1. 1-39 Acth
2. Acth
3. Acth (1-39)
4. Adrenocorticotrophic Hormone
5. Adrenocorticotropic Hormone
6. Adrenocorticotropin
7. Corticotrophin
8. Corticotrophin (1-39)
9. Corticotropin (1-39)
10. Hormone, Adrenocorticotrophic
11. Hormone, Adrenocorticotropic
1. Cortrophin
2. 9002-60-2
3. Adrenocorticotropin
4. Acth (1-39)
5. 12427-33-7
6. Adrenocorticotropic Hormone (1-39), Human
7. Acthargel
8. Beta-corticotropin
9. H.p. Acthar Gel
10. Corticotropin [usp:inn]
11. Unii-k0u68q2txa
12. K0u68q2txa
13. Acth (1-39) (human)
14. Chebi:3892
15. Bdbm82408
16. Acth-(1-39)
17. 25-asp-30-gln-corticotropin Porcine
18. Ncgc00167127-01
19. Cas_12279-41-3
20. Sysmehfrwgkpvgkkrrpvkvypdgaedqlaeafplef
21. Sysmehfrwgkpvgkkrrpvkvypngaedesaeafplef-oh
22. J-004856
23. Alpha1-39-corticotropin (swine), 25-l-aspartic Acid-30-l-glutamine
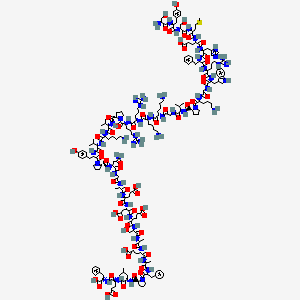
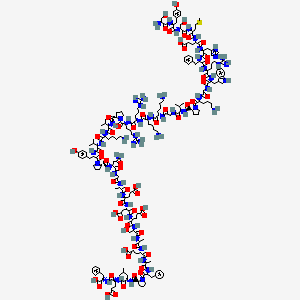
24. H-ser-tyr-ser-met-glu-his-phe-arg-trp-gly-lys-pro-val-gly-lys-lys-arg-arg-pro-val-lys-val-tyr-pro-asn-gly-ala-glu-asp-glu-ser-ala-glu-ala-phe-pro-leu-glu-phe-oh
| Molecular Weight | 4541 g/mol |
|---|---|
| Molecular Formula | C207H308N56O58S |
| XLogP3 | -19.7 |
| Hydrogen Bond Donor Count | 63 |
| Hydrogen Bond Acceptor Count | 68 |
| Rotatable Bond Count | 148 |
| Exact Mass | 4540.2660828 g/mol |
| Monoisotopic Mass | 4538.2593732 g/mol |
| Topological Polar Surface Area | 1860 Ų |
| Heavy Atom Count | 322 |
| Formal Charge | 0 |
| Complexity | 11200 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 36 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Corticotropin is used as an aid in the diagnosis of adrenocortical insufficiency. /Use Included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Corticotropin has been used in patients with normal adrenocortical function for its anti-inflammatory and immunosuppressant properties and its effect on blood and lymphatic systems in the palliative treatment of various nonendocrine disorders that are responsive to glucocorticoids. /Use Included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
In patients with normal adrenocortical function, corticotropin has been used for its anti-inflammatory and immunosuppressant properties and its effects on blood and lymphatic systems in the palliative treatment of various nonendocrine disorders that are responsive to glucocorticoids. /Use Included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 3291
Corticotropin has been used effectively in patients with moderately to severly active and severe fulminant Crohn's disease, including those with an abdominal mass, when a parenteral corticosteroid was indicated, usually in patients who have not responded to oral therapy. Individuals with an inflammatory abdominal mass should receive broad-spectrum anti-infective agents in conjunction with corticotropin. /Use not currently Included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 3291
Corticotropin may be used in the palliative treatment of various nonendocrine disorders that are responsive to glucocorticoids. Corticotropin also may be used in the symptomatic treatment of acute exacerbations of multiple sclerosis or other neuromuscular disorders such as dermatomyositis. Corticotropin therapy is not curative and is indicated only as supportive therapy to be used adjunctively with other indicated therapies. If prolonged therapy is required, continual attempts should be made to reduce the dosage or, preferably, to withdraw corticotropin therapy completely. /Use Included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 3291
After IM or subcutaneous administration of corticotropin, transient local induration, pain, and abscesses may occur at the injection site.
American Industrial Hygiene Association; Emergency Response Planning Guidelines & Workplace Enviromental Exposure Levels. Fairfax, VA 2009
Hypersensitivity to corticotropin has occurred, even in patients who have not previously been treated with the drug. Cosyntropin is less antigenic and is less likely to produce allergic reactions than is corticotropin, but hypersensitivity reactions have occurred rarely. Hypersensitivity to corticotropin may be manifested by skin reactions (urticaria, pruritus, scarlatiniform exanthema), dizziness, nausea, vomiting, and mild fever and, in some instances, anaphylactic shock, wheezing, circulatory failure, and death. Anaphylactic reactions should be treated immediately with IV epinephrine; less severe hypersensitivity reactions may be treated with IV or IM administration of a corticosteroid. Hypersensitivity may be caused by an impurity in the corticotropin preparation or the drug itself. Before administering corticotropin in patients with suspected sensitivity to porcine proteins, hypersensitivity skin testing should be performed. To decrease the risk of anaphylactic reactions in patients with limited adrenal reserves (especially primary adrenocortical insufficiency), 1 mg of dexamethasone may be given at midnight before the corticotropin test and 0.5 mg at the start of the test. During IV administration or immediately after IM or subcutaneous injection of corticotropin preparations, all patients should be carefully observed for hypersensitivity reactions. Some patients who are hypersensitive to corticotropin preparations may be able to tolerate cosyntropin, but cross-sensitivity reactions may occur.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Except for hypersensitivity reactions, short-term administration of corticotropin, even in massive doses, is unlikely to produce harmful effects. When the drug is used for longer than brief periods, however, it can produce a variety of devastating effects.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Patients receiving cortisone or hydrocortisone on the test day may exhibit abnormally high baseline plasma cortisol concentrations and a paradoxical decrease in plasma cortisol concentrations following administration of corticotropin. Patients receiving estrogens may have abnormally elevated plasma cortisol concentrations before and after corticotropin administration, but a normal incremental response to corticotropin still occurs.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
For more Drug Warnings (Complete) data for Corticotropin (29 total), please visit the HSDB record page.
For use as a diagnostic agent in the screening of patients presumed to have adrenocortical insufficiency. Purified corticotropin for injection is indicated for a variety of allergic and autoimmune conditions.
Corticotropin acts through the stimulation of cell surface ACTH receptors, which are primarily located on the adrenocortical cells. Corticotropin stimulates the cortex of the adrenal gland and boosts the synthesis of corticosteroids, mainly glucocorticoids but also sex steroids (androgens). Corticotropin is also related to the circadian rhythm in many organisms.
Hormones
Chemical substances having a specific regulatory effect on the activity of a certain organ or organs. The term was originally applied to substances secreted by various ENDOCRINE GLANDS and transported in the bloodstream to the target organs. It is sometimes extended to include those substances that are not produced by the endocrine glands but that have similar effects. (See all compounds classified as Hormones.)
H - Systemic hormonal preparations, excl. sex hormones and insulins
H01 - Pituitary and hypothalamic hormones and analogues
H01A - Anterior pituitary lobe hormones and analogues
H01AA - Acth
H01AA01 - Corticotropin
Absorption
Corticotropin is rapidly absorbed following intramuscular administration; the repository dosage form is slowly absorbed over approximately 8 to 16 hours.
In the circulation, corticotropin is transported with Cohn protein fractions II and III. The precise distribution and metabolic fate of the drug is not known, but the drug is rapidly removed from the plasma by many tissues. Corticotropin apparently does not cross the placenta. Circulating corticotropin may be enzymatically cleaved at the 16-17 lysine-arginine bond by the plasmin-plasminogen system.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 3293
After IM or rapid direct IV administration of 25 units of corticotropin injection in patients with normal adrenocortical function, peak plasma cortisol concentrations are usually achieved within 1 hour and begin to decrease after 2-4 hours. In one study in healthy individuals, subcutaneous administration of 80 units of repository corticotropin injection produced peak plasma 17-hydroxycorticosteroid (17-OHCS) concentrations in 3-12 hours and baseline concentrations were attained in 10-25 hours.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Following oral administration, corticotropin is inactivated by the proteolytic enzymes of the GI tract, and the drug is ineffective when applied topically to the skin or eye. Corticotropin injection is rapidly absorbed following IM injection. Following IM administration of repository corticotropin injection, the drug is absorbed over a period of about 8-16 hours. In most adults with normal adrenocortical function, maximal adrenal stimulation is attained after infusing 1-6 units of corticotropin injection IV (no longer commercially available in the US) over a period of 8 hours. With a fixed dose, corticotropin injection stimulates more cortisol secretion if the drug is given slowly IV rather than rapidly or if given IM as the repository injection rather than as corticotropin injection. Increasing the IM or IV dose increases the duration of action. Repeated doses of IV corticotropin injection over an 8-hour period on successive days increase the responsiveness of the adrenal cortex to further stimulation by the drug. Following IM administration of 100 units of corticotropin (as the repository injection) in patients with normal adrenocortical function, approximately 100 mg of cortisol is secreted in 16 hours. Following IM or rapid direct IV administration of 25 units of corticotropin injection in patients with normal adrenocortical function, peak plasma cortisol concentrations are achieved within 1 hour and begin to decrease after 2 hours. In one study in healthy individuals, subcutaneous administration of 80 units of repository corticotropin injection produced peak plasma 17-hydroxycorticosteroid (17-OHCS) concentrations in 3-12 hours and baseline concentrations were attained in 10-25 hours.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 3293
ACTH rapidly disappears from the circulation following its IV administration ...
Novak, K.M. (ed.). Drug Facts and Comparisons2008 Edition. Wolters Kluwer Health. St. Louis, Missouri 2008., p. 446
About 15 minutes following intravenous administration.
... in humans, the plasma half life is about 15 minutes.
Novak, K.M. (ed.). Drug Facts and Comparisons2008 Edition. Wolters Kluwer Health. St. Louis, Missouri 2008., p. 446
As a diagnostic aid (adrenocortical function), corticotropin combines with a specific receptor on the adrenal cell plasma membrane. In patients with normal adrenocortical function, it stimulates the initial reaction involved in the synthesis of adrenal steroids (including cortisol, cortisone, weak androgenic substances, and a limited quantity of aldosterone) from cholesterol by increasing the quantity of cholesterol within the mitochondria. Corticotropin does not significantly increase serum cortisol concentrations in patients with primary adrenocortical insufficiency (Addison's disease). The mechanism of action of corticotropin in the treatment of infantile myoclonic seizures is unknown.
ACTH stimulates the adrenal cortex to secrete cortisol, corticosterone, aldosterone, and a number of weakly androgenic substances. Although ACTH does stimulate secretion of aldosterone, the rate is relatively independent. Prolonged administration of large doses of ACTH induces hyperplasia and hypertrophy of the adrenal cortex and continuous high output of cortisol, corticosterone, and weak androgens. The release of ACTH is under the influence of the nervous system via the corticotropin regulatory hormone released from the hypothalamus and by a negative corticosteroid feedback mechanism. Elevated plasma cortisol suppresses ACTH release.
Novak, K.M. (ed.). Drug Facts and Comparisons2008 Edition. Wolters Kluwer Health. St. Louis, Missouri 2008., p. 446
Exogenous corticotropin elicits all the pharmacologic responses usually produced by endogenous corticotropin. In patients with normal adrenocortical function, corticotropin stimulates the adrenal cortex to secrete cortisol (hydrocortisone), corticosterone, several weakly androgenic substances, and to a very limited extent aldosterone. In healthy individuals, the rate of release of corticotropin from the anterior pituitary is determined by a balance of inhibitory effects of the secretions of the adrenal cortex on the pituitary (negative corticosteroid feedback mechanism) and the excitatory effects of the nervous system. In response to neurogenic stimuli, corticotropin-releasing factor (CRF) is released from neuronal endings in the median eminence of the hypothalamus and transported in the hypophyseal-portal vessels to the anterior pituitary, where corticotropin is released. Corticotropin, via cyclic 3',5'-adenosine monophosphate (cAMP), controls the initial rate-limiting step in steroidogenesis from cholesterol and leads to the synthesis of adrenocortical hormones. Corticotropin also stimulates growth of the adrenal cortex. In high concentrations, corticotropin may have extra-adrenal effects (i.e., melanocyte stimulation, activation of tissue lipase).
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 3293