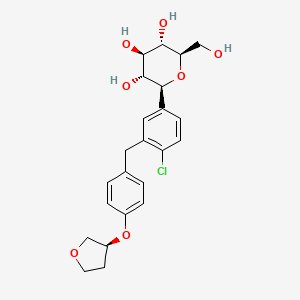
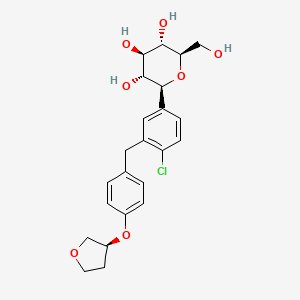
1. 1-chloro-4-(glucopyranos-1-yl)-2-(4-(tetrahydrofuran-3-yloxy)benzyl)benzene
2. Bi 10773
3. Bi-10773
4. Bi10773
5. Jardiance
1. 864070-44-0
2. Jardiance
3. Bi 10773
4. Bi-10773
5. Bi10773
6. Empagliflozin (bi 10773)
7. (2s,3r,4r,5s,6r)-2-(4-chloro-3-(4-(((s)-tetrahydrofuran-3-yl)oxy)benzyl)phenyl)-6-(hydroxymethyl)tetrahydro-2h-pyran-3,4,5-triol
8. Hdc1r2m35u
9. 1-chloro-4-(glucopyranos-1-yl)-2-(4-(tetrahydrofuran-3-yloxy)benzyl)benzene
10. Chebi:82720
11. (1s)-1,5-anhydro-1-(4-chloro-3-{4-[(3s)-tetrahydrofuran-3-yloxy]benzyl}phenyl)-d-glucitol
12. (2s,3r,4r,5s,6r)-2-[4-chloro-3-({4-[(3s)-oxolan-3-yloxy]phenyl}methyl)phenyl]-6-(hydroxymethyl)oxane-3,4,5-triol
13. (2s,3r,4r,5s,6r)-2-[4-chloro-3-[[4-[(3s)-oxolan-3-yl]oxyphenyl]methyl]phenyl]-6-(hydroxymethyl)oxane-3,4,5-triol
14. (1s)-1,5-anhydro-1-c-{4-chloro-3-((4-{((3s)-oxolan-3-yl)oxy}phenyl)methyl)phenyl}-d-glucitol
15. (2s,3r,4r,5s,6r)-2-[4-chloranyl-3-[[4-[(3s)-oxolan-3-yl]oxyphenyl]methyl]phenyl]-6-(hydroxymethyl)oxane-3,4,5-triol
16. D-glucitol, 1,5-anhydro-1-c-(4-chloro-3-((4-(((3s)-tetrahydro-3-furanyl)oxy)phenyl)methyl)phenyl)-, (1s)-
17. Empagliflozin [inn]
18. Unii-hdc1r2m35u
19. Empagliflozin [usan:inn]
20. Mfcd22566222
21. Jardiance (tn)
22. (s)-empagliflozin D4
23. Empagliflozin [mi]
24. Bi-10773;empagliflozin
25. Empagliflozin [jan]
26. Empagliflozin [usan]
27. Empagliflozin (bi10773)
28. Empagliflozin [vandf]
29. Schembl899986
30. Empagliflozin [who-dd]
31. Gtpl4754
32. Chembl2107830
33. Empagliflozin (jan/usan/inn)
34. Amy1858
35. Ex-a414
36. Bdbm150162
37. Dtxsid601026093
38. Empagliflozin [orange Book]
39. Bbl104150
40. S8022
41. Stl557964
42. Us8980829, Empagliflozin
43. Zinc36520252
44. Akos024464680
45. Glyxambi Component Empagliflozin
46. Ccg-269242
47. Cs-0940
48. Db09038
49. Ds-9824
50. Pb23119
51. (1s)-1,5-anhydro-1-c-[4-chloro-3-[[4-[[(3s)-tetrahydro-3-furanyl]oxy]phenyl]methyl]phenyl]-d-glucitol
52. Ac-27643
53. Empagliflozin Component Of Glyxambi
54. Empagliflozin Component Of Synjardy
55. Hy-15409
56. Trijardy Xr Component Empagliflozin
57. Empagliflozin Component Of Trijardy Xr
58. Sw219120-1
59. C22194
60. D10459
61. A852380
62. Au-004/43508285
63. Q5373824
64. Empagliflozin (bi-10773;bi 10773;bi10773)
65. 1,5-anhydro-1-{4-chloro-3-[4-(tetrahydro-3-furanyloxy)benzyl]phenyl}hexitol
66. (1s)-1,5-anhydro-1-c-(4-chloro-3-((4-(((3s)-oxan-3-yl)oxy)phenyl)methyl)phenyl)-d-glucitol
67. (2s,3r,4r,5s,6r)-2-(4-chloro-3-(4-((s)-tetrahydrofuran-3-yloxy)benzyl)phenyl)-6-(hydroxymethyl)-tetrahydro-2h-pyran-3,4,5-triol
68. (2s,3r,4r,5s,6r)-2-(4-chloro-3-(4-((s)-tetrahydrofuran-3-yloxy)benzyl)phenyl)-6-(hydroxymethyl)tetrahydro-2h-pyran-3,4,5-triol
69. (2s,3r,4r,5s,6r)-2-[4-chloro-3-[[4-[(3s)-tetrahydrofuran-3-yl]oxyphenyl]methyl]phenyl]-6-(hydroxymethyl)tetrahydropyran-3,4,5-triol
70. 7r3
| Molecular Weight | 450.9 g/mol |
|---|---|
| Molecular Formula | C23H27ClO7 |
| XLogP3 | 2 |
| Hydrogen Bond Donor Count | 4 |
| Hydrogen Bond Acceptor Count | 7 |
| Rotatable Bond Count | 6 |
| Exact Mass | 450.1445309 g/mol |
| Monoisotopic Mass | 450.1445309 g/mol |
| Topological Polar Surface Area | 109 Ų |
| Heavy Atom Count | 31 |
| Formal Charge | 0 |
| Complexity | 558 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 6 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Empagliflozin is indicated as an adjunct to diet and exercise to improve glycemic control in adult patients with type 2 diabetes. It is also indicated to reduce the risk of cardiovascular death in adult patients with both type 2 diabetes mellitus and established cardiovascular disease. Empagliflozin is also available as a combination product with either metformin and linagliptin as an adjunct to diet and exercise in the management of type 2 diabetes mellitus in adults. An extended-release combination product containing empagliflozin, metformin, and linagliptin was approved by the FDA in January 2020 for the improvement of glycemic control in adults with type 2 diabetes mellitus when used adjunctively with diet and exercise. Empagliflozin is also approved to reduce the risk of cardiovascular mortality and hospitalization in adults with heart failure with reduced ejection fraction regardless of whether or not the patient has concomitant diabetes. Empagliflozin is not approved for use in patients with type 1 diabetes.
Type 2 diabetes mellitus
Jardiance is indicated for the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise - as monotherapy when metformin is considered inappropriate due to intolerance - in addition to other medicinal products for the treatment of diabetes For study results with respect to combinations, effects on glycaemic control and cardiovascular events, and the populations studied, see sections 4. 4, 4. 5 and 5. 1.
Heart failure
Jardiance is indicated in adults for the treatment of symptomatic chronic heart failure.
Treatment of type I diabetes mellitus
Treatment of chronic kidney disease
Prevention of cardiovascular events in patients with chronic heart failure
Treatment of type II diabetes mellitus
Empagliflozin lowers blood glucose levels by preventing glucose reabsorption in the kidneys, thereby increasing the amount of glucose excreted in the urine. It has a relatively long duration of action requiring only once-daily dosing. Patients should be monitored closely for signs and symptoms of ketoacidosis regardless of blood glucose level as empagliflozin may precipitate diabetic ketoacidosis in the absence of hyperglycemia. As its mechanism of action is contingent on the renal excretion of glucose, empagliflozin may be held in cases of acute kidney injury and/or discontinued in patients who develop chronic renal disease. The overexcretion of glucose creates a sugar-rich urogenital environment which increases the risk of urogenital infections - including urosepsis, pyelonephritis, mycotic infections, and even Fournier's gangrene - in both male and female patients - monitor closely for signs and symptoms of developing infection.
Sodium-Glucose Transporter 2 Inhibitors
Compounds that inhibit SODIUM-GLUCOSE TRANSPORTER 2. They lower blood sugar by preventing the reabsorption of glucose by the kidney and are used in the treatment of TYPE 2 DIABETES MELLITUS. (See all compounds classified as Sodium-Glucose Transporter 2 Inhibitors.)
A10BK03
A - Alimentary tract and metabolism
A10 - Drugs used in diabetes
A10B - Blood glucose lowering drugs, excl. insulins
A10BK - Sodium-glucose co-transporter 2 (sglt2) inhibitors
A10BK03 - Empagliflozin
Absorption
Following oral administration, peak plasma concentrations are reached in approximately 1.5 hours (Tmax). At steady-state, plasma AUC and Cmax were 1870 nmolh/L and 259 nmol/L, respectively, following therapy with empagliflozin 10mg daily and 4740 nmolh/L and 687 nmol/L, respectively, following therapy with empagliflozin 25mg daily. Administration with food does not significantly affect the absorption of empagliflozin.
Route of Elimination
After oral administration of radiolabeled empagliflozin approximately 41.2% of the administered dose was found eliminated in feces and 54.4% eliminated in urine. The majority of radioactivity in the feces was due to unchanged parent drug while approximately half of the radioactivity in urine was due to unchanged parent drug.
Volume of Distribution
The estimated apparent steady-state volume of distribution is 73.8 L.
Clearance
Apparent oral clearance was found to be 10.6 L/h based on a population pharmacokinetic analysis.
Empagliflozin undergoes minimal metabolism. It is primarily metabolized via glucuronidation by 5'-diphospho-glucuronosyltransferases 2B7, 1A3, 1A8, and 1A9 to yield three glucuronide metabolites: 2-O-, 3-O-, and 6-O-glucuronide. No metabolite represented more than 10% of total drug-related material.
The apparent terminal elimination half-life was found to be 12.4 h based on population pharmacokinetic analysis.
The vast majority of glucose filtered through the glomerulus is reabsorbed within the proximal tubule, primarily via SGLT2 (sodium-glucose linked co-transporter-2) which is responsible for ~90% of the total glucose reabsorption within the kidneys. Na+/K+-ATPase on the basolateral membrane of proximal tubular cells utilize ATP to actively pump Na+ ions into the interstitium surrounding the tubule, establishing a Na+ gradient within the tubular cell. SGLT2 on the apical membrane of these cells then utilize this gradient to facilitate secondary active co-transport of both Na+ and glucose out of the filtrate, thereby reabsorbing glucose back into the blood inhibiting this co-transport, then, allows for a marked increase in glucosuria and decrease in blood glucose levels. Empagliflozin is a potent inhibitor of renal SGLT2 transporters located in the proximal tubules of the kidneys and works to lower blood glucose levels via an increase in glucosuria. Empagliflozin also appears to exert cardiovascular benefits - specifically in the prevention of heart failure - independent of its blood glucose-lowering effects, though the exact mechanism of this benefit is not precisely understood. Several theories have been posited, including the potential inhibition of Na+/H+ exchanger (NHE) 1 in the myocardium and NHE3 in the proximal tubule, reduction of pre-load via diuretic/natriuretic effects and reduction of blood pressure, prevention of cardiac fibrosis via suppression of pro-fibrotic markers, and reduction of pro-inflammatory adipokines.