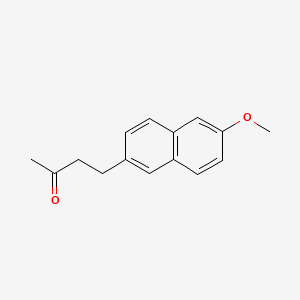
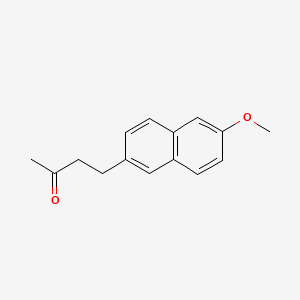
1. 4-(6-methoxy-2-naphthyl)-2-butanone
2. Apo-nabumetone
3. Aponabumetone
4. Arthraxan
5. Brl 14777
6. Gen-nabumetone
7. Listran
8. Mebutan
9. Nabucox
10. Nabumeton
11. Relafen
12. Relif
13. Relifex
14. Rhoxal Nabumetone
15. Rhoxal-nabumetone
1. 42924-53-8
2. Relafen
3. 4-(6-methoxynaphthalen-2-yl)butan-2-one
4. Arthaxan
5. Nabumetona
6. Relifex
7. 4-(6-methoxy-2-naphthyl)-2-butanone
8. Listran
9. Relifen
10. Consolan
11. Balmox
12. Nabumetonum [inn-latin]
13. Nabumetonum
14. Nabuser
15. 4-(6-methoxy-2-naphthalenyl)-2-butanone
16. Brl 14777
17. Brl-14777
18. 4-(2-methoxynaphthalen-6-yl)butan-2-one
19. Brl14777
20. 2-butanone, 4-(6-methoxy-2-naphthalenyl)-
21. Mls000069541
22. Nabumeton
23. Mebutan
24. Relif
25. Nsc-758623
26. Lw0tiw155z
27. Smr000058835
28. Chebi:7443
29. Dolsinal
30. Flambate
31. Unimetone
32. Prodac
33. Ncgc00016853-01
34. Cas-42924-53-8
35. Dsstox_cid_25472
36. Dsstox_rid_80901
37. Dsstox_gsid_45472
38. Sr-01000759138
39. Unii-lw0tiw155z
40. Brn 2103472
41. Ccris 8108
42. Nabumatone Form Ii
43. Relafen (tn)
44. Mfcd00079518
45. Nabumetone [usan:usp:inn:ban:jan]
46. Spectrum_001486
47. Nabumetone [mi]
48. Opera_id_765
49. Nabumetone [inn]
50. Nabumetone [jan]
51. Prestwick0_000909
52. Prestwick1_000909
53. Prestwick2_000909
54. Prestwick3_000909
55. Spectrum2_001969
56. Spectrum4_000174
57. Spectrum5_001286
58. Nabumetone [usan]
59. Nabumetone [vandf]
60. Cid_4409
61. Nabumetone [mart.]
62. Schembl2256
63. Chembl1070
64. Nabumetone [usp-rs]
65. Nabumetone [who-dd]
66. Bspbio_000758
67. Kbiogr_000687
68. Kbioss_001966
69. Mls001076325
70. Bidd:gt0104
71. Divk1c_000850
72. Spectrum1503650
73. Spbio_002097
74. Spbio_002957
75. Nabumetone, Analytical Standard
76. Bpbio1_000834
77. Gtpl7245
78. Nabumetone (jp17/usp/inn)
79. Dtxsid4045472
80. Nabumetone [orange Book]
81. Bdbm40128
82. Hms502k12
83. Kbio1_000850
84. Kbio2_001966
85. Kbio2_004534
86. Kbio2_007102
87. Zinc20221
88. Nabumetone [ep Monograph]
89. Nabumetone [usp Impurity]
90. Ninds_000850
91. Hms1570f20
92. Hms1922g10
93. Hms2090d13
94. Hms2093i05
95. Hms2097f20
96. Hms2230h12
97. Hms3259i16
98. Hms3652m04
99. Hms3714f20
100. Hms3885a22
101. Nabumetone [usp Monograph]
102. Pharmakon1600-01503650
103. Bcp12152
104. Hy-b0559
105. Tox21_110647
106. Ccg-39507
107. Nsc758623
108. S4051
109. Akos009529199
110. Tox21_110647_1
111. 4-(6-methoxy-2-naphthyl)butan-2-one
112. Db00461
113. Ks-1371
114. Nc00579
115. Nsc 758623
116. Idi1_000850
117. Ncgc00016853-02
118. Ncgc00016853-03
119. Ncgc00016853-06
120. Ncgc00016853-13
121. Ncgc00095063-01
122. Ncgc00095063-02
123. Ac-19025
124. Bn166181
125. Nabumetone 100 Microg/ml In Acetonitrile
126. Sbi-0051869.p002
127. Ab00052392
128. Am20040460
129. Ft-0629765
130. Ft-0672583
131. Sw197312-3
132. D00425
133. L10109
134. Ab00052392-13
135. Ab00052392_14
136. Ab00052392_15
137. 924n538
138. A826072
139. Q425207
140. Sr-01000759138-2
141. Sr-01000759138-3
142. Brd-k65146499-001-04-8
143. Brd-k65146499-001-14-7
144. Nabumetone, British Pharmacopoeia (bp) Reference Standard
145. Nabumetone, European Pharmacopoeia (ep) Reference Standard
146. Nabumetone, United States Pharmacopeia (usp) Reference Standard
| Molecular Weight | 228.29 g/mol |
|---|---|
| Molecular Formula | C15H16O2 |
| XLogP3 | 3.1 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 2 |
| Rotatable Bond Count | 4 |
| Exact Mass | 228.115029749 g/mol |
| Monoisotopic Mass | 228.115029749 g/mol |
| Topological Polar Surface Area | 26.3 Ų |
| Heavy Atom Count | 17 |
| Formal Charge | 0 |
| Complexity | 262 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 2 | |
|---|---|
| Drug Name | Nabumetone |
| PubMed Health | Nabumetone (By mouth) |
| Drug Classes | Analgesic, Antirheumatic, Central Nervous System Agent, Musculoskeletal Agent |
| Drug Label | Nabumetone is a naphthylalkanone designated chemically as 4-(6-methoxy-2-naphthalenyl)-2-butanone. It has the following structure:chemical structureC15H16O2 M.W. 228.3 Nabumetone is a white to off-white crystalline substance. It is nonacidic and... |
| Active Ingredient | Nabumetone |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 500mg; 750mg |
| Market Status | Prescription |
| Company | Mylan Pharms; Teva; Apotex; Lupin; Sandoz; Invagen Pharms; Par Pharm; Watson Labs |
| 2 of 2 | |
|---|---|
| Drug Name | Nabumetone |
| PubMed Health | Nabumetone (By mouth) |
| Drug Classes | Analgesic, Antirheumatic, Central Nervous System Agent, Musculoskeletal Agent |
| Drug Label | Nabumetone is a naphthylalkanone designated chemically as 4-(6-methoxy-2-naphthalenyl)-2-butanone. It has the following structure:chemical structureC15H16O2 M.W. 228.3 Nabumetone is a white to off-white crystalline substance. It is nonacidic and... |
| Active Ingredient | Nabumetone |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 500mg; 750mg |
| Market Status | Prescription |
| Company | Mylan Pharms; Teva; Apotex; Lupin; Sandoz; Invagen Pharms; Par Pharm; Watson Labs |
**Indicated** for: 1) Symptomatic relief in rheumatoid arthritis. 2) Symptomatic relief in osteoarthritis.
FDA Label
NSAIDs, like nabumetone, are well established as analgesics. NSAIDs reduce both peripheral and central sensitization of nociceptive neurons due to inflammation which contribute to hyperalgesia and allodynia. This sensitization occurs through reducing the action potential threshold in peripheral neurons, reducing the intensity of painful stimuli needed to produce a painful sensation. Centrally, activation of dorsal horn neurons occurs along with increased release of glutamate, calcitonin gene-related peptide (CGRP), and substance P which increase the transmission of painful stimuli. Coupled with this is an inhibition glycinergic neurons which normally inhibit pain transmission, a phenomenon known as disinhibition. Increased activity ofn-methyl d-aspartate (NMDA) and -amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors leads to the establishment of central sensitization, allowing both mild painful and innocuous stimuli to produce action potentials in nociceptive projection neurons. NSAIDs are effective in reducing mild-moderate acute and chronic nociceptive pain, however, the usefulness of NSAIDs in neuropathic pain is limited. The anti-inflammatory effect of NSAIDs is mediated by preventing vasodilation, increases in vascular permeability, and the release of cytokines from endothelial cells. These three effects together prevent immunocompetent cells from migrating to the site of injury thereby preventing additional damage and inflammation due to activation of the immune system at the site of damage. PGs also modulate T-helper cell activation and differentiation, an activity which is thought to be of importance in arthritic conditions. The anti-pyretic effect of NSAIDs is mediated through preventing increases in temperature by prostaglandins (PGs) via the hypothalamus. Activation of this process by other inflammatory mediators relies upon subsequent action by PGs, therefore NSAIDs are able to reduce fever due to these mediators as well. The adverse effects of NSAIDs are related to their therapeutic effects. The same vasodilatory action which occurs in inflammation also serves to regulate blood flow to the kidneys through the afferent renal arteries. NSAIDs are widely known as nephrotoxic agents as the reduction in PGs produces vasoconstriction of these arteries resulting in reduced blood flow to the kidneys and a subsequent decline in renal function. Reductions in mucus and HCO3- secretion in the stomach increases the risk of ulceration by limiting the protection mediated by PGs. Lastly, COX-2 selective agents like nabumetone can unbalance prothrombotic and antithrombotic prostanoid generation leading to increased platelet aggregation and increased risk of thrombosis.
Anti-Inflammatory Agents, Non-Steroidal
Anti-inflammatory agents that are non-steroidal in nature. In addition to anti-inflammatory actions, they have analgesic, antipyretic, and platelet-inhibitory actions. They act by blocking the synthesis of prostaglandins by inhibiting cyclooxygenase, which converts arachidonic acid to cyclic endoperoxides, precursors of prostaglandins. Inhibition of prostaglandin synthesis accounts for their analgesic, antipyretic, and platelet-inhibitory actions; other mechanisms may contribute to their anti-inflammatory effects. (See all compounds classified as Anti-Inflammatory Agents, Non-Steroidal.)
Cyclooxygenase 2 Inhibitors
A subclass of cyclooxygenase inhibitors with specificity for CYCLOOXYGENASE-2. (See all compounds classified as Cyclooxygenase 2 Inhibitors.)
M01AX01
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
M - Musculo-skeletal system
M01 - Antiinflammatory and antirheumatic products
M01A - Antiinflammatory and antirheumatic products, non-steroids
M01AX - Other antiinflammatory and antirheumatic agents, non-steroids
M01AX01 - Nabumetone
Absorption
Nabumetone is well-absorbed from the GI tract and undergoes significant first pass metabolism resulting in approximately 35% being converted to the active metabolite, 6-MNA. Tmax for 6-MNA varies widely with a mean values of 3 and 11 hours reported in official product monographs, and described as 9-12 hours in published literature Administration with food increases Cmax by 33% and increases absorption rate. If formulated as a suspension the Cmax increases and the Tmax is reduced by 0.8 hours while the all other pharmacokinetic parameters remain unchanged.
Route of Elimination
Most drug is eliminated via hepatic metabolism with minimal to no parent drug detectable in the plasma. 80% of the dose is then excreted by the kidneys and 10% in the feces. It does not appear to undergo enterohepatic recirculation.
Volume of Distribution
The Vd of 6-MNA reported after administration of a single dose is 0.1-0.2 L/kg or approximately 5-10 L. Vdss reported in official product labeling is approximately 53 L.
Clearance
6-MNA has an apparent steady-state clearance of 20 - 30 mL/min.
Nabumetone is reduced to 3-hydroxy nabumetone by the aldo-keto reductase-1C family and by corticosteroid 11-beta-dehydrogenase. It then undergoes oxidative cleavage by CYP1A2 to 6-MNA, the active metabolite. 6-MNA is eliminated by O-demethylation by CYP2C9 to 6-hydroxy-2-naphthylacetic acid (6-HNA). Both 6-MNA and 6-HNA are further converted to conjugates. Other metabolites are generated through a mix of ketone reduction and O-demethylation along with subsequent conjugation. Glucuronide conjugates of several metabolites have been found to become further conjugated to glycine residues.
Nabumetone has known human metabolites that include 4-hydroxy-4-(6-methoxynaphthalen-2-yl)butan-2-one.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
6-MNA has a mean half-life of 24 hours with a range of 19-36 hours.
Nabumetone's active metabolite, 6-MNA, is an inhibitor of both COX-1 and COX-2 although it exhibits some COX-2 selectivity. Inhibition of COX-1 and COX-2 reduces conversion of arachidonic acid to PGs and thromboxane (TXA2). This reduction in prostanoid production is the common mechanism that mediates the effects of nambutone. PGE2 is the primary PG involved in modulation of nociception. It mediates peripheral sensitization through a variety of effects. PGE2 activates the Gq-coupled EP1 receptor leading to increased activity of the inositol trisphosphate/phospholipase C pathway. Activation of this pathway releases intracellular stores of calcium which directly reduces action potential threshold and activates protein kinase C (PKC) which contributes to several indirect mechanisms. PGE2 also activates the EP4 receptor, coupled to Gs, which activates the adenylyl cyclase/protein kinase A (AC/PKA) signaling pathway. PKA and PKC both contribute to the potentiation of transient receptor potential cation channel subfamily V member 1 (TRPV1) potentiation, which increases sensitivity to heat stimuli. They also activate tetrodotoxin-resistant sodium channels and inhibit inward potassium currents. PKA further contributes to the activation of the P2X3 purine receptor and sensitization of T-type calcium channels. The activation and sensitization of depolarizing ion channels and inhibition of inward potassium currents serve to reduce the intensity of stimulus necessary to generate action potentials in nociceptive sensory afferents. PGE2 act via EP3 to increase sensitivity to bradykinin and via EP2 to further increase heat sensitivity. Central sensitization occurs in the dorsal horn of the spinal cord and is mediated by the EP2 receptor which couples to Gs. Pre-synaptically, this receptor increases the release of pro-nociceptive neurotransmitters glutamate, CGRP, and substance P. Post-synaptically it increases the activity of AMPA and NMDA receptors and produces inhibition of inhibitory glycinergic neurons. Together these lead to a reduced threshold of activating, allowing low intensity stimuli to generate pain signals. PGI2 is known to play a role via its Gs-coupled IP receptor although the magnitude of its contribution varies. It has been proposed to be of greater importance in painful inflammatory conditions such as arthritis. By limiting sensitization, both peripheral and central, via these pathways NSAIDs can effectively reduce inflammatory pain. PGI2 and PGE2 contribute to acute inflammation via their IP and EP2 receptors. Similarly to adrenergic receptors these are Gs-coupled and mediate vasodilation through the AC/PKA pathway. PGE2 also contributes by increasing leukocyte adhesion to the endothelium and attracts the cells to the site of injury. PGD2 plays a role in the activation of endothelial cell release of cytokines through its DP1 receptor. PGI2 and PGE2 modulate T-helper cell activation and differentiation through IP, EP2, and EP4 receptors which is believed to be an important activity in the pathology of arthritic conditions. By limiting the production of these PGs at the site of injury, NSAIDs can reduce inflammation. PGE2 can cross the blood-brain barrier and act on excitatory Gq EP3 receptors on thermoregulatory neurons in the hypothalamus. This activation triggers an increase in heat-generation and a reduction in heat-loss to produce a fever. NSAIDs prevent the generation of PGE2 thereby reducing the activity of these neurons. The adverse effects of NSAIDs stem from the protective and regulatory roles of prostanoids which have been well-characterized. PGI2 and PGE2 regulate blood flow to the kidney by similar mechanisms to the vasodilation they produce in inflammation. Prevention of this regulation by NSAIDs produces vasoconstriction which limits renal function by reducing blood flow and the hydrostatic pressure which drives filtration. PGE2 also regulates gastric protection via EP3 receptors which are, in this location, coupled to Gi which inhibits the AC/PKA pathway. This reduces the secretion of protons by H+/K+ ATPase in parietal cells and increases the secretion of mucus and HCO3- by superficial endothelial cells. Disruption of this protective action by NSAIDs lead to ulceration of the gastric mucosa. Lastly, disruption of PGI2, which opposes platelet aggregation, generation by COX-2 selective agents leads to an imbalance with TXA2 generated by COX-1, which promotes aggregation of platelets, leading to increased risk of thrombosis. Since nabumetone is somewhat COX-2 selective it is thought to promote this imbalance and increase thrombotic risk.