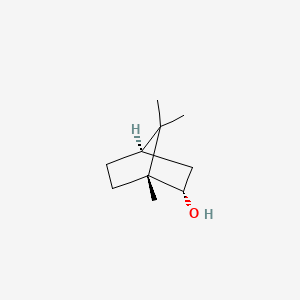
1. Isoborneol
2. Isoborneol, (1r-endo)-isomer
3. Isoborneol, (1r-exo)-isomer
4. Isoborneol, (1s-endo)-isomer
5. Isoborneol, (1s-exo)-isomer
6. Isoborneol, (endo)-isomer
7. Isoborneol, (endo-(+-))-isomer
8. Isoborneol, (exo)-isomer
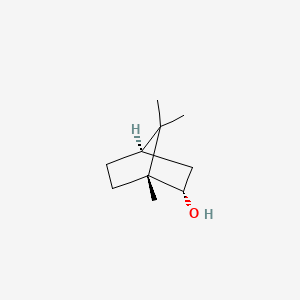
1. (+)-borneol
2. 464-43-7
3. D-borneol
4. Camphol
5. 507-70-0
6. Isoborneol
7. 2-hydroxybornane
8. 2-camphanol
9. 2-hydroxycamphane
10. (1r,2s,4r)-borneol
11. 2-bornanol, Endo-
12. 2-endo-bornyl Alcohol
13. Camphane, 2-hydroxy-
14. Dexborneol
15. Fema No. 2157
16. Hechenglongnao
17. Bingpian
18. Borneol, (+)-
19. Dl-isoborneol
20. (1r,2s,4r)-1,7,7-trimethylbicyclo[2.2.1]heptan-2-ol
21. Borneol, Dl-
22. Unii-m89nib437x
23. Borneolum Syntheticum
24. Bornyl Alcohol
25. Ccris 7300
26. Hsdb 946
27. M89nib437x
28. D-camphanol
29. Dl-borneol
30. Borneol D-form
31. Borneol, D-
32. Einecs 208-080-0
33. Bicyclo[2.2.1]heptan-2-ol, 1,7,7-trimethyl-, (1r,2s,4r)-
34. Bicyclo[2.2.1]heptan-2-ol, 1,7,7-trimethyl-, (1r,2s,4r)-rel-
35. 8d24lwt4fk
36. Borneocamphor
37. Borneo Camphor
38. Endo-(1r)-1,7,7-trimethylbicyclo[2.2.1]heptan-2-ol
39. Sumatra Camphor
40. Endo-borneol
41. Ai3-00116
42. 2-hydroxy-1,7,7-trimethylnorbornane, Endo-
43. Borneol, (+/-)-
44. 2-borneol
45. Bicyclo(2.2.1)heptan-2-ol, 1,7,7-trimethyl-, Endo-
46. Chebi:15393
47. Nsc 60223
48. 1,7,7-trimethyl-bicyclo(2.2.1)heptan-2-ol, Endo-
49. (+)?-?borneol
50. Borneol (mart.)
51. Borneol [mart.]
52. 124-76-5
53. (1r-endo)-1,7,7-trimethylbicyclo(2.2.1)heptan-2-ol
54. Endo-2-camphanol
55. Malayan Camphor
56. Baros Camphor
57. Trans-borneol
58. Bhimsaim Camphor
59. Mfcd00066427
60. Nsc-60223
61. (1r,2s,4r)-rel-1,7,7-trimethylbicyclo[2.2.1]heptan-2-ol
62. D-(+)-borneol
63. Endo-2-hydroxycamphane
64. Dryobalanops Camphor
65. (+-)-borneol
66. Unii-8d24lwt4fk
67. (1r-endo)-1,7,7-trimethylbicyclo[2.2.1]heptan-2-ol
68. Bicyclo(2.2.1)heptan-2-ol, 1,7,7-trimethyl-, (1r,2s,4r)-rel-
69. Ccris 6550
70. Mfcd00074821
71. Borneol (contains Ca. 20% Isoborneol)
72. (+)-borneol 100 Microg/ml In Methanol
73. Einecs 207-352-6
74. Endo-2-hydroxy-1,7,7-trimethylnorbornane
75. Un1312
76. (-) Borneol
77. Varicose Veins Patch
78. Brn 2038056
79. Borneol [fhfi]
80. Borneol [hsdb]
81. Borneol [fcc]
82. Enokon Pain Relief Patch
83. Borneol [mi]
84. Borneol [who-dd]
85. (+)-borneol, 97%
86. D-borneol [who-dd]
87. Schembl56713
88. Borneol D-form [mi]
89. 4-06-00-00281 (beilstein Handbook Reference)
90. Endo-1,7,7-trimethylbicyclo
91. Chembl486208
92. Gtpl6413
93. Dtxsid2058700
94. Dtxsid3052143
95. Rel-(1s,2r,4s)-1,7,7-trimethylbicyclo(2.2.1)heptan-2-ol
96. Bdbm36265
97. Hy-n1368a
98. (+)-borneol, Analytical Standard
99. Dtgkskdoiyivql-wedxcclwsa-n
100. Borneolum Syntheticum [chp]
101. Endo-(+-)-bornan-2-ol
102. Bicyclo(2.2.1)heptan-2-ol, 1,7,7-trimethyl-, (1r-endo)-
103. Ccg-36088
104. Akos016004136
105. Cs-7758
106. Borneol [un1312] [flammable Solid]
107. Bs-42578
108. Fema No. 2157, (+)-
109. Borneol (constituent Of Black Pepper)
110. Ns00080677
111. En300-84951
112. D96054
113. Pain Relief Patch-acupoint Pressure Stimulation
114. Q412435
115. Borneol (constituent Of Black Pepper) [dsc]
116. Q-100570
117. Enokon Pain Relief Patch-acupoint Pressure Stimulation
118. F0001-1255
119. Z1255372631
120. (1r,3s,4r)-4,7,7-trimethylbicyclo[2.2.1]heptan-3-ol
121. (1r,4r,6s)-1,7,7-trimethylbicyclo[2.2.1]heptan-6-ol
122. Flavor And Extract Manufacturers' Association Number 2157
| Molecular Weight | 154.25 g/mol |
|---|---|
| Molecular Formula | C10H18O |
| XLogP3 | 2.7 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 1 |
| Rotatable Bond Count | 0 |
| Exact Mass | g/mol |
| Monoisotopic Mass | g/mol |
| Topological Polar Surface Area | 20.2 |
| Heavy Atom Count | 11 |
| Formal Charge | 0 |
| Complexity | 185 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 3 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Helps relieve the local itching and discomfort associated with hemorrhoids. Temporarily shrinks hemorrhoidal tissue and relieves burning. Temporarily provides a coating for relief of anorectal discomforts. Temporarily protects the inflamed, irritated anorectal surface to help make bowel movements less painful.
DailyMed; MA YING LONG HEMORRHOIDAL- moschus artifactus, bovis calculus artifactus, margarita, borneolum syntheticum, succinum, calamina (calcined), borax ointment; Available from, as of June 24, 2016: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=59305749-d5af-412f-93d9-c20ff73ca523
For the temporary relief of minor aches and pains of muscles and joints due to: arthritis - strains - bruises - sprains - simple backaches
DailyMed; PAIN FREE - menthol, methyl salycilate, borneol ointment; Available from, as of June 24, 2016: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=b64f07b7-27ea-42d1-a2b5-08910c24b472
Antibacterial
DailyMed; SHUNFA ANTI-BACTERIA SPRA- didecyldimethyl ammonium,triclosan, borneol, benzalkonium bromide spray; Available from, as of June 24, 2016: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=92cf6f49-d10b-49da-9d36-0aaef95ad6c2
Borneol is consumed excessively in China and Southeast Asian countries particularly in combined formula for preventing cardiovascular disease, but few studies were conducted on its effects on thrombosis. In this study, the antithrombotic and antiplatelet activities of borneol were investigated on thrombosis in vivo and on platelet aggregation ex-vivo. In addition, the coagulation parameters and influence on fibrinolytic activity were also assessed. The results showed that borneol had concentration dependent inhibitory effects on arterio-venous shunt and venous thrombosis but no effect on ADP and AA-induced platelet aggregation. Meanwhile, borneol prolonged the coagulation parameters for prothrombin time (PT) and thrombin time (TT), but did not show any fibrinolytic activity. It suggested that the antithrombotic activity of borneol and its action in combined formula for preventing cardiovascular diseases might be due to anticoagulant activity rather than antiplatelet activity. /Traditional medicine/
Yan-Hong Li et al; Am. J. Chin. Med. 36: 719 (2008)
For more Therapeutic Uses (Complete) data for BORNEOL (6 total), please visit the HSDB record page.
/EXPL THER/ Isoborneol, a monoterpene and a component of several plant essential oils, showed dual viricidal activity against herpes simplex virus 1 (HSV-1). First, it inactivated HSV-1 by almost 4 log10 values within 30 min of exposure, and second, isoborneol at a concentration of 0.06% completely inhibited viral replication, without affecting viral adsorption. Isoborneol did not exhibit significant cytotoxicity at concentrations ranging between 0.016% and 0.08% when tested against human and monkey cell lines. Isoborneol specifically inhibited glycosylation of viral polypeptides based on the following data: (1) the mature fully glycosylated forms of two viral glycoproteins gB and gD were not detected when the virus was replicated in the presence of isoborneol, (2) no major changes were observed in the glycosylation pattern of cellular polypeptides between untreated and isoborneol treated Vero cells, (3) isoborneol did not affect the glycosylation of gB produced from a copy of the gB gene resident in the cellular genome, and (4) other monoterpenes such as 1,8-cineole and borneol, a stereoisomer of isoborneol, did not inhibit HSV-1 glycosylation.
PMID:10517310 Armaka M et al; Antiviral Res 43 (2): 79-92 (1999)
4. 4= Very toxic: probable oral lethal dose (human) 50-500 mg/kg, between one teaspoon and one oz for 70 kg person (150 lb).
Gosselin, R.E., H.C. Hodge, R.P. Smith, and M.N. Gleason. Clinical Toxicology of Commercial Products. 4th ed. Baltimore: Williams and Wilkins, 1976., p. II-169
To develop a GC-FID method to determine borneol's concentration in mouse tissues, and to investigate the tissue distribution after intravenous and intranasal administrations of borneol, mouse brains, hearts, livers, spleens, lungs and kidneys were collected at 1, 3, 5, 10, 20, 30, 60, 90, 120 min after administration of borneol with the dose of 30.0 mg/kg. The drug in tissues was extracted with ethyl acetate, and borneol's concentration detected by GC, with octadecane as the internal standard. The calibration curve showed a good linear relationship. Extraction recoveries, inter-day and intra-day precisions and stability were in conformity with the analytical requirements of biological samples. Borneol was mainly distributed in most tissues, more in heart, brain and kidney, and less in liver, spleen and lung. The established GC-FID method is applicable for content determination of borneol in tissues. After intravenous and intranasal administrations in mice, borneol is mainly distributed in abundant blood-supply tissues. After intranasal administration, brain tissues showed the highest target coefficient and target effectiveness.
PMID:23847960 Zhao JY et al; Zhongguo Zhong Yao Za Zhi 38 (7): 1071-4 (2013)
... In order to understand the blood and brain pharmacokinetics after intravenous, intranasal, or oral administration and to investigate the superiority and feasibility of intranasal administration, a simple gas chromatographic (GC) method with flame ionization detection (FID) was developed for the quantification of borneol. Blood samples and brain were collected from mice at 1, 3, 5, 10, 20, 30, 60, 90, and 120 min after intravenous, intranasal, or oral administration of borneol at a dosage of 30.0 mg/kg. Sample preparations were carried out by liquid-liquid extraction with an internal standard solution of octadecane. The pharmacokinetic parameters were calculated /using computer software/. The calibration curves were linear in the range of 0.11-84.24 ug/mL and 0.16-63.18 ug/g for borneol in plasma and brain, respectively. The methodological and extraction recoveries were both in the range of 85%-115%. The intra-day and inter-day variabilities for plasma and brain samples were
PMID:23225854 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3520453 Zhao JY et al; J Zhejiang Univ Sci B 13 (12): 990-6 (2012)
The aim of this work was to study the in situ and in vivo nasal absorption of borneol. A novel single pass in situ nasal perfusion technique was applied to examine the rate and extent of nasal absorption of borneol by rats. Experimental conditions, such as perfusion rate, pH and drug concentration, were investigated. The in situ experiments showed that the nasal absorption of borneol was not dependent on drug concentration, and fitted a first order process. The absorption rate constant, Ka, influenced with an increase in perfusion speed. The borneol was well absorbed in the conditions of the nasal cavity within the pH range and pH value of physiological conditions. In vivo studies of borneol absorption were carried out in rats and the pharmacokinetics parameters of intranasal (in) was compared with intravenous (iv) administration. The bioavailabilities of borneol was 90.82% for i.n. while Tmax values were 10 min. MRT (Mean Residence Time) were 262.55 +/- 67.35 min and 204.22 +/- 14.50 min for in and iv methods, respectively. The results demonstrate that borneol could be absorbed promptly and thoroughly by in administration in rats.
PMID:23136719 Song X et al; Pharmazie 67 (10): 848-51 (2012)
Previous studies have indicated that borneol has double side effects on the central nervous system (CNS), but the mechanism is unknown. The aim of this study was to clarify the relationship between excitation ratio [contents of excitatory amino acids (AAs) versus that of inhibitory] and the content of natural borneol after a single oral dose. Mice were administered a 1.2 g/kg dose of natural borneol (containing 98% D: -borneol) by oral ingestion. Brain samples were collected before administration and at 0.083, 0.167, 0.25, 0.333, 0.5, 0.75, 1, 1.5, 2, 2.5, 3, 4, and 5 hr after administration. The brain concentration of natural borneol and contents of AA neurotransmitters in mice brain were determined by GC-MS and HPLC-FLU, respectively. After per oral application, natural borneol was absorbed rapidly into the brain and could be determined 5 min after dosing. The maximal brain concentration (86.52 ug/g) was reached after 1 hr post-dosing. Natural borneol could affect the contents of AA neurotransmitters in mice brain: L: -aspartic acid increased significantly from 0.083 to 1 hr after administration, L: -glutamic acid increased significantly at 0.333 hr and decreased from 1.5 to 5 hr, gamma-amino-N-butyric acid increased significantly from 0.167 to 5 hr, whereas glycine was not affected. The excitation ratio is the contents of excitatory AAs versus that of inhibitory AAs, which reflects the excitatory or inhibitory state of the body. The excitation ratio elevated transitorily and then declined 0.5 hr post-dosing; there were significant differences between 1.5-5 hr post-dose compared with pre-dose. The present study indicated that natural borneol could affect the contents of AA neurotransmitters, and the change in excitatory ratio led to borneol's double side effects on the CNS.
PMID:21948240 Li WR et al; Eur J Drug Metab Pharmacokinet 37 (1): 39-44 (2012)
The percutaneous absorptions of camphene, isoborneol-acetate, limonene, menthol and alpha-pinene as constituents of a foam bath (Pinimenthol) were measured on animals using radioactively labeled ingredients. Pharmacokinetic measurements showed maximum blood levels for all tested ingredients 10 min after the onset of percutaneous absorption. None of the ingredients was preferentially absorbed. Blood levels of all ingredients after 10 min of percutaneous absorption were a direct function of the size of the skin area involved.
PMID:7199340 Schafer R, Schafer W; Arzneimittelforschung 32 (1): 56-8 (1982)