd)furan-3,5-diol, 4alpha,5,7alpha,8-tetrahydro-12-methyl-
144. Morphine; (5a,6a)-7,8-didehydro-4,5-epoxy-17-methylmorphinian-3,6-diol; Morphium; Morphia; Dolcontin; Duromorph; Morphina; Nepenthe
145. Morphine;4-methyl-(1s,5r,13r,14s,17r)-12-oxa-4-azapentacyclo[9.6.1.01,13.05,17.07,18]octadeca-7(18),8,10,15-tetraene-10,14-diol
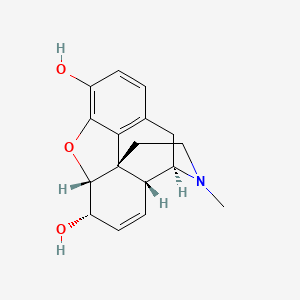
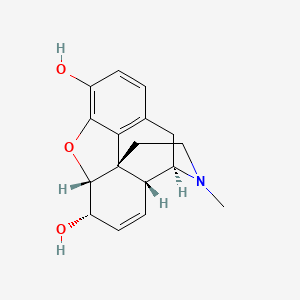
| Molecular Weight | 285.34 g/mol |
|---|---|
| Molecular Formula | C17H19NO3 |
| XLogP3 | 0.8 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 0 |
| Exact Mass | 285.13649347 g/mol |
| Monoisotopic Mass | 285.13649347 g/mol |
| Topological Polar Surface Area | 52.9 Ų |
| Heavy Atom Count | 21 |
| Formal Charge | 0 |
| Complexity | 494 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 5 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Analgesics, Opioid; Narcotics
National Library of Medicine's Medical Subject Headings. Morphine. Online file (MeSH, 2016). Available from, as of August 12, 2016: https://www.nlm.nih.gov/mesh/2016/mesh_browser/MBrowser.html
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Morphine is included in the database.
NIH/NLM; ClinicalTrials.Gov. Available from, as of March 17, 2016: https://clinicaltrials.gov/ct2/results?term=morphine&Search=Search
The primary objective was to determine whether oral morphine sulfate contributed to decreased length of stay, both in the hospital and neonatal intensive care unit (NICU), when compared to oral methadone for the treatment of neonatal abstinence syndrome (NAS). Secondary objectives included evaluation of NAS scores, opioid requirements, use of adjuvant therapy, and total cost of hospital stay. An equal number of neonates who received oral morphine sulfate and oral methadone as treatment for NAS were identified. Inclusion criteria included in utero exposure to opioids as determined by maternal history, toxicology reports during pregnancy or at the time of delivery, or infant urine toxicology reports and symptoms of NAS requiring pharmacological treatment. Exclusion criteria included neonates transferred to or from another facility during treatment, neonates discharged on NAS treatment, and neonates diagnosed with iatrogenic NAS due to postnatal exposure to opioids. Twenty six neonates met inclusion criteria. Statistically significant decreases in length of hospital and NICU stay, length of treatment, maximum opioid requirements, and total cost were found when neonates treated for NAS with oral morphine sulfate were compared to those treated with oral methadone. No statistically significant differences in average maximum NAS score or use of adjuvant therapy were found between the two groups. Oral morphine sulfate reduced length of NICU and hospital stay, length of treatment, and total cost of treatment for neonates treated for NAS.
PMID:26582303 Young ME et al; Am J Health Syst Pharm 72 (23 Suppl 3): S162-7 (2015)
We have conducted a meta-analysis of the clinical effects of morphine and hydromorphone to compare their benefit in analgesia. Embase and Medline were searched with an end-date of June 2009 for randomized, controlled trials or observational studies that addressed comparative analgesic and side-effects or particular side-effects. Two researchers independently identified included studies and extracted the data. Estimates of opioid effects were combined by using a random-effects model. Meta-analysis of eight studies suggested that hydromorphone (494 patients) provides slightly better (P=0.012) clinical analgesia than morphine (510 patients). The effect-size was small (Cohen's d=0.266) and disappeared when one study was removed, although the advantage of hydromorphone was more evident in studies of better quality (Jadad's rating). Side-effects were similar, for example, nausea (P=0.383, nine studies, 456 patients receiving hydromorphone and 460 morphine); vomiting (P=0.306, six studies, 246 patients receiving hydromorphone and 239 morphine); or itching (P=0.249, eight studies, 405 patients receiving hydromorphone, 410 morphine). This suggests some advantage of hydromorphone over morphine for analgesia. Additional potential clinical pharmacological advantages with regard to side-effects, such as safety in renal failure or during acute analgesia titration, are based on limited evidence and require substantiation by further studies.
PMID:21841049 Felden L et al; Br J Anaesth 107 (3): 319-28 (2011)
For more Therapeutic Uses (Complete) data for MORPHINE (10 total), please visit the HSDB record page.
The U.S. Food and Drug Administration (FDA) is warning about several safety issues with the entire class of opioid pain medicines. These safety risks are potentially harmful interactions with numerous other medications, problems with the adrenal glands, and decreased sex hormone levels. We are requiring changes to the labels of all opioid drugs to warn about these risks. Opioids can interact with antidepressants and migraine medicines to cause a serious central nervous system reaction called serotonin syndrome, in which high levels of the chemical serotonin build up in the brain and cause toxicity. Taking opioids may lead to a rare, but serious condition in which the adrenal glands do not produce adequate amounts of the hormone cortisol. Cortisol helps the body respond to stress. Long-term use of opioids may be associated with decreased sex hormone levels and symptoms such as reduced interest in sex, impotence, or infertility.
FDA; FDA Drug Safety Communication: FDA Warns About Several Safety Issues with Opioid Pain Medicines; Requires Label Changes (March 22, 2016). Available from, as of March 22, 2016: https://www.fda.gov/Drugs/DrugSafety/ucm489676.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery
In a continuing effort to educate prescribers and patients about the potential risks related to opioid use, the U.S. Food and Drug Administration today announced required class-wide safety labeling changes for immediate-release (IR) opioid pain medications. Among the changes, the FDA is requiring a new boxed warning about the serious risks of misuse, abuse, addiction, overdose and death. Today's actions are among a number of steps the agency recently outlined in a plan to reassess its approach to opioid medications. The plan is focused on policies aimed at reversing the epidemic, while still providing patients in pain access to effective relief.
FDA; FDA News Release: FDA Announces Enhanced Warnings for Immediate-Release Opioid Pain Medications Related to Risks of Misuse, Abuse, Addiction, Overdose and Death (March 22, 2016). Available from, as of March 22, 2016 https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm491739.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery
CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016; This guideline provides recommendations for primary care clinicians who are prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. The guideline addresses 1) when to initiate or continue opioids for chronic pain; 2) opioid selection, dosage, duration, follow-up, and discontinuation; and 3) assessing risk and addressing harms of opioid use. CDC developed the guideline using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework, and recommendations are made on the basis of a systematic review of the scientific evidence while considering benefits and harms, values and preferences, and resource allocation. CDC obtained input from experts, stakeholders, the public, peer reviewers, and a federally chartered advisory committee. It is important that patients receive appropriate pain treatment with careful consideration of the benefits and risks of treatment options. This guideline is intended to improve communication between clinicians and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder, overdose, and death.
Dowell D et al; Morbidity and Mortality Weekly Report (MMWR) 65 (1):1-49 (2016); Available from, as of March 22, 2016: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm
Caution should be taken to avoid the use of morphine preparations with preservatives in intrathecal or epidural use.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 768
For more Drug Warnings (Complete) data for MORPHINE (17 total), please visit the HSDB record page.
The mean morphine blood level in 10 fatalities was 0.2 to 2.3 ug/g. After an overdose of morphine sulfate, a 14-year-old girl had a plasma morphine concentration of 0.5 ug/mL. She developed an atypical leukoencephalopathy.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 769
Morphine leads to death in amounts of 0.15-0.2 g (sc) or 0.3-0.4g (oral) in adults. Babies and young children are much more susceptible, and death has been observed at doses of 30 mg.
Harvey, A.L. (ed.). Natural and Synthetic Neurotoxins. London, England: Academic Press 1993., p. 263
Toxic morphine blood concentration: 10-100 ug/dL; Lethal morphine blood concentration: > 400 ug/dL /From table/
Gossel, T.A., J.D. Bricker. Principles of Clinical Toxicology. 3rd ed. New York, NY: Raven Press, Ltd., 1994., p. 421
Morphine is used for the management of chronic, moderate to severe pain. Opiods, including morphine, are effective for the short term management of pain. Patients taking opioids long term may need to be monitored for the development of physical dependence, addiction disorder, and drug abuse.
FDA Label
Morphine binding to opioid receptors blocks transmission of nociceptive signals, signals pain-modulating neurons in the spinal cord, and inhibits primary afferent nociceptors to the dorsal horn sensory projection cells. Morphine has a time to onset of 6-30 minutes. Excess consumption of morphine and other opioids can lead to changes in synaptic neuroplasticity, including changes in neuron density, changes at postsynaptic sites, and changes at dendritic terminals. Intravenous morphine's analgesic effect is sex dependent. The EC50 in men is 76ng/mL and in women is 22ng/mL. Morphine-6-glucuronide is 22 times less potent than morphine in eliciting pupil constriction.
Narcotics
Agents that induce NARCOSIS. Narcotics include agents that cause somnolence or induced sleep (STUPOR); natural or synthetic derivatives of OPIUM or MORPHINE or any substance that has such effects. They are potent inducers of ANALGESIA and OPIOID-RELATED DISORDERS. (See all compounds classified as Narcotics.)
Analgesics, Opioid
Compounds with activity like OPIATE ALKALOIDS, acting at OPIOID RECEPTORS. Properties include induction of ANALGESIA or NARCOSIS. (See all compounds classified as Analgesics, Opioid.)
N02AA01
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
N02AA01
S66 | EAWAGTPS | Parent-Transformation Product Pairs from Eawag | DOI:10.5281/zenodo.3754448
N - Nervous system
N02 - Analgesics
N02A - Opioids
N02AA - Natural opium alkaloids
N02AA01 - Morphine
Absorption
Morphine is absorbed in the alkaline environments of the upper intestine and rectal mucosa. The bioavailability of morphine is 80-100%. There is significant first-pass metabolism, therefore oral doses are 6 times larger than parenteral doses to achieve the same effect. Morphine reaches steady-state concentrations after 24-48 hours. Parenteral morphine has a Tmax of 15 minutes and oral morphine has a Tmax of 90 minutes, with a Cmax of 283nmol/L. The AUC of morphine is 225-290nmol\*h/L.
Route of Elimination
70-80% of an administered dose is excreted within 48 hours. Morphine is predominantly eliminated in the urine with 2-10% of a dose recovered as the unchanged parent drug. 7-10% of a dose of morphine is eliminated in the feces.
Volume of Distribution
The volume of distribution of morphine is 5.31L/kg. Morphine-6-glucuronide has a volume of distribution of 3.61L/kg.
Clearance
The apparent clearance of intravenous or subcutaneous morphine is 1600 mL/min.
Morphine crosses the placenta at term. ... Pregnant patients in labor clear the parent compound almost twice as fast. Infants younger than 1 month of age have prolonged half-life of morphine compared to older children. The clearance of morphine approaches adult values in the second month of life. The milk to plasma ratio of morphine is 2.5:1. Although significant infant plasma levels may develop, breast-feeding can usually be performed safely. A breast-feeding infant may absorb 0.8% to 12% of the maternal dose.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 768
Morphine sulfate is variably absorbed from the GI tract. Food may increase the extent of GI absorption of morphine sulfate administered as conventional preparations. Food may decrease the rate of absorption of morphine sulfate administered as extended-release capsules; however, the extent of absorption of the drug does not appear to be affected.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2234
Following administration of single 10-mg doses of morphine sulfate as an oral solution or rectal suppository in one study in a limited number of patients with pain associated with cancer, absorption of the drug from the rectal suppository was greater than that from the oral solution over a 4.5-hour period after administration. Oral bioavailability and average plasma concentrations at steady state reportedly are similar following oral administration of morphine sulfate as conventional or extended-release preparations. However, lower peak and higher trough plasma concentrations of morphine may occur with administration of some extended-release tablets and capsules compared with conventional morphine sulfate formulations. In patient-controlled analgesia studies, the minimum analgesic plasma concentration of morphine was determined to be 20-40 ng/mL.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2234
Peak analgesia occurs within 60 minutes following oral administration of conventional preparations of the drug, and analgesia occurs within 20-60 minutes after rectal administration. Peak analgesia occurs within 50-90 minutes following subcutaneous injection, 30-60 minutes after IM injection, and 20 minutes after IV injection. Analgesia may be maintained up to 7 hours. Following IM administration of morphine sulfate, maximal respiratory depression occurs within 30 minutes. Maximal respiratory depression following IV and subcutaneous injection occurs within 7 minutes and 90 minutes, respectively. Sensitivity of the respiratory center returns to normal within 2-3 hours, but respiratory minute volume may remain below normal for 4-5 hours.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2234
For more Absorption, Distribution and Excretion (Complete) data for MORPHINE (19 total), please visit the HSDB record page.
Morphine is 90% metabolized by glucuronidation by UGT2B7 and sulfation at positions 3 and 6. Morphine can also be metabolized to codeine, normorphine, and morphine ethereal sulfate.
... patients on therapeutic codeine also test positively for morphine, because morphine is a codeine metabolite.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 769
/Heroin/ is converted metabolically by ester hydrolysis first to 6-monoacetylmorphine (heroin-specific metabolite) and then to morphine by hydrolysis for the second acetate ester. When the heroin base enters the body, it is fairly lipophilic, so a portion of the dose readily crosses the blood-brain barrier into the central nervous system where the hydrolysis of the two esters can take place. Morphine is less lipophilic than heroin and does not cross back across the blood-brain barrier as readily. Morphine readily undergoes the additional phase I metabolic transformation of oxidative N-demethylation by CYP2D6. Phase II (conjugation) reactions of morphine include formation of the glucuronide conjugates at the hydroxyl moieties at positions 3 and 6. The glucuronides are then excreted. Note that the aromatic ring stays intact throughout the metabolic transformations, illustrating the stability imparted by aromaticity.
Dart, R.C. (ed). Medical Toxicology. Third Edition, Lippincott Williams & Wilkins. Philadelphia, PA. 2004., p. 370
Morphine is metabolized principally in the liver and undergoes conjugation with glucuronic acid principally at the 3-hydroxyl group. Secondary conjugation also occurs at the 6-hydroxyl group to form the 6-glucuronide, which is pharmacologically active, and to a limited extent the 3,6-diglucuronide. Plasma concentrations of the 3-glucuronide, which is inactive, and the 6-glucuronide substantially exceed those of unchanged drug, and the latter metabolite appears to contribute substantially to the drug's pharmacologic activity. Elimination of the drug may be reduced substantially in neonates compared with older children and adults. Morphine is excreted in urine mainly as morphine-3-glucuronide. In addition to the 3,6-diglucuronide, other minor metabolites that have been described includes normorphine and the 3-ethereal sulfate. ... In patients with renal impairment, accumulation of morphine-6-glucuronide occurs, which can result in enhanced and prolonged opiate activity.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2235
The major pathway for the metabolism of morphine is conjugation with glucuronic acid. The two major metabolites formed are morphine-6-glucuronide and morphine-3-glucuronide. Small amounts of morphine-3,6-diglucuronide also may be formed.
Brunton, L. Chabner, B, Knollman, B. Goodman and Gillman's The Pharmaceutical Basis of Therapeutics, Twelth Edition, McGraw Hill Medical, New York, NY. 2011, p. 499
For more Metabolism/Metabolites (Complete) data for MORPHINE (12 total), please visit the HSDB record page.
Morphine has known human metabolites that include (2S,3S,4S,5R)-6-[[(4R,4Ar,7S,7aR,12bS)-7-hydroxy-3-methyl-2,4,4a,7,7a,13-hexahydro-1H-4,12-methanobenzofuro[3,2-e]isoquinolin-9-yl]oxy]-3,4,5-trihydroxyoxane-2-carboxylic acid and (2S,3S,4S,5R)-6-[[(4R,4Ar,7S,7aR,12bS)-9-hydroxy-3-methyl-2,4,4a,7,7a,13-hexahydro-1H-4,12-methanobenzofuro[3,2-e]isoquinolin-7-yl]oxy]-3,4,5-trihydroxyoxane-2-carboxylic acid.
Morphine is a known human metabolite of codeine.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
Morphine has a half life of 2-3 hours.
... The mean terminal half-life of morphine following epidural injection is 90 minutes (range: 39-349 minutes), which is similar to the half-life of the drug reported after IV or IM administration (1.5-4.5 hours).
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2235
CSF concentrations of morphine decline in a biphasic manner following epidural injection of conventional morphine sulfate injection, with an early distribution half-life of 1.5 hours and a terminal half-life of about 6 hours.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2235
Following epidural administration of a 10-, 15-, or 20-mg dose of morphine sulfate extended-release liposomal injection, the half-life reportedly is 16.2, 20, or 23.9 hours, respectively.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2235
Following intrathecal administration of /morphine/, the mean reported CSF half-life is 90 minutes (range: 42-136 minutes).
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 2235
For more Biological Half-Life (Complete) data for MORPHINE (6 total), please visit the HSDB record page.
Morphine-6-glucuronide is responsible for approximately 85% of the response observed by morphine administration. Morphine and its metabolites act as agonists of the mu and kappa opioid receptors. The mu-opioid receptor is integral to morphine's effects on the ventral tegmental area of the brain. Morphine's activation of the reward pathway is mediated by agonism of the delta-opioid receptor in the nucleus accumbens, while modification of the respiratory system and addiction disorder are mediated by agonism of the mu-opioid receptor.
Visual analysis of the direct electroencephalograph has revealed that morphine /slowed/ the predominant frequency and /increased/ high-voltage delta activity.
Khazan N; p.173-215 in Methods in Narcotics Research; Ehrempresis S, Neidle A, eds (1981) as cited in DHHS/NIDA; Research Monograph Series 52: Testing Drugs for Physical Dependence Potential and Abuse Liability p.30 (1984) DHHS Pub No. (ADM)87-1332