1. Absolute Alcohol
2. Alcohol, Absolute
3. Alcohol, Ethyl
4. Alcohol, Grain
5. Ethyl Alcohol
6. Grain Alcohol
1. Ethyl Alcohol
2. Alcohol
3. 64-17-5
4. Grain Alcohol
5. Methylcarbinol
6. Ethyl Hydroxide
7. Ethyl Hydrate
8. Tecsol
9. Etoh
10. Algrain
11. Anhydrol
12. Hydroxyethane
13. Alkohol
14. Jaysol S
15. Potato Alcohol
16. Cologne Spirit
17. 1-hydroxyethane
18. Absolute Ethanol
19. Ethanol 200 Proof
20. Molasses Alcohol
21. Spirits Of Wine
22. Etanol
23. Aethylalkohol
24. Denatured Alcohol
25. Denatured Ethanol
26. Aethanol
27. Alcool Ethylique
28. Fermentation Alcohol
29. Alcohol, Diluted
30. Tecsol C
31. Dehydrated Ethanol
32. Alcool Etilico
33. Alcohol, Ethyl
34. Alcohols
35. Etanolo
36. Jaysol
37. Etylowy Alkohol
38. Absolute Alcohol
39. Ethanol Solution
40. Alcohol Dehydrated
41. Alkoholu Etylowego
42. Dehydrated Alcohol
43. Ethyl Alcohol Usp
44. Alcohol, Anhydrous
45. Synasol
46. Ethyl Alcohol Anhydrous
47. Denatured Alcohol Cd-5
48. Denatured Alcohol Sd-1
49. Alcohol Anhydrous
50. Distilled Spirits
51. Denatured Alcohol Cd-5a
52. Denatured Alcohol Sd-3a
53. Denatured Alcohol Cd-10
54. Denatured Alcohol Sd-17
55. Denatured Alcohol Sd-28
56. Denatured Alcohol Sd-30
57. Denatured Alcohol Sd-13a
58. Denatured Alcohol Sd-23a
59. Denatured Alcohol Sd-39b
60. Denatured Alcohol Sd-39c
61. Denatured Alcohol Sd-40m
62. Ethylalcohol
63. Spirit
64. Alcohol, Dehydrated
65. Sd Alchol 23-hydrogen
66. Alkohol [german]
67. Aethanol [german]
68. Etanolo [italian]
69. Ethyl Alcohol & Water, 5%
70. Thanol
71. Ethanol, Undenatured
72. Spirt
73. Alcare Hand Degermer
74. Ethyl Alcohol & Water, 10%
75. Ethyl Alcohol & Water, 20%
76. Ethyl Alcohol & Water, 30%
77. Ethyl Alcohol & Water, 40%
78. Ethyl Alcohol & Water, 50%
79. Ethyl Alcohol & Water, 60%
80. Ethyl Alcohol & Water, 70%
81. Ethyl Alcohol & Water, 80%
82. Ethyl Alcohol & Water, 95%
83. Ethyl Alcohol & Water, 96%
84. Ethyl Alc
85. Ethylalcohol [dutch]
86. Ethyl Alcohol And Water
87. Alcohol, Absolute
88. Nci-c03134
89. Alcohol (ethyl Alcohol)
90. Alcohol [usp]
91. Ethanol [jan]
92. Ethicap
93. Hinetoless
94. Alcohols, C1-3
95. Cologne Spirits
96. Caswell No. 430
97. Reagent Alcohol
98. Infinity Pure
99. Aethylalkohol [german]
100. Desinfektol El
101. Anhydrous Alcohol
102. Anhydrous Ethanol
103. Ethyl Alcohol In Alcoholic Beverages
104. Fema No. 2419
105. Fema Number 2419
106. Alcool Etilico [italian]
107. Etylowy Alkohol [polish]
108. Ethyl Alcohol, Undenatured
109. Alcool Ethylique [french]
110. C2h5oh
111. Alkoholu Etylowego [polish]
112. Hsdb 82
113. Sdm No. 37
114. Ai3-01706
115. Ccris 945
116. Ethylicum
117. Alcohol,ethyl
118. Edible Alcohol
119. Ethanol Vapor
120. Sd Alcohol 23-hydrogen
121. Alcohol Denatured
122. Alcohol,dehydrated
123. Ru-tuss Hydrocodone Liquid
124. Alcohol, Denatured
125. Ethanol, Denatured
126. Ethanol, Anhydrous
127. Nsc 85228
128. Ethanol, Dehydrated
129. Alcohol (usp)
130. Epa Pesticide Chemical Code 001501
131. Absolute Ethyl Alcohol
132. Ethyl Alcohol, Absolute
133. Punctilious Ethyl Alcohol
134. Ethyl Alcohol, Dehydrated
135. Ethanol Absolute
136. Ethanol, Anhydrous, Denatured
137. Alcohol Determination--alcohol
138. Chebi:16236
139. Nsc-85228
140. 3k9958v90m
141. Ethanol, Cda 19
142. Ethanol, 200 Proof
143. Ethyl Alcohol Denatured
144. Ethylol
145. Pm-6193-200
146. Ethanol Anhydrous
147. 68475-56-9
148. Eoh
149. Sekundasprit
150. Alcohol Etilico
151. Spiritus Vini
152. Mfcd00003568
153. Ethanol Denatured
154. 42845-45-4
155. Lux
156. Sy Fresh M
157. Esumiru Wk 88
158. Ethanol (9ci)
159. Ethanol, Silent Spirit
160. Alcohol Denat.
161. Anhydrol Pm 4085
162. Ethyl Alcohol, Anhydrous
163. Ethyl Alcohol (ethanol)
164. Higher Alcohol Distillate
165. Alcohol 5% In Dextrose 5%
166. Einecs 200-578-6
167. Cologne Spirits (alcohol)
168. Sda 3a
169. Alcoholum
170. Ethanolum
171. Silent Spirit
172. Diluted Alcohol
173. Ethanol In Alcoholic Beverages
174. Vodka
175. Alcohol,sda
176. Ethanol-
177. 100c.npa
178. Cda 19
179. Ims 99
180. Sd Alcohol
181. Ethanol, Dimer
182. Alcohol,denatured
183. Unii-3k9958v90m
184. Alcohol (ethyl)
185. Undenatured Ethanol
186. Ahd 2000
187. Sda 40-2
188. Vanilla Powder
189. Einecs 270-649-4
190. Eosin Y, Alcoholic
191. Ablysinol
192. Alcohol 95%
193. Alcohol 190 Proof
194. Cda 19-200
195. Ethyl Alcohol 40%
196. Ethyl Alcohol 70%
197. Ethyl Alcohol 75%
198. Ethyl Alcohol 80%
199. Ethyl Alcohol 90%
200. Alcohol [vandf]
201. Alcohol [hsdb]
202. Alcohol [inci]
203. Ethanol, 99.8%
204. Ethanol, Technical Grade
205. Fatty Alcohol C8-10
206. Reagent Alcohol, 70%
207. Reagent Alcohol, 80%
208. Reagent Alcohol, 95%
209. Alcohol [ii]
210. Ch3ch2oh
211. Dehydrated Ethanol (tn)
212. Ethyl Alcohol 47.5%
213. Ethylicum [hpus]
214. Dsstox_cid_584
215. Ethanol, Standard For Gc
216. Alcohol [usp-rs]
217. Alcohol [who-ip]
218. Ethanol [who-dd]
219. Ethanol [who-ip]
220. Industrial Alcohol (ims)
221. Bmse000297
222. Chembl545
223. Ec 200-578-6
224. Ethanol, >=99.5%
225. Aerosol™ Ot Solution
226. Anhydrous Ethanol (jp17)
227. Ethyl Alcohol [mi]
228. Reagent Alcohol, For Hplc
229. Ethanol, Analytical Standard
230. Dsstox_rid_75674
231. Sd 3a
232. Dsstox_gsid_20584
233. Ru-tuss Liquid (salt/mix)
234. Ethanol, Usp, 99.5%
235. Ethyl Alcohol [fhfi]
236. Wln: Q2
237. Ethanol, For Residue Analysis
238. Reagent Alcohol, Acs Reagent
239. Alcohol [orange Book]
240. Alcohol,ethyl [vandf]
241. B3324 [langual]
242. Duplicating Fluid 100c.npa
243. Ethanol, P.a., 99.8%
244. Reagent Alcohol, Reagent Grade
245. Sdm No. 37 (salt/mix)
246. Gtpl2299
247. Anhydrous Ethanol [jan]
248. Avagard Component Alcohol
249. Hbn-1 Component Ethanol
250. Alcohol Dehydrated, >=85.0%
251. Dtxsid9020584
252. Ethanol, Technical Grade, 93%
253. Ethanol, Technical Grade, 99%
254. Unii-7528n5h79b
255. Chebi:17246
256. Ethanol, 95.1-96.9%
257. Poly(vinyl Alcohol) Macromolecule
258. Ru-tuss Expectorant (salt/mix)
259. Alcohol, Dehydrated [ii]
260. Alcoholum [who-ip Latin]
261. Ethanolum [who-ip Latin]
262. Ethyl Alcohol (6ci,7ci,8ci)
263. Alcohol,dehydrated [vandf]
264. Ethanol Component Of Hbn-1
265. Ethanol, Technical Grade, 93.8%
266. Ethanol, Technical Grade, 99.5%
267. Alcohol Component Of Avagard
268. Alcohol, Dehydrated [vandf]
269. Dehydrated Alcohol [usp-rs]
270. Ethanol, >=99.5%, For Hplc
271. Nsc85228
272. Str05604
273. Ethanol 100 Microg/ml In Methanol
274. Ethyl Alcohol 95% Acs/usp Grade
275. Tox21_202510
276. Stl264245
277. Ethanol 1000 Microg/ml In Methanol
278. Ethanol 2000 Microg/ml In Methanol
279. Ethanol, 95.0%, (190 Proof)
280. Ethanol, P.a., Acs Reagent, 96%
281. Ethanol, Tested According To Ph.eur.
282. Ethanol, Usp, 70.0-72.0%
283. Ethanol, Usp, 94.9-96.0%
284. Akos009104571
285. Ethanol, Reagent (denatured Sda 3a)
286. 7528n5h79b
287. Db00898
288. Ethanol 10000 Microg/ml In Methanol
289. Ethanol, Absolute, >=99.8% (gc)
290. Ethanol, Uv Hplc Spectroscopic, 95%
291. Un 1170
292. Cas-64-17-5
293. Ethanol, Denatured, (uk Ida Standard)
294. Ethanol, Saj First Grade, >=99.5%
295. Ethyl Alcohol Absolute, Acs/usp Grade
296. Ethanol, Jis Special Grade, >=99.5%
297. Ethanol, P.a., Acs Reagent, 95.0%
298. Ethanol, Technical Grade, 92.6-93.8
299. Ncgc00091458-01
300. Ncgc00091458-02
301. Ncgc00260059-01
302. Reagent Alcohol, Spectrophotometric Grade
303. Dehydrated Alcohol [usp Monograph]
304. Ethanol, Anhydrous [ep Monograph]
305. Q153
306. Ethanol, Absolute, For Hplc, >=99.8%
307. Ethanol, Anhydrous, Denatured, Hplc Grade
308. Ethyl Alcohol 95% (synthetic) Fcc Grade
309. Ethanol, Acs Reagent, 99.8, 200 Proof
310. Ethanol, Jis First Grade, 94.8-95.8%
311. Ethyl Alcohol Absolute (organic) Usp Grade
312. E1510
313. Ethanol In Alcoholic Beverages [iarc]
314. Ethanol Solution, Ep, Bp, 69.5-70.4%
315. Ethanol, Denatured, Spectrophotometric Grade
316. Ethanol, Jis Special Grade, 94.8-95.8%
317. Ft-0625729
318. Ft-0625731
319. Ft-0625732
320. Ft-0668048
321. Ethanol, >=99.5%, Saj Super Special Grade
322. Reagent Alcohol, Anhydrous, <=0.003% Water
323. Reagent Alcohol, Anhydrous, <=0.005% Water
324. C00469
325. D00068
326. Ethanol, >=99.5%, Suitable For Fluorescence
327. Ethanol, Alcohol Reagent, Anhydrous, Denatured
328. Ethyl Alcohol 95% (grain Derived) Fcc Grade
329. Ethyl Alcohol 95% (synthetic) Acs/usp Grade
330. Ethyl Alcohol Absolute (synthetic) Acs/usp Grade
331. Sr-01000944357
332. Ethanol, Puriss. P.a., Absolute, >=99.8% (gc)
333. Sr-01000944357-1
334. Ethanol, Denatured (5 % Ipa, 5 % N-propylacetate)
335. Reagent Alcohol, Used For Histology Tissue Preparation
336. Ethanol, Anhydrous, Denatured, Spectrophotometric Grade
337. Ethyl Alcohol, Pure, 190 Proof, For Molecular Biology
338. Ethyl Alcohol, Pure, 200 Proof, Anhydrous, >=99.5%
339. Ethyl Alcohol, Pure, 200 Proof, For Molecular Biology
340. Ethanol 70%, Denatured With 1% Mek, 1% Ipa, 10 Mg/l
341. Ethanol, Absolute, >=99.8% (gc), Sales Not In Germany
342. Ethyl Alcohol Absolute (dehydrated) Usp, Bp/ep, Jp Grade
343. Ethyl Alcohol, Pure, 200 Proof, Acs Reagent, >=99.5%
344. Reagent Alcohol, 70%, Used For Histology Tissue Preparation
345. Reagent Alcohol, 80%, Used For Histology Tissue Preparation
346. 1e37b0d2-6209-4b03-a57d-500f3223c2da
347. Alcohol, United States Pharmacopeia (usp) Reference Standard
348. Ethanol, >=99.5%, Suitable For Absorption Spectrum Analysis
349. Ethanol-water Solutions, Nist(r) Srm(r) 1828b, Six Levels
350. Ethyl Alcohol, Pure, 200 Proof, Hplc/spectrophotometric Grade
351. Reagent Alcohol, 95%, Used For Histology Tissue Preparation
352. Ethanol Solution, Nist(r) Srm(r) 2897a, Nominal Mass Fraction 2%
353. Ethanol Solution, Nist(r) Srm(r) 2898a, Nominal Mass Fraction 6%
354. Ethanol Solution, Nist(r) Srm(r) 2899a, Nominal 25% By Mass
355. Ethanol, P.a., Acs Reagent, Reag. Iso, Reag. Ph. Eur., 99.9%
356. Ethanol, Suitable For 300 Per Jis, >=99.5%, For Residue Analysis
357. Ethyl Alcohol, Pure, 190 Proof, Meets Usp Testing Specifications
358. Ethyl Alcohol, Pure, 200 Proof, Anhydrous, Zero2(tm), >=99.5%
359. Ethyl Alcohol, Pure, 200 Proof, Meets Usp Testing Specifications
360. Specially Denatured Alcohol, 190 Proof, Sda 23a, Contains Acetone
361. Specially Denatured Alcohol, 190 Proof, Sda 2b-3, Contains Toluene
362. Specially Denatured Alcohol, 190 Proof, Sda 30, Contains Methanol
363. Specially Denatured Alcohol, 190 Proof, Sda 3a, Contains Methanol
364. Specially Denatured Alcohol, 200 Proof, Sda 23a, Contains Acetone
365. Specially Denatured Alcohol, 200 Proof, Sda 2b-3, Contains Toluene
366. Specially Denatured Alcohol, 200 Proof, Sda 30, Contains Methanol
367. Specially Denatured Alcohol, 200 Proof, Sda 3a, Contains Methanol
368. Alcohol, Pharmaceutical Secondary Standard; Certified Reference Material
369. Dehydrated Alcohol, United States Pharmacopeia (usp) Reference Standard
370. Ethanol Fixative 80% V/v, Suitable For Fixing Solution (blood Films)
371. Ethanol Solution, Certified Reference Material, 2000 Mug/ml In Methanol
372. Ethanol Standards 10% (v/v), 10 % (v/v) In H2o, Analytical Standard
373. Ethanol, Absolute, For Gradient Elution, Sales Not In Germany, >=99.9%
374. Ethanol, Absolute, For Hplc, Sales Not In Germany1, >=99.8% (gc)
375. Ethanol, Absolute, Semiconductor Grade Puranal(tm) (honeywell 17826)
376. Ethanol, Suitable For 1000 Per Jis, >=99.5%, For Residue Analysis
377. Ethanol-water Solution, Nist(r) Srm(r) 2894, Nominal Mass Fraction 0.1%
378. Ethanol-water Solution, Nist(r) Srm(r) 2895, Nominal Mass Fraction 0.2%
379. Ethanol-water Solution, Nist(r) Srm(r) 2896, Nominal Mass Fraction 0.3%
380. Ethanol-water Solution, Nist(r) Srm(r) 2900, Nominal 95.6% By Mass
381. Ethyl Alcohol Absolute (dehydrated, Synthetic) Usp, Bp/ep, Jp Grade
382. Ethyl Alcohol, Pure, 140 Proof, Excise Tax-free, Permit For Use Required
383. Ethyl Alcohol, Pure, 160 Proof, Excise Tax-free, Permit For Use Required
384. Ethyl Alcohol, Pure, 190 Proof, Acs Spectrophotometric Grade, 95.0%
385. Specially Denatured Alcohol, 190 Proof, Sda 2b-4, Contains Heptanes
386. Specially Denatured Alcohol, 190 Proof, Sda 2b-4, Contains N-heptane
387. Specially Denatured Alcohol, 190 Proof, Sda 2b-5, Contains N-hexane
388. Specially Denatured Alcohol, 190 Proof, Sda 35a, Contains Ethyl Acetate
389. Specially Denatured Alcohol, 190 Proof, Sda 3c, Contains Isopropanol
390. Specially Denatured Alcohol, 200 Proof, Sda 2b-4, Contains Heptanes
391. Specially Denatured Alcohol, 200 Proof, Sda 2b-4, Contains N-heptane
392. Specially Denatured Alcohol, 200 Proof, Sda 2b-5, Contains N-hexane
393. Specially Denatured Alcohol, 200 Proof, Sda 35a, Contains Ethyl Acetate
394. Specially Denatured Alcohol, 200 Proof, Sda 3c, Contains Isopropanol
395. Alcohol Determination-alcohol, United States Pharmacopeia (usp) Reference Standard
396. Dehydrated Alcohol, Pharmaceutical Secondary Standard; Certified Reference Material
397. Ethanol Calibration Kit, Ampule Of 10 X 1.2 Ml, Certified Reference Material
398. Ethanol, Absolute, Reag. Iso, Reag. Ph. Eur., >=99.8% (gc), Liquid (clear, Colorless)
399. Ethanol, Puriss. P.a., Acs Reagent, Absolute Alcohol, Without Additive, A15 O1, >=99.8%
400. Ethanol, Puriss. P.a., Acs Reagent, Prima Fine Spirit, Without Additive, F15 O1, ~96%
401. Ethanol, Puriss., Meets Analytical Specification Of Ph.??eur., Bp, 96% (v/v)
402. Ethanol, Puriss., Meets Analytical Specification Of Ph.??eur., Bp, 96.0-97.2%
403. Ethanol-10, 10 Mg/dl In H2o, Pack Of 10 X 1.2 Ml Ampules, Certified Reference Material
404. Ethanol-150, 150 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
405. Ethanol-25, 25 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
406. Ethanol-300, 300 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
407. Ethanol-40, 40 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
408. Ethanol-50, 50 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
409. Ethanol-500, 500 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
410. Ethanol-80, 80 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
411. Ethanol-80, 80 Mg/dl In H2o, Ampule Of 5 X 5 Ml, Certified Reference Material
412. Ethanol-water Solution, Nist(r) Srm(r) 2891, Nominal Mass Fraction 0.02%
413. Ethanol-water Solution, Nist(r) Srm(r) 2892, Nominal Mass Fraction 0.04%
414. Ethanol-water Solution, Nist(r) Srm(r) 2893, Nominal Mass Fraction 0.08%
415. Specially Denatured Alcohol, 190 Proof, Sda 39c, Contains Diethyl Phthalate
416. Specially Denatured Alcohol, 200 Proof, Sda 39c, Contains Diethyl Phthalate
417. Ethanol, Absolute, Denaturated With 0.5-1.5 Vol.% 2-butanone And Approx. 0.001% Bitrex (gc), >=98% (gc)
418. Ethanol, Absolute, Semiconductor Grade Puranal(tm) (honeywell 17833), Sales Not In Germany, >=99.8% (vol.)
419. Ethanol, Bioultra, For Molecular Biology, >=99.8%, (absolute Alcohol, Without Additive, A15 O1)
420. Ethanol, Puriss., Over Molecular Sieve (h2o <=0.01%), Absolute Alcohol, Without Additive, A15 O1, >=99.8%
421. Ethanol, Purum, Absolute Ethanol, Denaturated With 1% Cyclohexane, A15 Cyclo1, >=99.8% (based On Denaturant-free Substance)
422. Ethanol, Purum, Absolute Ethanol, Denaturated With 2% 2-butanone, A15 Mek1, >=99.8% (based On Denaturant-free Substance)
423. Ethanol, Purum, Absolute Ethanol, Denaturated With 4.8% Isopropanol, A15 Ipa1, >=99.8% (based On Denaturant-free Substance)
424. Ethanol, Purum, Fine Spirit, Denaturated With 2% 2-butanone, F25 Mek1, ~96% (based On Denaturant-free Substance)
425. Ethanol, Purum, Fine Spirit, Denaturated With 4.8% Methanol, F25 Methyl1, ~96% (based On Denaturant-free Substance)
426. Ethanol, Purum, Secunda Spirit, Denaturated With 2% 2-butanone And 0.5% 4-methyl-2-pentanone, S15, ~96% (based On Denaturant-free Substance)
427. Ethanol-100 (10 Ampules/kit), 100 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
428. Ethanol-100 (5 Ampules/kit), 100 Mg/dl In H2o, Ampule Of 5 X 5 Ml, Certified Reference Material
429. Ethanol-20 (10 Ampules/kit), 20 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
430. Ethanol-20 (5 Ampules/kit), 20 Mg/dl In H2o, Ampule Of 5 X 5 Ml, Certified Reference Material
431. Ethanol-200 (10 Ampules/kit), 200 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
432. Ethanol-200 (5 Ampules/kit), 200 Mg/dl In H2o, Ampule Of 5 X 5 Ml, Certified Reference Material
433. Ethanol-400 (10 Ampules/kit), 400 Mg/dl In H2o, Ampule Of 10 X 1.2 Ml, Certified Reference Material
434. Ethanol-400 (5 Ampules/kit), 400 Mg/dl In H2o, Ampule Of 5 X 5 Ml, Certified Reference Material
435. Ethyl Alcohol, Pure, 140 Proof, Meets Water Usp Testing Specifications, Excise Tax-free, Permit For Use Required
436. Ethyl Alcohol, Pure, 190 Proof, Acs Reagent, Meets Usp Testing Specifications, Excise Tax-free, Permit For Use Required
437. Ethyl Alcohol, Pure, 200 Proof, Acs Reagent, Meets Usp Testing Specifications, Excise Tax-free, Permit For Use Required
438. Specially Denatured Alcohol, 190 Proof, Sda 40 (40-2), Contains 0.14 % (v/v) Tert-butyl Alcohol And Brucine Sulfate
439. Specially Denatured Alcohol, 190 Proof, Sda 40b, Contains Tert-butyl Alcohol And Denatonium Benzoate
440. Specially Denatured Alcohol, 200 Proof, Sda 40 (40-2), Contains 0.14 % (v/v) Tert-butyl Alcohol And Brucine Sulfate
441. Specially Denatured Alcohol, 200 Proof, Sda 40b, Contains Tert-butyl Alcohol And Denatonium Benzoate
| Molecular Weight | 46.07 g/mol |
|---|---|
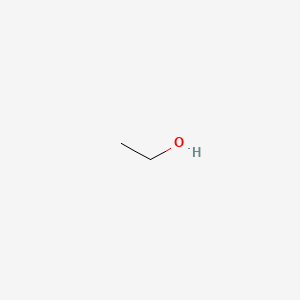
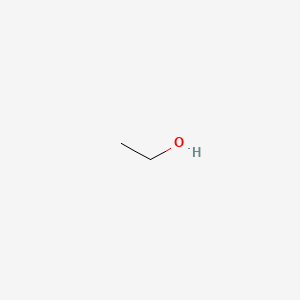
| Molecular Formula | C2H6O |
| XLogP3 | -0.1 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 1 |
| Rotatable Bond Count | 0 |
| Exact Mass | 46.041864811 g/mol |
| Monoisotopic Mass | 46.041864811 g/mol |
| Topological Polar Surface Area | 20.2 Ų |
| Heavy Atom Count | 3 |
| Formal Charge | 0 |
| Complexity | 2.8 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
/EXPL THER/ Ethanol lock therapy (ELT) has emerged as an effective method for the prevention and treatment of central line-associated bloodstream infections (CLABSIs), but the safety of ELT in infants has not been established. The objective of this study was to determine blood alcohol concentration (BAC) and evidence of hepatic injury in infants after infusing a small one-time dose of ethanol, equivalent to the volume that would be flushed through the central venous catheter (CVC) after ELT is completed. This was a prospective pilot study in infants weighing
PMID:25632063 Chhim RF et al; Ann Pharmacother 49 (4): 431-6 (2015)
/The objective of the study was/ to evaluate the efficacy, safety, pain perception and health-related quality of life (QoL) of percutaneous ethanol injection treatment (PEIT) as an alternative to thyroid surgery in symptomatic thyroid cysts. Thirty consecutive patients (46 +/- 10 years; 82% women) with symptomatic benign thyroid cysts relapsed after drainage were included. In all cases, cytology prior to treatment, maximum cyst diameter and volume were determined. PEIT was conducted using the established procedure, and the volume of fluid removed and pain perceived by the patient were assessed. In each procedure, the volume of alcohol instilled was <2 mL. After follow-up, final cyst diameter and volume were determined and the persistence of symptoms and QoL were assessed by a questionnaire (SF-36). Mean symptom duration was 10 +/- 20 months. A single session of PEIT was required to complete the procedure in 45% of patients, two in 31% and three in 13%. Mean initial maximum cyst diameter was 3.5 +/- 1.0 cm and mean extracted liquid volume 61 +/- 36 mL. During PEIT, 39% of patients experienced virtually no pain, 43% mild pain and 17% moderate pain. No complications of PEIT were observed. After 12.1 +/- 1.4 months of follow-up, cysts were reduced more than 70% in volume in 86.3% of patients, more than 80% in 61.9% and more than 90% in 42%. On the health-related QoL SF-36 questionnaire, patient scores 6 months post-PEIT did not differ significantly from those of the healthy Spanish population. With respect to cosmetic complaints or local symptoms of compression, PEIT-treated patients presented an initial score of 22 +/- 8 and 13 +/- 5 after treatment (p < 0.05). In our experience, percutaneous ethanol injection has proved to be an effective, safe and well-tolerated first-line treatment of symptomatic thyroid cysts.
PMID:26610707 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4661972 Reverter JL et al; BMC Endocr Disord 15: 73 (2015)
Because of the increased risk of surgery, thyroid nodules causing compression signs and/or hyperthyroidism are concerning during pregnancy. Six patients with nontoxic cystic, four with nontoxic solid, and three with overt hyperthyroidism caused by toxic nodules were treated with percutaneous ethanol injection therapy (PEI). An average of 0.68 mL ethanol per 1 mL nodule volume was administered. Mean number of PEI treatments for patients was 2.9. Success was defined as the shrinkage of the nodule by more than 50% of the pretreatment volume (V0) and the normalization of TSH and FT4 levels. The average V0 was 15.3 mL. Short-term success was measured prior to labor, whereas long-term success was determined during the final follow-up (an average of 6.8 years). The pressure symptoms decreased in all but one patient after PEI and did not worsen until delivery. The PEI was successful in 11 (85%) and 7 (54%) patients at short-term and long-term follow-up, respectively. Three patients underwent repeat PEI which was successful in 2 patients. PEI is a safe tool and seems to have good short-term results in treating selected symptomatic pregnant patients. Long-term success may require repeat PEI.
PMID:26697066 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677206 Solymosi T et al; Int J Endocrinol 2015: 765950 (2015)
Methanol poisoning outbreaks are a global public health issue, with delayed treatment causing poor outcomes. Out-of-hospital ethanol administration may improve outcome, but the difficulty of conducting research in outbreaks has meant that its effects have never been assessed. We study the effect of out-of-hospital ethanol in patients treated during a methanol outbreak in the Czech Republic between 2012 and 2014. This was an observational case-series study of 100 hospitalized patients with confirmed methanol poisoning. Out-of-hospital ethanol as a "first aid antidote" was administered by paramedic or medical staff before the confirmation of diagnosis to 30 patients; 70 patients did not receive out-of-hospital ethanol from the staff (12 patients self-administered ethanol shortly before presentation). The state of consciousness at first contact with paramedic or medical staff, delay to admission, and serum methanol concentration were similar among groups. The median serum ethanol level on admission in the patients with out-of-hospital administration by paramedic or medical staff was 84.3 mg/dL (interquartile range 32.7 to 129.5 mg/dL). No patients with positive serum ethanol level on admission died compared with 21 with negative serum ethanol level (0% versus 36.2%). Patients receiving out-of-hospital ethanol survived without visual and central nervous system sequelae more often than those not receiving it (90.5% versus 19.0%). A positive association was present between out-of-hospital ethanol administration by paramedic or medical staff, serum ethanol concentration on admission, and both total survival and survival without sequelae of poisoning. We found a positive association between out-of-hospital ethanol administration and improved clinical outcome. During mass methanol outbreaks, conscious adults with suspected poisoning should be considered for administration of out-of-hospital ethanol to reduce morbidity and mortality.
PMID:26875060 Zakharov S et al; Ann Emerg Med 68 (1): 52-61 (2016)
For more Therapeutic Uses (Complete) data for Ethanol (24 total), please visit the HSDB record page.
Although there is a dose response relationship between alcohol consumption and liver damage, less than one-third of alcoholics develop alcoholic liver disease (ALD). This individual susceptibility to the development of alcoholic liver disease may be explained by genetic and environmental factors. Of the genetic factors, female sex is clearly a significant risk factor, human leukocyte antigen status is probably important but further studies are needed, abnormalities in alcohol metabolism have not been shown to be of primary pathogenic importance and the plethora of immunological disturbances reported appear to be mere epiphenomena. Of the environmental factors, no consistent evidence attests to the significance of hepatitis B viral infection in the susceptibility to developing alcoholic liver disease.
Johnson RD, Williams R; Alcohol 20 (2): 137-60 (1985)
Maternal Medication usually Compatible with Breast-Feeding: alcohol (ethanol): Reported Sign or Symptom in Infant or Effect on Lactation: With large amounts drowsiness, diaphoresis, deep sleep, weakness, decrease in linear growth, abnormal weight gain; maternal ingestion of 1 g/kg daily decreases milk ejection reflex. /from Table 6/
Report of the American Academy of Pediatrics Committee on Drugs in Pediatrics 93 (1): 140 (1994)
Two weeks after percutaneous ethanol injection therapy for hepatocellular carcinoma, performed by injecting 110 mL ethanol in a single session with general anesthesia, a 69-year-old woman with well-compensated liver cirrhosis developed an extensive thrombosis of the whole portal tree that caused severe uncorrectable ascites and progressive deterioration of her general condition, resulting in death 6 weeks after the procedure.
PMID:9922194 Lencioni R et al; Abdom Imaging 23 (6): 608-10 (1998)
Two patients developed hepatic infarction after undergoing percutaneous ethanol injection therapy (PEIT) for hepatocellular carcinoma (HCC). In both cases, liver function parameters deteriorated immediately after the ethanol injection, and enhanced computed tomography images showed a wedge-shaped avascular low-density area due to hepatic infarction. In one patient, PEIT was performed for a nodule treated with transcatheter arterial infusion (TAI) using a suspension of styrene maleic acid neocarzinostatin (SMANCS) 4 weeks before. In the other patient, TAI with SMANCS had been carried out 14 months previously for a different nodule in the same segment where the nodule treated with PEIT was located. When PEIT is used for patients with HCC who have previously undergone TAI, especially with SMANCS, PEIT may induce hepatic infarction.
PMID:9872612 Seki T et al; Eur J Gastroenterol Hepatol 10 (11): 915-8
Since 1990, percutaneous ethanol injection therapy (PEIT) has been clinically applied as a treatment for autonomous functioning nodules of the thyroid as well as for cystic lesions. Some additional indications are currently under consideration, e.g. inoperable advanced cancer of the thyroid. Since its inception, PEIT has generally been regarded as an effective, low-risk, inexpensive procedure which can be performed on an ambulatory basis. /The authors/ report the first case of severe ethyl toxic necrosis of the larynx combined with necrotic dermatitis in a patient treated with PEIT by a radiologist. The patient was admitted to hospital, where the necrosis and dermatitis were treated conservatively. A cyst which developed in the right false vocal fold was removed by microsurgery 10 months later. Voice was restored almost to normal but a significant reduction in nodular volume was not seen, probably due to the inexperience of the operator. PEIT for functional thyroid gland autonomy is an inexpensive method of treating hyperthyroidism with focal autonomy on an ambulatory basis if surgical intervention and radioiodine therapy are not feasible either for medical reasons or because of refusal by the patient. Severe complications must be taken into consideration and discussed with the patient. To avoid complications, substantial experience and a precise ultrasound-guided injection are required. In the case of complications the opinion of a specialist should be sought at an early stage.
PMID:15768823 Mauz PS et al; Acta Otolaryngol 124 (10): 1226-30 (2004)
... The fatal dose of ethanol is between 500 and 1000 mL of 100-proof liquor (50% ethanol), ingested in an hour or two. ...
PMID:4574410 McBay AJ; Clinical Chemistry 19 (4): 361-365 (1973)
For therapeutic neurolysis of nerves or ganglia for the relief of intractable chronic pain in such conditions as inoperable cancer and trigeminal neuralgia (tic douloureux), in patients for whom neurosurgical procedures are contraindicated.
Treatment of congenital venous malformations
Treatment of uncontrolled primary hypertension
Alcohol produces injury to cells by dehydration and precipitation of the cytoplasm or protoplasm. This accounts for its bacteriocidal and antifungal action. When alcohol is injected in close proximity to nerve tissues, it produces neuritis and nerve degeneration (neurolysis). Ninety to 98% of ethanol that enters the body is completely oxidized. Ethanol is also used as a cosolvent to dissolve many insoluble drugs and to serve as a mild sedative in some medicinal formulations. Ethanol also binds to GABA, glycine, NMDA receptors and modulates their effects. Ethanol is also metabolised by the hepatic enzyme alcohol dehydrogenase.
Anti-Infective Agents, Local
Substances used on humans and other animals that destroy harmful microorganisms or inhibit their activity. They are distinguished from DISINFECTANTS, which are used on inanimate objects. (See all compounds classified as Anti-Infective Agents, Local.)
Central Nervous System Depressants
A very loosely defined group of drugs that tend to reduce the activity of the central nervous system. The major groups included here are ethyl alcohol, anesthetics, hypnotics and sedatives, narcotics, and tranquilizing agents (antipsychotics and antianxiety agents). (See all compounds classified as Central Nervous System Depressants.)
Solvents
Liquids that dissolve other substances (solutes), generally solids, without any change in chemical composition, as, water containing sugar. (Grant and Hackh's Chemical Dictionary, 5th ed) (See all compounds classified as Solvents.)
D08AX08
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
D - Dermatologicals
D08 - Antiseptics and disinfectants
D08A - Antiseptics and disinfectants
D08AX - Other antiseptics and disinfectants
D08AX08 - Ethanol
V - Various
V03 - All other therapeutic products
V03A - All other therapeutic products
V03AB - Antidotes
V03AB16 - Ethanol
V - Various
V03 - All other therapeutic products
V03A - All other therapeutic products
V03AZ - Nerve depressants
V03AZ01 - Ethanol
Absorption
Rapidly absorbed.
After oral administration, ethanol is absorbed rapidly into the bloodstream from the stomach and small intestines and distributes into total body water (0.5-0.7 L/kg). Peak blood levels occur about 30 minutes after ingestion of ethanol when the stomach is empty. Because absorption occurs more rapidly from the small intestine than from the stomach, delays in gastric emptying (owing, e.g., to the presence of food) slow ethanol absorption. ... After oral consumption of alcohol, first-pass metabolism by gastric and liver alcohol dehydrogenase enzymes leads to lower blood alcohol levels than would be obtained if the same dose were administered intravenously.
Brunton, L. Chabner, B, Knollman, B. Goodman and Gillman's The Pharmaceutical Basis of Therapeutics, Twelth Edition, McGraw Hill Medical, New York, NY. 2011, p. 630
The distribution of alcohol between alveolar air and blood depends on its speed of diffusion, and its vapor pressure at the prevailing temp and concentration of alcohol in the lung capillaries. Empirical determinations have yielded rather different values for this distribution ratio, but a commonly accepted value is 1:2100.
International Encyclopedia of Pharmacology and Therapeutics. Vol 1 Section 20: 170 (1970)
Venous blood (orbital sinus) and brain ethanol levels were measured in long sleep and short sleep mice within the first 30 min following ethanol administration (2.5 to 6.0 g/kg). Ethanol was administered ip or intragastrically. For both lines of mice and for every dose, brain ethanol concentrations were significantly greater (as much as 100 mg/dL) than blood ethanol levels for the first 6 min, and peak blood and brain ethanol levels were reached 4 to 6 min after dosing. Approx 6 to 10 min (depending on dose and line of mouse) was required for blood and brain concn to reach equilibrium. At the time of loss of the righting response brain ethanol levels were significantly higher than blood ethanol levels. These results indicate that within the first 6 min after administration of ethanol, blood ethanol level is not suitable for the assessment of brain ethanol content.
PMID:2719816 Smolen TN, Smolen A; Alcohol 6 (1): 33-8 (1989)
The method of Pohorecky and Brick was modified for determination of ethanol concn in rebreathed air of rats. Female Sprague Dawley rats were injected with different doses (1 to 2 g/kg) of ethanol and both arterial blood and rebreathed air samples were collected at various time intervals (15 to 120 min) after administration. A good correlation (r= 0.96) was found between ethanol concn in arterial blood and in rebreathed air; the blood/breath conversion factor was 3241 + or - 55.
PMID:2719817 Hiltunen AJ et al; Alcohol 6 (1): 39-43 (1989)
For more Absorption, Distribution and Excretion (Complete) data for Ethanol (31 total), please visit the HSDB record page.
Hepatic. Metabolized by cytochrome P450 enzyme CYP2E1.
Ethanol metabolism in hepatocytes causes the generation of reactive oxygen species, endoplasmic reticulum stress and alterations in mitochondrial energy and REDOX metabolism. In ethanol-exposed liver disease, autophagy not only acts as a cleanser to remove damaged organelles and cytosolic components, but also selectively clears specific targets such as lipid droplets and damaged mitochondria. Moreover, ethanol appears to play a role in protecting hepatocytes from apoptosis at certain concentrations. This article describes the evidence, function and potential mechanism of autophagy in ethanol-exposed liver disease and the controversy surrounding the effects of ethanol on autophagy.
PMID:26186640 Wang LR et al; Expert Rev Gastroenterol Hepatol 9 (8): 1031-7 (2015)
There have been allegations in the courtroom that elevated serum lactic acid in trauma victims can yield a falsely elevated serum ethanol assay. Most hospitals utilize an indirect method of ethanol measurement where a serum sample is added to a mix of alcohol dehydrogenase and oxidized nicotinamide adenine dinucleotide (NAD+). This allows any ethanol in the patient's serum to be metabolized to acetaldehyde, and in the process results in the reduction of NAD+ to NADH. NADH is then measured using spectrophotometry. The courtroom allegation stems from the concept that oxidation of lactate to pyruvate by lactate dehydrogenase (LDH) results in the same molar-for-molar reduction of NAD+ to NADH, and could therefore theoretically cause patients with elevated lactate and LDH to have a falsely elevated ethanol concentration. Patients with elevated lactic acid and LDH concentrations who presented to a university hospital from 20 April 2015 to 13 December 2015 were identified to provide possible test specimens. If a sufficient amount of serum was available, the sample was used to re-run the lactate and LDH concentration simultaneously with an enzymatic ethanol assay. Any samples that had elevated lactic acid and LDH concentrations on this retesting, and also yielded a positive ethanol concentration, were sent for confirmatory gas chromatography testing of ethanol concentrations. A control group of 20 samples with normal lactate and LDH were included. A total of 37 samples were included in the final analysis. Only 4 patients had an elevated enzymatic ethanol concentration, and all 4 also had a measurable GC ethanol concentration. The lactate in this dataset ranged from 2.4 to 24.2 mmol/L, with a mean of 6.53 mmol/L (normal value 0.5-2.2). The LDH ranged from 242 to 8838 U/L with a mean of 1695 U/L (normal value 122-225 U/L). Twenty control samples were run on patients with normal lactate and LDH, none of which yielded a positive enzymatic ethanol result. This data does not support the contention that an elevated LDH and lactate can yield a false positive serum ethanol result as run by enzymatic ethanol assay in live patients presenting to the emergency department.
PMID:28812382 Nacca N et al; Clin Toxicol (Phila) 16: 1-4 (2017)
Ethanol is metabolized largely by sequential hepatic oxidation, first to acetaldehyde by alcohol dehydrogenase (ADE) and then to acetic acid by aldehyde dehydrogenase (ALDH). Each metabolic step requires NAD+; thus oxidation of 1 mol ethanol (46 g) to 1 mol acetic acid requires 2 mol NAD+ in the liver; indeed, NAD+ availability limits ethanol metabolism to about 8 gr or 10 mL (approximately 170 mmol) per hour in a 70-kg adult, or approximately 120 mg/kg per hour. Thus hepatic ethanol metabolism functionally saturates at relatively low blood levels compared with the high blood ethano levels (BELs) achieved, and ethanol metabolism is a zero-order process (constant amount per unit time). Small amounts of ethanol are excreted in urine, sweat, and breath, but metabolism to acetate accounts to 90-98% of ingested ethanol, mostly owing to hepatic metabolism by ADH and ADLH.
Brunton, L. Chabner, B, Knollman, B. Goodman and Gillman's The Pharmaceutical Basis of Therapeutics, Twelth Edition, McGraw Hill Medical, New York, NY. 2011, p. 630
Metabolism of ethanol, propanol, isopropanol, butanol, isobutanol, sec-butanol, and tert-butanol was studied after oral administration in rabbits. Blood pH was on the acid side with propanol, butanol, and isobutanol, and on the alkaline side with isopropanol and sec-butanol, but no change was observed with ethanol and tert-butanol. Butanol and isobutanol had the lowest rate of urinary excretion. Acetaldehyde and acetic acid were detected as the urinary metabolites of ethanol and propanol, whereas isobutyraldehyde and isovaleric acid were the metabolites of isobutanol.
Saito M; Nichidai Igaku Zasshi 34 (8-9): 569-85 (1975)
For more Metabolism/Metabolites (Complete) data for Ethanol (13 total), please visit the HSDB record page.
Ethanol has known human metabolites that include acetaldehyde.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
... The concentrations of ethanol and methanol in blood were determined indirectly by analysis of end-expired alveolar air. In the morning when blood-ethanol dropped below the Km of liver alcohol dehydrogenase (ADH) of about 100 mg/L (2.2 mM), the disappearance half-life of ethanol was 21, 22, 18 and 15 min. in 4 test subjects respectively. ...
PMID:3588516 Jones AW; Pharmacol Toxicol. 60 (3): 217-20 (1987)
Ethanol affects the brains neurons in several ways. It alters their membranes as well as their ion channels, enzymes, and receptors. Alcohol also binds directly to the receptors for acetylcholine, serotonin, GABA, and the NMDA receptors for glutamate. The sedative effects of ethanol are mediated through binding to GABA receptors and glycine receptors (alpha 1 and alpha 2 subunits). It also inhibits NMDA receptor functioning. In its role as an anti-infective, ethanol acts as an osmolyte or dehydrating agent that disrupts the osmotic balance across cell membranes.
... Ethanol is known to affect a large number of membrane proteins that participate in signaling pathways such as neurotransmitter receptors, enzymes, and ion channels, and there is extensive evidence that ethanol interacts with a variety of neurotransmitters. The major actions of ethanol involve enhancing the inhibitory effects of gamma-aminobutyric acid (GABA) at GABAa receptors and blockade of the N-methyl-D-aspartate (NMDA) subtype of glutamate, an excitatory amine acid (EAA) receptor. Animal studies indicate that the acute effects of ethanol result from competitive inhibition of glycine binding to NMDA receptor and disruption of glutamatergic neurotransmission by inhibiting the response of the NMDA receptor. Persistent glycine antagonism and attenuation of glutamatergic neurotransmission by chronic ethanol exposure results in tolerance to ethanol by enhancing EAA neurotransmission and NMDA receptor upregulation. The latter appears to involve selective increases in NMDA R2B subunit concentrations and other molecular changes in specific brain loci. The abrupt withdrawal of ethanol thus produces a hyperexcitable state that leads to the ethanol withdrawal syndrome and excitotoxic neuronal death. GABA-mediated inhibition, which normally acts to limit excitation, is eliminated during ethanol withdrawal syndrome and further intensifies this excitation. In addition, NMDA receptors function to inhibit the release of dopamine in the nucleus accumbens and mesolimbic structures, which modulate the reinforcing action of addictive xenobiotics such as ethanol. By inhibiting NMDA receptor activity, ethanol could increase dopamine release from the nucleus accumbens and ventral tegmental area and could thus create dependence. Chronic ethanol administration also results in tolerance, dependence, and an ethanol withdrawal syndrome, mediated, in part, by desensitization and or downregulation of GABAa receptors.
Goldfrank, L.R., Goldfrank's Toxicologic Emergencies 10th Ed. 2015., McGraw-Hill, New York, N.Y., p. 1085
The development of alcoholic ketoacidosis (AKA) requires that a combination of physical and physiologic events occur. The normal response to starvation and depletion of hepatic glycogen stores is for amino acids to be converted to pyruvate. Pyruvate can serve as a substrate for gluconeogenesis, be converted to acetyl-CoA, which can enter the Krebs cycle or can be utilized in various biosynthetic pathways (eg, fatty acid, ketone bodies, cholesterol, and acetylcholine) ... Ethanol metabolism generates NADH, resulting in an excess of reducing potential. This high redox state favors the conversion of pyruvate to lactate, diverting pyruvate from being a substrate for gluconeogenesis. To compensate for the lack of normal metabolic substrates, the body mobilizes fat from adipose tissue and increased fatty acid metabolism as an alternative source of energy. This response is mediated by a decrease in insulin and an increased secretion of glucagon, catecholamines, growth hormone, and cortisol. Fatty acid metabolism results in the formation of acetyl-CoA and it combines with the excess acetate that is generated from ethanol metabolism to form acetoacetate. Most of the acetoacetate is reduced to beta-hydroxybutyrate due to the excess reducing potential or high redox state of the cell. Volume depletion interferes with the renal elimination of acetoacetate and beta-hydroxybutyrate, and contributes to the acidosis. An elevated lactate concentration may result from shunting from pyruvate or from hypoperfusion or infection that may coexist with the underlying ketoacidosis.
Goldfrank, L.R., Goldfrank's Toxicologic Emergencies 10th Ed. 2015., McGraw-Hill, New York, N.Y., p. 1088
Adenosine may mediate many of the acute and chronic motor effects of ethanol on the brain. Ethanol, probably through its metabolite, acetate, prevents adenosine uptake, raising synaptic adenosine concentrations. Excessive stimulation of several adenosine receptors in the cerebellum may explain much of the motor impairment from low ethanol concentrations. In fact, animals made tolerant to ethanol develop cross-tolerance to adenosine agonists. In mice, adenosine receptor agonists increase ethanol-induced incoordination while adenosine antagonists decrease this intoxicating response.
Goldfrank, L.R. (ed). Goldfrank's Toxicologic Emergencies. 7th Edition McGraw-Hill New York, New York 2002., p. 162
Chronic ethanol (alcohol) administration has been associated with alterations in the binding and function of the gamma-aminobutyric acid (GABAA) receptor. To evaluate the mechanism underlying these changes, /the authors/ measured the steady state levels of the mRNAs for the alpha 1, alpha 2, alpha 3, alpha 5, and alpha 6 subunits of the GABAA receptor after chronic ethanol administration to rats and ethanol withdrawal for 24 hr. The results indicated that chronic ethanol administration resulted in a 61% decline in the level of the GABAA receptor alpha 1 subunit mRNAs [3.8 and 4.3 kilobases (kb)] in the cerebral cortex in rats. The levels of the alpha 2 subunit mRNAs (6 and 3 kb) and the alpha 5 subunit mRNA (2.8 kb) were also reduced, by 61, 45, and 51%, respectively, whereas there was no change in the level of the alpha 3 subunit mRNA (3 kb). Furthermore, the ethanol-induced decrease in receptor mRNA levels persisted for 24 hr, after withdrawal of ethanol and returned to control values at 36 hr of withdrawal. alpha 1 mRNA levels in cerebellum also decreased by 28%. The level of the alpha 6 subunit mRNA, which selectively encodes Ro15-4513 binding sites, was found to be increased by approximately 76% in the cerebellum. Also, the photoaffinity labeling studies using [3H]Ro15-4513 indicated an increase in the levels of various protein components of the GABAA receptor, in the cerebellum and the cerebral cortex (e.g., 50- and 55-kDa proteins in the cerebellum and 41- and 50-kDa proteins in the cortex), after chronic ethanol treatment. The increase in alpha 6 mRNA in the cerebellum might be related to the increased labeling of the 55-kDa (approximately 56-kDa) protein and partially responsible for the increased binding ... . Because the alpha 6 subunit is not expressed in cortex, involvement of an as yet unknown subunit in this region cannot be ruled out. The effect of chronic ethanol treatment appears to be specific for GABAA receptor subunit mRNAs, because the same treatment did not alter the levels of glyceraldehyde-3-dehydrogenase mRNA or poly(A)+ RNA. In summary, these data indicate that chronic ethanol treatment results in an alteration in the regulation of expression of GABAA receptor subunit-encoding mRNAs, which could be due to alterations in transcription or mRNA stability.
PMID:1383684 Mhatre MC et al; Mol Pharmacol 42 (3): 415-22 (1992)
For more Mechanism of Action (Complete) data for Ethanol (8 total), please visit the HSDB record page.