1. Antibiotic 10676
2. Framycetin
3. Framycetin Sulfate
4. Neomycin B
5. Neomycin B Sulfate
6. Soframycin
7. Sulfate, Framycetin
8. Sulfate, Neomycin B
1. Framycetin
2. Neomycin B
3. Fradiomycin
4. Mycifradin
5. Soframycin
6. Fradiomycin B
7. Actiline
8. Enterfram
9. Framygen
10. Actilin
11. Neomas
12. Fradiomycinum
13. Framicetina
14. Framycetine
15. Framycetinum
16. 119-04-0
17. Caswell No. 595
18. Nivemycin
19. Neomycin B Sulfate
20. 1404-04-2
21. Antibiotic 10676
22. Neomycin Sulfate
23. Neomycin Solution
24. Neobrettin
25. Usaf Cb-19
26. Ccris 5462
27. Framidal
28. Framycin
29. Francetin
30. Dekamycin Iii
31. Hsdb 3242
32. Soframycine
33. Framycetin (inn)
34. Neo-rx
35. Antibiotique
36. Myacyne
37. Neolate
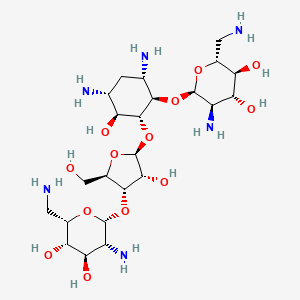
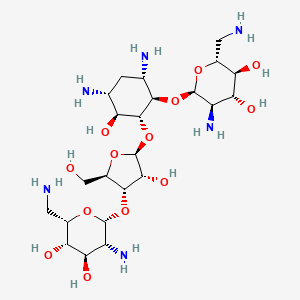
38. (2r,3s,4r,5r,6r)-5-amino-2-(aminomethyl)-6-[(1r,2r,3s,4r,6s)-4,6-diamino-2-[(2s,3r,4s,5r)-4-[(2r,3r,4r,5s,6s)-3-amino-6-(aminomethyl)-4,5-dihydroxyoxan-2-yl]oxy-3-hydroxy-5-(hydroxymethyl)oxolan-2-yl]oxy-3-hydroxycyclohexyl]oxyoxane-3,4-diol
39. Antibiotique Ef 185
40. Neomycin Sulphate
41. Chebi:7508
42. Vonamycin Powder V
43. (1r,2r,3s,4r,6s)-4,6-diamino-2-{[3-o-(2,6-diamino-2,6-dideoxy-beta-l-idopyranosyl)-beta-d-ribofuranosyl]oxy}-3-hydroxycyclohexyl 2,6-diamino-2,6-dideoxy-alpha-d-glucopyranoside
44. Neomcin
45. Neomin
46. 4boc774388
47. Neomicina [dcit]
48. Framycetinum [inn-latin]
49. Neomicina
50. Neomycine
51. Neomycinum
52. Pimavecort
53. Framycetin [inn]
54. Neomycine [inn-french]
55. Neomycinum [inn-latin]
56. Framycetine [inn-french]
57. Nmy
58. Framicetina [inn-spanish]
59. Framycetin [inn:ban:dcf]
60. Bycomycin
61. Jernadex
62. Neomycin [inn:ban]
63. Einecs 204-292-2
64. Einecs 215-766-3
65. Epa Pesticide Chemical Code 006303
66. Brn 0101621
67. Mycerin
68. Unii-i16qd7x297
69. Unii-4boc774388
70. Antibiotic 956
71. (2r,3s,4r,5r,6r)-5-amino-2-(aminomethyl)-6-[(1r,2r,3s,4r,6s)-4,6-diamino-2-[(2s,3r,4s,5r)-4-[(2r,3r,4r,5s,6s)-3-amino-6-(aminomethyl)-4,5-dihydroxy-tetrahydropyran-2-yl]oxy-3-hydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl]oxy-3-hydroxy-cyclohexoxy]tetrahydropyran-3,4-diol
72. Neomycinb
73. Antibiotic Produced By Streptomyces Decaris. Neomycin B
74. Neomycin B [mi]
75. Prestwick3_000158
76. Kdr Kinase Inhibitor, 3
77. Bdbm19
78. Neomycin B; Fradiomycin B
79. Schembl3279
80. Framycetin [who-dd]
81. Bspbio_000296
82. Gtpl709
83. Neomycin B [usp-rs]
84. 4-18-00-07476 (beilstein Handbook Reference)
85. D-streptamine, O-2,6-diamino-2,6-dideoxy-alpha-d-glucopyranosyl-(1-4)-o-(o-2,6-diamino-2,6-dideoxy-beta-l-idopyranosyl-(1-3)-beta-d-ribofuranosyl-(1-5))-2-deoxy-
86. Bpbio1_000326
87. Chembl184618
88. Dtxsid2023359
89. Hms2089p15
90. I16qd7x297
91. Zinc71928291
92. Akos024284361
93. Cs-6390
94. Db00452
95. Ncgc00179612-01
96. D-streptamine, O-2,6-diamino-2,6-dideoxy-.beta.-l-idopyranosyl-(1.->3)-o-.beta.-d-ribofuranosyl-(1->5)]-o-[2,6-diamino-2,6-dideoxy-.alpha.-d-glucopyranosyl-(1->4)]-2-deoxy
97. Hy-17624
98. Ab00443887
99. C01737
100. D05140
101. Ab00443887-03
102. Mycifradin; Neomas; Pimavecort; Vonamycin
103. Antibiotic Produced By Streptomyces Decaris
104. J-004060
105. Q4492348
106. Brd-k71013094-065-01-2
107. (2r,3s,4r,5r,6r)-5-amino-2-(aminomethyl)-6-{[(1r,2r,3s,4r,6s)-4,6-diamino-2-{[(2s,3r,4s,5r)-4-{[(2r,3r,4r,5s,6s)-3-amino-6-(aminomethyl)-4,5-dihydroxyoxan-2-yl]oxy}-3-hydroxy-5-(hydroxymethyl)oxolan-2-yl]oxy}-3-hydroxycyclohexyl]oxy}oxane-3,4-diol
108. (2s,3s,4r,5r,6r)-5-amino-2-(aminomethyl)-6-{[(2r,3s,4r,5s)-5-{[(1r,2r,3s,5r,6s)-3,5-diamino-2-{[(2r,3r,4r,5s,6r)-3-amino-6-(aminomethyl)-4,5-dihydroxyoxan-2-yl]oxy}-6-hydroxycyclohexyl]oxy}-4-hydroxy-2-(hydroxymethyl)oxolan-3-yl]oxy}oxane-3,4-diol
109. 11004-65-2
110. 6-(2-{(4s,2r,3r,5r)-4-[(5s,6s,2r,3r,4r)-3-amino-6-(aminomethyl)-4,5-dihydroxy( 2h-3,4,5,6-tetrahydropyran-2-yloxy)]-3-hydroxy-5-(hydroxymethyl)oxolan-2-yloxy }(3s,6s,1r,2r,4r)-4,6-diamino-3-hydroxycyclohexyloxy)(3s,2r,4r,5r,6r)-5-amino- 2-(aminomethyl)-2h
111. D-streptamine, O-2,6-diamino-2,6-dideoxy-.alpha.-d-glucopyranosyl-(1->4)-o-(o-2,6-diamino-2,6-dideoxy-.beta.-l-idopyranosyl-(1->3)-.beta.-d-ribofuranosyl-(1->5))-2-deoxy-
112. D-streptamine, O-2,6-diamino-2,6-dideoxy-.beta.-l-idopyranosyl-(1->3)-o-.beta.-d-ribofuranosyl-(1->5)-o-(2,6-diamino-2,6-dideoxy-.alpha.-d-glucopyranosyl-(1->4))-2-deoxy-
113. Wurcs=2.0/3,3,2/[a222h-1b_1-4][a2122h-1a_1-5_2*n_6*n][a2121h-1b_1-5_2*n_6*n]/1-2-3/a1n2-b1n1*1oc^rc^ro*2/4c^sc^rcc^s$3/10n/8n/7o_a3-c1
| Molecular Weight | 614.6 g/mol |
|---|---|
| Molecular Formula | C23H46N6O13 |
| XLogP3 | -9 |
| Hydrogen Bond Donor Count | 13 |
| Hydrogen Bond Acceptor Count | 19 |
| Rotatable Bond Count | 9 |
| Exact Mass | 614.31228554 g/mol |
| Monoisotopic Mass | 614.31228554 g/mol |
| Topological Polar Surface Area | 353 Ų |
| Heavy Atom Count | 42 |
| Formal Charge | 0 |
| Complexity | 872 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 19 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 4 | |
|---|---|
| Drug Name | Neo-fradin |
| PubMed Health | Neomycin (By mouth) |
| Drug Classes | Antibiotic |
| Active Ingredient | Neomycin sulfate |
| Dosage Form | Solution |
| Route | Oral |
| Strength | eq 87.5mg base/5ml |
| Market Status | Prescription |
| Company | X Gen Pharms |
| 2 of 4 | |
|---|---|
| Drug Name | Neomycin sulfate |
| Active Ingredient | Neomycin sulfate |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 500mg |
| Market Status | Prescription |
| Company | Oman Pharm Products; Teva; X Gen Pharms |
| 3 of 4 | |
|---|---|
| Drug Name | Neo-fradin |
| PubMed Health | Neomycin (By mouth) |
| Drug Classes | Antibiotic |
| Active Ingredient | Neomycin sulfate |
| Dosage Form | Solution |
| Route | Oral |
| Strength | eq 87.5mg base/5ml |
| Market Status | Prescription |
| Company | X Gen Pharms |
| 4 of 4 | |
|---|---|
| Drug Name | Neomycin sulfate |
| Active Ingredient | Neomycin sulfate |
| Dosage Form | Tablet |
| Route | Oral |
| Strength | 500mg |
| Market Status | Prescription |
| Company | Oman Pharm Products; Teva; X Gen Pharms |
Anti-Bacterial Agents; Protein Synthesis Inhibitors
National Library of Medicine's Medical Subject Headings. Neomycin. Online file (MeSH, 2016). Available from, as of December 5, 2016: https://www.nlm.nih.gov/mesh/2016/mesh_browser/MBrowser.html
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Neomycin is included in the database.
NIH/NLM; ClinicalTrials.Gov. Available from, as of February 1, 2017: https://clinicaltrials.gov/ct2/results?term=NEOMYCIN&Search=Search
Neomycin sulfate tablets are indicated as adjunctive therapy as part of a regimen for the suppression of the normal bacterial flora of the bowel, e.g., preoperative preparation of the bowel. It is given concomitantly with erythromycin enteric-coated base. /Included in US product label/
NIH; DailyMed. Current Medication Information for Neomycin Sulfate (Neomycin Sulfate Tablet) (Updated: June 2016). Available from, as of February 16, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3114c827-1923-437a-bc8a-a1ac20327a28
Neomycin sulfate has been shown to be effective adjunctive therapy in hepatic coma by reduction of the ammonia-forming bacteria in the intestinal tract. The subsequent reduction in blood ammonia has resulted in neurologic improvement. /Included in US product label/
NIH; DailyMed. Current Medication Information for Neomycin Sulfate (Neomycin Sulfate Tablet) (Updated: June 2016). Available from, as of February 16, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3114c827-1923-437a-bc8a-a1ac20327a28
For more Therapeutic Uses (Complete) data for Neomycin (14 total), please visit the HSDB record page.
/BOXED WARNING/ WARNINGS SYSTEMIC ABSORPTION OF NEOMYCIN OCCURS FOLLOWING ORAL ADMINISTRATION AND TOXIC REACTIONS MAY OCCUR. Patients treated with neomycin should be under close clinical observation because of the potential toxicity associated with their use. NEUROTOXICITY (INCLUDING OTOTOXICITY) AND NEPHROTOXICITY FOLLOWING THE ORAL USE OF NEOMYCIN SULFATE HAVE BEEN REPORTED, EVEN WHEN USED IN RECOMMENDED DOSES. THE POTENTIAL FOR NEPHROTOXICITY, PERMANENT BILATERAL AUDITORY OTOTOXICITY AND SOMETIMES VESTIBULAR TOXICITY IS PRESENT IN PATIENTS WITH NORMAL RENAL FUNCTION WHEN TREATED WITH HIGHER DOSES OF NEOMYCIN AND/OR FOR LONGER PERIODS THAN RECOMMENDED. Serial, vestibular and audiometric tests, as well as tests of renal function, should be performed (especially in high-risk patients). THE RISK OF NEPHROTOXICITY AND OTOTOXICITY IS GREATER IN PATIENTS WITH IMPAIRED RENAL FUNCTION. Ototoxicity is often delayed in onset and patients developing cochlear damage will not have symptoms during therapy to warn them of developing eighth nerve destruction and total or partial deafness may occur long after neomycin has been discontinued. Neuromuscular blockage and respiratory paralysis have been reported following the oral use of neomycin. The possibility of the occurrence of neuromuscular blockage and respiratory paralysis should be considered if neomycin is administered, especially to patients receiving anesthetics, neuromuscular blocking agents such as tubocurarine, succinylcholine, decamethonium, or in patients receiving massive transfusions of citrate anticoagulated blood. If blockage occurs, calcium salts may reverse these phenomena but mechanical respiratory assistance may be necessary. Concurrent and/or sequential systemic, oral or topical use of other aminoglycosides, including paromomycin and other potentially nephrotoxic and/or neurotoxic drugs such as bacitracin, cisplatin, vancomycin, amphotericin B, polymyxin B, colistin and viomycin, should be avoided because the toxicity may be additive. Other factors which increase the risk of toxicity are advanced age and dehydration. The concurrent use of neomycin with potent diuretics such as ethacrynic acid or furosemide should be avoided, since certain diuretics by themselves may cause ototoxicity. In addition, when administered intravenously, diuretics may enhance neomycin toxicity by altering the antibiotic concentration in serum and tissue.
NIH; DailyMed. Current Medication Information for Neomycin Sulfate (Neomycin Sulfate Tablet) (Updated: June 2016). Available from, as of February 16, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3114c827-1923-437a-bc8a-a1ac20327a28
VET: Ototoxicity, neuromuscular blockade, and nephrotoxicity are reported most frequently; these effects may vary with the aminoglycoside and dose or interval used, but all members of the group are potentially toxic. Nephrotoxicity is of major concern and may result in renal failure due to acute tubular necrosis with secondary interstitial damage. Aminoglycosides accumulate in proximal tubular epithelial cells, where they are sequestered in lysosomes and interact with ribosomes, mitochondria, and other intracellular constituents to cause cell injury. The greater the ionization (eg, the more the amine groups and the lower the pH), the greater the active uptake. Kidneys must have a drug-free period to eliminate accumulated drugs. As such, persistence of aminoglycosides in plasma and thus urine is likely to predispose the tubular cells to toxicity, and the risk may by reduced by allowing plasma drug concentrations to drop below recommended concentrations (generally 1-2 ug/mL) before the next dose. Nonoliguric renal failure is the usual observation; it is generally reversible if damage is not sufficiently extensive to harm the basement membrane, although recovery may be prolonged. /Aminoglycosides/
Kahn, C.M (ed.).; The Merck Veterinary Manual 10th Edition. Merck & Co. Whitehouse Station NJ. 2010, p. 2277-8
VET: Renal function should be monitored during therapy; however, no indicator of renal disease is sufficiently sensitive to prevent continued damage once nephrotoxicity is detected. Polyuria, decreased urine osmolality, enzymuria, proteinuria, cylindruria, and increased fractional sodium excretion are indicative of aminoglycoside nephrotoxicity. Later, BUN and creatinine concentrations may be increased. Early changes or evidence of nephrotoxicity can be detected in 3-5 days, with more overt signs in 7-10 days. Several factors predispose to aminoglycoside nephrotoxicosis, including age (with young (especially the newborn foal) and old animals being sensitive), compromised renal function, total dose, duration of treatment, dehydration and hypovolemia, aciduria, acidosis, hypomagnesemia, severe sepsis or endotoxemia, concurrent administration of furosemide, and exposure to other potential nephrotoxins (eg, methoxyflurane, amphotericin B, cisplatinum, and perhaps some cephalosporins). In renal insufficiency, generally the interval between doses is prolonged (rather than reducing the dose) to minimize toxicity, while avoiding a negative impact on efficacy. Dosing in the morning may decrease toxicity in diurnal animals. The risk of toxicity is less in alkaline urine. Nephroactive drugs, including those that alter renal vascular response (eg, autoregulation) should be avoided or used cautiously (eg, NSAIDs, diuretics). Treatment with N-acetylcysteine should be considered. /Aminoglycosides/
Kahn, C.M (ed.).; The Merck Veterinary Manual 10th Edition. Merck & Co. Whitehouse Station NJ. 2010, p. 2278
VET: Aminoglycosides can cause ototoxicity, which may manifest as either auditory or vestibular dysfunction. Binding or damage to mitochondria plays a prominent role in ototoxicity. Vestibular injury leads to nystagmus, incoordination, and loss of the righting reflex. The lesion is often irreversible, although physiologic adaptation can occur. Ototoxicity is not unusual in people, but relevance to veterinary patients is not clear. Cats are particularly sensitive to the toxic vestibular effects, although occurrence at therapeutic concentrations after systemic administration is unlikely. However, aminoglycosides should not be administered topically into the ear unless the tympanic membrane is intact. Hearing impairment reflects permanent damage and loss of the hair cells in the organ of Corti. Loss of high-frequency hearing is followed by deafness, which may not be complete if sufficiently low doses or durations were used. Aminoglycosides should be avoided in working dogs that depend on hearing (eg, guide dogs). Factors increasing the risk of vestibular and cochlear damage are the same as for nephrotoxicity but also include preexisting acoustic or vestibular impairment and concurrent treatment with potentially ototoxic drugs. The ototoxic potential is greatest for gentamicin, sisomicin, and neomycin, and least for netilmicin. In people, treatment with N-acetylcysteine has deceased the risk of aminoglycoside ototoxicity. /Aminoglycosides/
Kahn, C.M (ed.).; The Merck Veterinary Manual 10th Edition. Merck & Co. Whitehouse Station NJ. 2010, p. 2278
For more Drug Warnings (Complete) data for Neomycin (39 total), please visit the HSDB record page.
For the treatment of bacterial blepharitis, bacterial bonjunctivitis, corneal injuries, corneal ulcers and meibomianitis. For the prophylaxis of ocular infections following foreign body removal
Oral neomycin sulfate is indicated as an adjunctive therapy in hepatic coma (portal-system encephalopathy) by reducing ammonia-forming bacteria in the intestinal tract. It is strongly recommended that oral neomycin is only used in infections that are proven or strongly suspected to be caused by susceptible bacteria to reduce the risk of the development of drug-resistant bacteria. Neomycin, in combination with polymyxin B sulfates and hydrocortisone in otic suspensions, is used in the treatment of superficial bacterial infections of the external auditory canal caused by organisms susceptible to the antibiotics. This otic formulation is also used in the treatment of infections of mastoidectomy and fenestration cavities caused by organisms susceptible to the antibiotics. The ophthalmic solution containing neomycin in combination with polymyxin B sulfates and dexamethasone is used to treat steroid-responsive inflammatory ocular conditions for which a corticosteroid is indicated and where bacterial infection or a risk of bacterial infection exists.
FDA Label
Framycetin is used for the treatment of bacterial eye infections such as conjunctivitis. Framycetin is an antibiotic. It is not active against fungi, viruses and most kinds of anaerobic bacteria. Framycetin works by binding to the bacterial 30S ribosomal subunit, causing misreading of t-RNA, leaving the bacterium unable to synthesize proteins vital to its growth. Framycetin is useful primarily in infections involving aerobic bacteria bacteria.
Neomycin mediates its bactericidal action by inhibiting bacterial protein synthesis, thereby suppressing the growth and survival of susceptible bacteria. Following oral administration, the duration of bactericidal activity of neomycin ranged from 48 to 72 hours. By decreasing colonic bacteria that produce ammonia, neomycin was shown to be effective as an adjunctive therapy in hepatic coma to improve neurologic symptoms. Neomycin is active against both gram positive and gram negative organisms, including the major _E. coli_ species resident in the colon as well as the enteropathogenic forms of _E. coli_. It is also active against _Klebsiella_-_Enterobacter_ group. Resistant strains of _E. coli_, _Klebsiella_ and _Proteus spp_. may emerge from neomycin therapy. Neomycin has no antifungal activity and has some activity against some protozoa.
Anti-Bacterial Agents
Substances that inhibit the growth or reproduction of BACTERIA. (See all compounds classified as Anti-Bacterial Agents.)
R01AX08
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
A - Alimentary tract and metabolism
A01 - Stomatological preparations
A01A - Stomatological preparations
A01AB - Antiinfectives and antiseptics for local oral treatment
A01AB08 - Neomycin
A - Alimentary tract and metabolism
A07 - Antidiarrheals, intestinal antiinflammatory/antiinfective agents
A07A - Intestinal antiinfectives
A07AA - Antibiotics
A07AA01 - Neomycin
B - Blood and blood forming organs
B05 - Blood substitutes and perfusion solutions
B05C - Irrigating solutions
B05CA - Antiinfectives
B05CA09 - Neomycin
D - Dermatologicals
D06 - Antibiotics and chemotherapeutics for dermatological use
D06A - Antibiotics for topical use
D06AX - Other antibiotics for topical use
D06AX04 - Neomycin
D - Dermatologicals
D09 - Medicated dressings
D09A - Medicated dressings
D09AA - Medicated dressings with antiinfectives
D09AA01 - Framycetin
J - Antiinfectives for systemic use
J01 - Antibacterials for systemic use
J01G - Aminoglycoside antibacterials
J01GB - Other aminoglycosides
J01GB05 - Neomycin
R - Respiratory system
R01 - Nasal preparations
R01A - Decongestants and other nasal preparations for topical use
R01AX - Other nasal preparations
R01AX08 - Framycetin
R - Respiratory system
R02 - Throat preparations
R02A - Throat preparations
R02AB - Antibiotics
R02AB01 - Neomycin
S - Sensory organs
S01 - Ophthalmologicals
S01A - Antiinfectives
S01AA - Antibiotics
S01AA03 - Neomycin
S - Sensory organs
S01 - Ophthalmologicals
S01A - Antiinfectives
S01AA - Antibiotics
S01AA07 - Framycetin
S - Sensory organs
S02 - Otologicals
S02A - Antiinfectives
S02AA - Antiinfectives
S02AA07 - Neomycin
S - Sensory organs
S03 - Ophthalmological and otological preparations
S03A - Antiinfectives
S03AA - Antiinfectives
S03AA01 - Neomycin
Absorption
Neomycin is poorly absorbed from the gastrointestinal tract. Gastrointestinal absorption of the drug may be increased if inflammatory or ulcerative gastrointestinal disease is present.
Route of Elimination
The small absorbed fraction of neomycin is excreted by the kidney. The unabsorbed portion of the drug is excreted unchanged in the feces.
Volume of Distribution
The small fraction of absorbed neomycin is rapidly distributed in the tissues. The amount of systemically absorbed neomycin is reported to increase cumulatively with each repeated dose administered until a steady state is reached.
Clearance
There is limited information on the clearance rate of neomycin.
Neomycin sulfate is poorly absorbed from the normal gastrointestinal tract. The small absorbed fraction is rapidly distributed in the tissues and is excreted by the kidney in keeping with the degree of kidney function. The unabsorbed portion of the drug (approximately 97%) is eliminated unchanged in the feces.
NIH; DailyMed. Current Medication Information for Neomycin Sulfate (Neomycin Sulfate Tablet) (Updated: June 2016). Available from, as of February 16, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3114c827-1923-437a-bc8a-a1ac20327a28
As with other aminoglycosides, the amount of systemically absorbed neomycin transferred to the tissues increases cumulatively with each repeated dose administered until a steady state is achieved. The kidney functions as the primary excretory path as well as the tissue binding site, with the highest concentration found in the renal cortex. With repeated dosings, progressive accumulation also occurs in the inner ear. Release of tissue-bound neomycin occurs slowly over a period of several weeks after dosing has been discontinued.
NIH; DailyMed. Current Medication Information for Neomycin Sulfate (Neomycin Sulfate Tablet) (Updated: June 2016). Available from, as of February 16, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3114c827-1923-437a-bc8a-a1ac20327a28
In one study in adults with normal renal function, a single 4-g oral dose of neomycin sulfate produced peak plasma neomycin concentrations of 2.5-6.1 ug/mL 1-4 hours after the dose in most patients; low plasma concentrations of the drug were detectable at 8 hours but the drug was undetectable at 24 hours.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016
In adults who received 1-g doses of oral neomycin sulfate and 1-g doses of oral erythromycin at 19, 18, and 9 hours before colorectal surgery, mean peak serum concentrations of neomycin were 0.59 ug/mL and were attained 12 hours after the first dose (i.e., 2 hours after the third dose).
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016
For more Absorption, Distribution and Excretion (Complete) data for Neomycin (16 total), please visit the HSDB record page.
There is limited information on the metabolism of neomycin, as there is limited systemic absorption following drug administration. Metabolism is deemed to be negligible.
Aminoglycosides are not metabolized and are excreted unchanged in the urine primarily by glomerular filtration. /Aminoglycosides/
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 31
There is limited information on the half-life of neomycin.
The plasma elimination half-life of neomycin usually is 2-3 hours in adults with normal renal function and has been reported to be 12-24 hours in adults with severe renal impairment.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016
Framycetin binds to specific 30S-subunit proteins and 16S rRNA, four nucleotides of 16S rRNA and a single amino acid of protein S12. This interferes with decoding site in the vicinity of nucleotide 1400 in 16S rRNA of 30S subunit. This region interacts with the wobble base in the anticodon of tRNA. This leads to interference with the initiation complex, misreading of mRNA so incorrect amino acids are inserted into the polypeptide leading to nonfunctional or toxic peptides and the breakup of polysomes into nonfunctional monosomes.
Like other aminoglycoside antibiotic drugs, neomycin inhibits bacterial ribosomes by binding to the 30S ribosomal subunit of susceptible bacteria and disrupting the translational machinery of bacterial protein synthesis. Bacterial translation is normally initiated by the mRNA binding to the 30S ribosomal subunit and subsequent binding with 50S subunit for elongation.
Aminoglycosides are usually bactericidal in action. Although the exact mechanism of action has not been fully elucidated, the drugs appear to inhibit protein synthesis in susceptible bacteria by irreversibly binding to 30S ribosomal subunits. /Aminoglycosides/
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 29
A class of angiogenesis inhibitor has emerged from our mechanistic study of the action of angiogenin, a potent angiogenic factor. Neomycin, an aminoglycoside antibiotic, inhibits nuclear translocation of human angiogenin in human endothelial cells, an essential step for angiogenin-induced angiogenesis. The phospholipase C-inhibiting activity of neomycin appears to be involved, because U-73122, another phospholipase C inhibitor, has a similar effect. In contrast, genistein, oxophenylarsine, and staurosporine, inhibitors of tyrosine kinase, phosphotyrosine phosphatase, and protein kinase C, respectively, do not inhibit nuclear translocation of angiogenin. Neomycin inhibits angiogenin-induced proliferation of human endothelial cells in a dose-dependent manner. At 50 microM, neomycin abolishes angiogenin-induced proliferation but does not affect the basal level of proliferation and cell viability. Other aminoglycoside antibiotics, including gentamicin, streptomycin, kanamycin, amikacin, and paromomycin, have no effect on angiogenin-induced cell proliferation. Most importantly, neomycin completely inhibits angiogenin-induced angiogenesis in the chicken chorioallantoic membrane at a dose as low as 20 ng per egg. These results suggest that neomycin and its analogs are a class of agents that may be developed for anti-angiogenin therapy.
Hu G; Proc Natl Acad Sci U S A 95(17): p.9791-9795 (1998)
... Aminoglycosides are aminocyclitols that kill bacteria by inhibiting protein synthesis as they bind to the 16S rRNA and by disrupting the integrity of bacterial cell membrane. Aminoglycoside resistance mechanisms include: (a) the deactivation of aminoglycosides by N-acetylation, adenylylation or O-phosphorylation, (b) the reduction of the intracellular concentration of aminoglycosides by changes in outer membrane permeability, decreased inner membrane transport, active efflux, and drug trapping, (c) the alteration of the 30S ribosomal subunit target by mutation, and (d) methylation of the aminoglycoside binding site. ... /Aminoglycosides/
PMID:17657587 Shakil S et al; J Biomed Sci 15 (1): 5-14 (2008)