

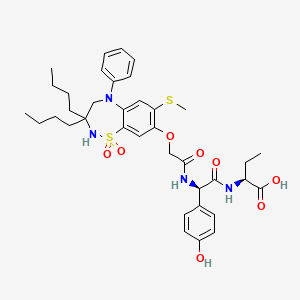
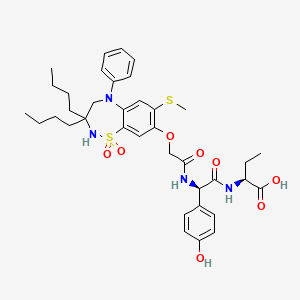
1. (2s)-2-(((2r)-2-((((3,3-dibutyl-7-(methylsulfanyl)-1,1-dioxido-5-phenyl-2,3,4,5-tetrahydro-1,2,5-benzothiadiazepin-8-yl)oxy)acetyl)amino)-2-(4-hydroxyphenyl)acetyl)amino)butanoic Acid
2. Bylvay
1. 501692-44-0
2. Azd8294
3. A4250
4. Ar-h064974
5. Odevixibat [usan]
6. A-4250
7. 2w150k0uuc
8. Azd-8294
9. Odevixibat (usan)
10. (2s)-2-[[(2r)-2-[[2-[(3,3-dibutyl-7-methylsulfanyl-1,1-dioxo-5-phenyl-2,4-dihydro-1lambda6,2,5-benzothiadiazepin-8-yl)oxy]acetyl]amino]-2-(4-hydroxyphenyl)acetyl]amino]butanoic Acid
11. (s)-2-((r)-2-(2-((3,3-dibutyl-7-(methylthio)-1,1-dioxido-5-phenyl-2,3,4,5-tetrahydrobenzo[f][1,2,5]thiadiazepin-8-yl)oxy)acetamido)-2-(4-hydroxyphenyl)acetamido)butanoic Acid
12. Butanoic Acid, 2-(((2r)-((((3,3-dibutyl-2,3,4,5-tetrahydro-7-(methylthio)-1,1-dioxido-5-phenyl-1,2,5-benzothiadiazepin-8-yl)oxy)acetyl)amino)(4-hydroxyphenyl)acetyl)amino)-, (2s)-
13. Butanoic Acid, 2-(((2r)-2-((2-((3,3-dibutyl-2,3,4,5-tetrahydro-7-(methylthio)-1,1-dioxido-5-phenyl-1,2,5-benzothiadiazepin-8-yl)oxy)acetyl)amino)-2-(4-hydroxyphenyl)acetyl)amino)-, (2s)-
14. Odevixibat [inn]
15. Odevixibat [who-dd]
16. Unii-2w150k0uuc
17. Schembl946468
18. Chembl4297588
19. Odevixibat [orange Book]
20. Bdbm77040
21. Gtpl11194
22. Dtxsid601336860
23. Ex-a5384
24. Example 5 [us9694018b1]
25. Who 10706
26. At28924
27. Bo181253
28. Hy-109120
29. Unk-d-ntyr-abu-oh (iupac Condensed Name)
30. Cs-0078340
31. D11716
32. Us9694018, 5
33. (2s)-2-(((2r)-2-((((3,3-dibutyl-7-(methylthio)-1,1-dioxido-5-phenyl-2,3,4,5-tetrahydro- 1,2,5-benzothiadiazepin-8-yl)oxy)acetyl)amino)-2-(4-hydroxyphenyl)acetyl)amino)butanoic Acid
| Molecular Weight | 740.9 g/mol |
|---|---|
| Molecular Formula | C37H48N4O8S2 |
| XLogP3 | 6.8 |
| Hydrogen Bond Donor Count | 5 |
| Hydrogen Bond Acceptor Count | 11 |
| Rotatable Bond Count | 17 |
| Exact Mass | 740.29135685 g/mol |
| Monoisotopic Mass | 740.29135685 g/mol |
| Topological Polar Surface Area | 208 Ų |
| Heavy Atom Count | 51 |
| Formal Charge | 0 |
| Complexity | 1230 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 2 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Odevixibat is indicated for the treatment of pruritus in patients older than 3 months, with progressive familiar intrahepatic cholestasis (PFIC). It may not be effective in PFIC type 2 with ABCB11 variants. These patients lack a functional bile salt export pump.
Treatment of biliary atresia
Treatment of Progressive Familial Intrahepatic Cholestasis
Bylvay is indicated for the treatment of progressive familial intrahepatic cholestasis (PFIC) in patients aged 6 months or older (see sections 4. 4 and 5. 1).
Treatment of Alagille syndrome
Odevixibat, or A4250, is an ileal sodium/bile acid cotransporter inhibitor indicated for the treatment of pruritus in patients older than 3 months, with progressive familiar intrahepatic cholestasis (PFIC). It has a moderate duration of action as it is given once daily. Odevixibat has a wide therapeutic index as patients were given single doses up to 10 mg while the maximum therapeutic dose is 6 mg daily. Patients should be counselled regarding the risks of elevated liver function tests, diarrhea, and fat soluble vitamin defiencies.
A05AX
A - Alimentary tract and metabolism
A05 - Bile and liver therapy
A05A - Bile therapy
A05AX - Other drugs for bile therapy
A05AX05 - Odevixibat
Absorption
A 7.2 mg single oral dose of odevixibat in adults reaches a Cmax of 0.47 ng/mL, with an AUC0-24h of 2.19 h\*ng/mL. The majority of adult and pediatric patients, given a therapeutic dose, do not have detectable plasma concentrations of odevixibat.
Route of Elimination
Odevixibat is 82.9% recovered in the feces and <0.002% recovered in the urine. The dose recovered in the feces is 97% unchanged parent compound.
Volume of Distribution
The majority of adult and pediatric patients, given a therapeutic dose, do not have detectable plasma concentrations of odevixibat. Therefore, a volume of distribution has not been calculated.
Clearance
The majority of adult and pediatric patients, given a therapeutic dose, do not have detectable plasma concentrations of odevixibat. Therefore, the clearance has not been calculated.
Odevixibat is largely unmetabolized, however a small amount is metabolized _in vitro_ by mono-hydroxylation. The exact structure of the metabolite has not been characterized as a primary endpoint of the clinical trial was to characterize the structure of metabolites accounting for >10% of the dose in plasma, urine, or feces. No metabolites have been identified at such a high concentration.
A 7.2 mg oral dose of odevixibat has a mean half life of 2.36 hours in adults.
Progressive familiar intrahepatic cholestasis (PFIC) is a group of autosomal recessive disorders leading to cholestasis, fibrosis, and eventually a need for liver transplantation. Patients with PFIC require liver transplants or develop hepatocellular carcinomas in their first few years of life. Many of these patients experience severe pruritus. The exact mechanism of pruritus is PFIC is not known, but lower concentrations of bile acids have been shown to reduce pruritus. Patients with certain forms of PFIC type 2, associated with a non-functional or absent bile salt export pump, are not expected to benefit from odevixibat treatment. The ileal sodium/bile acid cotransporter is a transport glycoprotein responsible for reabsorption of 95% of bile acids in the distal ileum. Odevixibat is a reversible inhibitor of the ileal sodium/bile acid contransporter. Patients taking odevixibat for a week experienced a 56% reduction in bile acid area under the curve with a 3 mg once daily dose. A 1.5 mg daily dose lead to a 43% reduction in bile acid area under the curve. The decreased reabsorption of bile acids, leads to reduced stimulation of FXR, which reduces expression of FGF19, reducing binding of FGF19 to FGF4R, decreasing inhibition of bile acid synthesis. Further synthesis of bile acids that will not be reabsorbed in the intestine contributes to lowering low density lipoprotein levels.