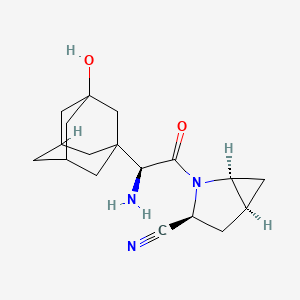
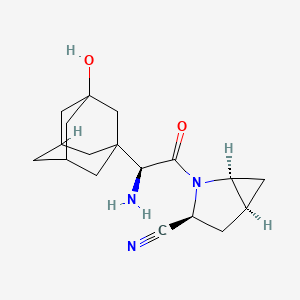
1. 3-hydroxyadamantylglycine-4,5-methanoprolinenitrile Hydrate
2. Bms 477118
3. Bms-477118
4. Bms477118
5. Saxagliptin
1. Saxagliptin
2. 361442-04-8
3. Bms-477118
4. Saxagliptin [inn]
5. Bms 477118
6. Opc-262
7. Saxagliptin Anhydrous
8. 8i7io46ivq
9. Chembl385517
10. Chebi:71272
11. Bms477118
12. (1s,3s,5s)-2-((2s)-2-amino-2-(3-hydroxyadamantan-1-yl)acetyl)-2-azabicyclo[3.1.0]hexane-3-carbonitrile
13. (1s,3s,5s)-2-((2s)-amino(3-hydroxytricyclo(3.3.1.13,7)dec-1-yl)acetyl)-2-azabicyclo(3.1.0)hexane-3-carbonitrile
14. (1s,3s,5s)-2-[(2s)-2-amino-2-(3-hydroxyadamantan-1-yl)acetyl]-2-azabicyclo[3.1.0]hexane-3-carbonitrile
15. 945667-22-1
16. (1s,3s,5s)-2-[(2s)-2-amino-2-(3-hydroxy-1-adamantyl)acetyl]-2-azabicyclo[3.1.0]hexane-3-carbonitrile
17. (1s,3s,5s)-2-[(2s)-2-amino-2-[(1r,3r,5r,7s)-3-hydroxyadamantan-1-yl]acetyl]-2-azabicyclo[3.1.0]hexane-3-carbonitrile
18. Unii-8i7io46ivq
19. Saxagliptine
20. Saxagliptin (bms-477118,onglyza)
21. Hsdb 8199
22. Opc 262
23. Ncgc00242597-01
24. Saxagliptin [mi]
25. 1073057-20-1
26. Saxagliptin (usan/inn)
27. Dsstox_cid_28506
28. Dsstox_rid_82778
29. Dsstox_gsid_48580
30. Schembl17168
31. Saxagliptin [who-dd]
32. Mls006011223
33. Gtpl6316
34. Saxagliptin - Bms-477118
35. Dtxsid7048580
36. Schembl20243458
37. Bdbm11542
38. Hms3264p11
39. Pharmakon1600-01502500
40. Tox21_112908
41. Bdbm50225074
42. Mfcd12756398
43. Nsc760407
44. S1540
45. Akos015896547
46. Ac-6008
47. Ccg-213084
48. Ccg-267647
49. Cs-0650
50. Db06335
51. Ex-7795
52. Ncgc00242597-02
53. Ncgc00242597-10
54. 2-azabicyclo[3.1.0]hexane-3-carbonitrile, 2-[(2s)-2-amino-2-(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)acetyl]-, (1s,3s,5s)-
55. Hy-10285
56. Smr004702984
57. Am20090693
58. Cas-361442-04-8
59. D08996
60. Ab01562984_01
61. Ab01562984_02
62. Q3121121
63. Brd-a81513827-001-03-6
64. Z2235802036
65. (s)-3-hydroxyadamantylglycine-l-cis-4,5-methanoprolinenitrile Tfa Salt
66. (1s,6s)-2-(2-adamantan-1-yl-2-amino-acetyl)-2-aza-bicyclo[3.1.0]hexane-3-carbonitrile
67. (1s,3s,5s)-2-((2s)-amino(3-hydroxytricyclo(3.3.1.1(sup 3,7))dec-1-yl)acetyl)-2-azabicyclo(3.1.0)hexane-3-carbonitrile
68. (1s,3s,5s)-2-[(2s)-2-amino-2-(3-hydroxyadamantan-1-yl)acetyl]-2-azabicyclo[3.1.0]hexane-3-carbonitrile; 2,2,2-trifluoroacetic Acid
69. (1s,3s,5s)-2-[(2s)-2-amino-2-(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)-1-oxoethyl]-2-azabicyclo[3.1.0]hexane-3-carbonitrile
70. (1s,3s,5s)-2-[(s)-2-amino-2-(3-hydroxy-adamantan-1-yl)-acetyl]-2-aza-bicyclo[3.1.0]hexane-3-carbonitrile
71. 2-azabicyclo(3.1.0)hexane-3-carbonitrile, 2-((2s)-amino(3-hydroxytricyclo(3.3.1.1(sup 3,7))dec-1-yl)acetyl), (1s,3s,5s)-
72. 2-azabicyclo(3.1.0)hexane-3-carbonitrile, 2-((2s)-amino(3-hydroxytricyclo(3.3.1.13,7)dec-1-yl)acetyl) , (1s,3s,5s)-
73. 2-azabicyclo[3.1.0]hexane-3-carbonitrile,2-[(2s)-amino(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)acetyl]-, (1s,3s,5s)-
| Molecular Weight | 315.4 g/mol |
|---|---|
| Molecular Formula | C18H25N3O2 |
| XLogP3 | 0.7 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 2 |
| Exact Mass | 315.19467705 g/mol |
| Monoisotopic Mass | 315.19467705 g/mol |
| Topological Polar Surface Area | 90.4 Ų |
| Heavy Atom Count | 23 |
| Formal Charge | 0 |
| Complexity | 609 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 4 |
| Undefined Atom Stereocenter Count | 2 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Onglyza is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus in multiple clinical settings. /Included in US product label/
NIH; DailyMed. Current Medication Information for Onglyza (Saxagliptin) Tablet, Film-coated (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ba48ac4b-9503-4006-f6e2-3b8a83059c03
Onglyza should not be used for the treatment of type 1 diabetes mellitus or diabetic ketoacidosis, as it would not be effective in these settings.
NIH; DailyMed. Current Medication Information for Onglyza (Saxagliptin) Tablet, Film-coated (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ba48ac4b-9503-4006-f6e2-3b8a83059c03
/BOXED WARNING/ WARNING: LACTIC ACIDOSIS. Lactic acidosis is a rare, but serious, complication that can occur due to metformin accumulation. The risk increases with conditions such as sepsis, dehydration, excess alcohol intake, hepatic impairment, renal impairment, and acute congestive heart failure. The onset of lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, increasing somnolence, and nonspecific abdominal distress. Laboratory abnormalities include low pH, increased anion gap, and elevated blood lactate. If acidosis is suspected, Kombiglyze XR should be discontinued and the patient hospitalized immediately. /Saxagliptin and metformin hydrochloride combination product/
NIH; DailyMed. Current Medication Information for Kombiglyze XR (Saxagliptin and Metformin Hydrochloride) Tablet, Film-coated, Extended Release (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=c1ac4f63-695c-6bd6-4a7f-ecb97e03569e
FDA is evaluating unpublished new findings by a group of academic researchers that suggest an increased risk of pancreatitis and pre-cancerous cellular changes called pancreatic duct metaplasia in patients with type 2 diabetes treated with a class of drugs called incretin mimetics. These findings were based on examination of a small number of pancreatic tissue specimens taken from patients after they died from unspecified causes. FDA has asked the researchers to provide the methodology used to collect and study these specimens and to provide the tissue samples so the Agency can further investigate potential pancreatic toxicity associated with the incretin mimetics. Drugs in the incretin mimetic class include exenatide (Byetta, Bydureon), liraglutide (Victoza), sitagliptin (Januvia, Janumet, Janumet XR, Juvisync), saxagliptin (Onglyza, Kombiglyze XR), alogliptin (Nesina, Kazano, Oseni), and linagliptin (Tradjenta, Jentadueto). These drugs work by mimicking the incretin hormones that the body usually produces naturally to stimulate the release of insulin in response to a meal. They are used along with diet and exercise to lower blood sugar in adults with type 2 diabetes. FDA has not reached any new conclusions about safety risks with incretin mimetic drugs. This early communication is intended only to inform the public and health care professionals that the Agency intends to obtain and evaluate this new information. ... FDA will communicate its final conclusions and recommendations when its review is complete or when the Agency has additional information to report. The Warnings and Precautions section of drug labels and patient Medication Guides for incretin mimetics contain warnings about the risk of acute pancreatitis. FDA has not previously communicated about the potential risk of pre-cancerous findings of the pancreas with incretin mimetics. FDA has not concluded these drugs may cause or contribute to the development of pancreatic cancer. At this time, patients should continue to take their medicine as directed until they talk to their health care professional, and health care professionals should continue to follow the prescribing recommendations in the drug labels. ...
US FDA; Safety Alerts for Human Medicial Products: Incretin Mimetic Drugs for Type 2 Diabetes: Early Communication - Reports of Possible Increased Risk of Pancreatitis and Pre-cancerous Findings of the Pancreas (Posted March 14, 1013). Available from, as of August 1, 2014: https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm343805.htm
Acute pancreatitis has been reported during postmarketing experience in patients receiving saxagliptin therapy. The US Food and Drug Administration (FDA) is evaluating unpublished findings suggesting an increased risk of pancreatitis and precancerous cellular changes (pancreatic duct metaplasia) in patients with type 2 diabetes mellitus receiving incretin mimetics (exenatide, liraglutide, sitagliptin, saxagliptin, alogliptin, or linagliptin). These findings are based on examination of a small number of pancreatic tissue specimens taken from patients who died from unspecified causes while receiving an incretin mimetic. FDA has not yet reached any new conclusions about safety risks with incretin mimetics. FDA will notify healthcare professionals of its conclusions and recommendations when the review is complete or when the agency has additional information to report. FDA states that at this time clinicians should continue to follow the recommendations in the prescribing information for incretin mimetics. The manufacturer states that patients receiving saxagliptin-containing therapy should be monitored for manifestations of pancreatitis. If pancreatitis is suspected, saxagliptin should be promptly discontinued and appropriate management instituted. Saxagliptin has not been studied in patients with a history of pancreatitis and it is not known whether such patients are at increased risk for pancreatitis with saxagliptin therapy.
American Society of Health-System Pharmacists 2014; Drug Information 2014. Bethesda, MD. 2014, p. 3208
... There have been postmarketing reports of serious allergic and hypersensitivity reactions (e.g., anaphylaxis, angioedema, exfoliative skin conditions). The onset of such reactions usually was within the first 3 months following treatment initiation; some reactions occurred after the first dose.
American Society of Health-System Pharmacists 2014; Drug Information 2014. Bethesda, MD. 2014, p. 3208
For more Drug Warnings (Complete) data for Saxagliptin (19 total), please visit the HSDB record page.
Treatment of type 2 diabetes mellitus to improve glycemic control in combination with other agents or as monotherapy.
FDA Label
* Add-on combination therapy:
Onglyza is indicated in adult patients aged 18 years and older with type-2 diabetes mellitus to improve glycaemic control:
as monotherapy:
- in patients inadequately controlled by diet and exercise alone and for whom metformin is inappropriate due to contraindications or intolerance;
as dual oral therapy:
- in combination with metformin, when metformin alone, with diet and exercise, does not provide adequate glycaemic control;
- in combination with a sulphonylurea, when the sulphonylurea alone, with diet and exercise, does not provide adequate glycaemic control in patients for whom use of metformin is considered inappropriate;
- in combination with a thiazolidinedione, when the thiazolidinedione alone with diet and exercise, does not provide adequate glycaemic control in patients for whom use of a thiazolidinedione is considered appropriate;
as triple oral therapy:
- in combination with metformin plus a sulphonylurea when this regimen alone, with diet and exercise, does not provide adequate glycaemic control;
as combination therapy with insulin (with or without metformin), when this regimen alone, with diet and exercise, does not provide adequate glycaemic control.
Post-administration of saxagliptin, GLP-1 and GIP levels rise up to 2- to 3- fold. Because it is very selective of DPP-4 inhibition, there are fewer systemic side effects. Saxagliptin inhibits DPP-4 enzyme activity for a 24-hour period. It also decreased glucagon concentrations and increased glucose-dependent insulin secretion from pancreatic beta cells. The half maximal inhibitory concentration (IC50) is 0.5 nmol/L. Saxagliptin did not prolong the QTc interval to a clinically significant degree.
Dipeptidyl-Peptidase IV Inhibitors
Compounds that suppress the degradation of INCRETINS by blocking the action of DIPEPTIDYL-PEPTIDASE IV. This helps to correct the defective INSULIN and GLUCAGON secretion characteristic of TYPE 2 DIABETES MELLITUS by stimulating insulin secretion and suppressing glucagon release. (See all compounds classified as Dipeptidyl-Peptidase IV Inhibitors.)
Incretins
Peptides which stimulate INSULIN release from the PANCREATIC BETA CELLS following oral nutrient ingestion, or postprandially. (See all compounds classified as Incretins.)
A10BH03
A10BH03
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
A - Alimentary tract and metabolism
A10 - Drugs used in diabetes
A10B - Blood glucose lowering drugs, excl. insulins
A10BH - Dipeptidyl peptidase 4 (dpp-4) inhibitors
A10BH03 - Saxagliptin
Absorption
Following a 5 mg single oral dose of saxagliptin to healthy subjects, the mean plasma AUC values for saxagliptin and its active metabolite were 78 ngh/mL and 214 ngh/mL, respectively. The corresponding plasma Cmax values were 24 ng/mL and 47 ng/mL, respectively. Saxagliptin did not accumulate following repeated doses. The median time to maximum concentration (Tmax) following the 5 mg once daily dose was 2 hours for saxagliptin and 4 hours for its active metabolite. Bioavailability, 2.5 - 50 mg dose = 67%
Route of Elimination
Saxagliptin is eliminated by both renal and hepatic pathways. Following a single 50 mg dose of 14C-saxagliptin, 24%, 36%, and 75% of the dose was excreted in the urine as saxagliptin, its active metabolite, and total radioactivity, respectively. A total of 22% of the administered radioactivity was recovered in feces representing the fraction of the saxagliptin dose excreted in bile and/or unabsorbed drug from the gastrointestinal tract.
Volume of Distribution
151 L
Clearance
Renal clearance, single 50 mg dose = 14 L/h
A single-dose, open-label study was conducted to evaluate the pharmacokinetics of saxagliptin (10 mg dose) in subjects with varying degrees of chronic renal impairment (N=8 per group) compared to subjects with normal renal function. The 10 mg dosage is not an approved dosage. The study included patients with renal impairment classified on the basis of creatinine clearance as mild (>50 to =80 mL/min), moderate (30 to =50 mL/min), and severe (<30 mL/min), as well as patients with end-stage renal disease on hemodialysis. ... The degree of renal impairment did not affect the Cmax of saxagliptin or its active metabolite. In subjects with mild renal impairment, the AUC values of saxagliptin and its active metabolite were 20% and 70% higher, respectively, than AUC values in subjects with normal renal function. Because increases of this magnitude are not considered to be clinically relevant, dosage adjustment in patients with mild renal impairment is not recommended. In subjects with moderate or severe renal impairment, the AUC values of saxagliptin and its active metabolite were up to 2.1- and 4.5-fold higher, respectively, than AUC values in subjects with normal renal function. To achieve plasma exposures of saxagliptin and its active metabolite similar to those in patients with normal renal function, the recommended dose is 2.5 mg once daily in patients with moderate and severe renal impairment, as well as in patients with end-stage renal disease requiring hemodialysis. Saxagliptin is removed by hemodialysis.
NIH; DailyMed. Current Medication Information for Onglyza (Saxagliptin) Tablet, Film-coated (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ba48ac4b-9503-4006-f6e2-3b8a83059c03
Saxagliptin is eliminated by both renal and hepatic pathways. Following a single 50 mg dose of (14)-C-saxagliptin, 24%, 36%, and 75% of the dose was excreted in the urine as saxagliptin, its active metabolite, and total radioactivity, respectively. The average renal clearance of saxagliptin (~230 mL/min) was greater than the average estimated glomerular filtration rate (approximately 120 mL/min), suggesting some active renal excretion. A total of 22% of the administered radioactivity was recovered in feces representing the fraction of the saxagliptin dose excreted in bile and/or unabsorbed drug from the gastrointestinal tract.
NIH; DailyMed. Current Medication Information for Onglyza (Saxagliptin) Tablet, Film-coated (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ba48ac4b-9503-4006-f6e2-3b8a83059c03
Saxagliptin was rapidly absorbed after oral administration in the fasted state, with maximum plasma concentrations (Cmax) of saxagliptin and its major metabolite attained within 2 and 4 hours (Tmax), respectively. The Cmax and AUC values of saxagliptin and its major metabolite increased proportionally with the increment in the saxagliptin dose, and this dose-proportionality was observed in doses up to 400 mg. Following a 5 mg single oral dose of saxagliptin to healthy subjects, the mean plasma AUC values for saxagliptin and its major metabolite were 78 ng*hr/mL and 214 ng*hr/mL, respectively. The corresponding plasma Cmax values were 24 ng/mL and 47 ng/mL, respectively. The intra-subject coefficients of variation for saxagliptin Cmax and AUC were less than 12%.
European Medicines Agency (EMEA); European Public Assessment Report for Authorized Medicinal Products for Human Use; Product Information Annex I Summary of Product Characteristics; p.12 (September 9, 2013). Available from, as of August 1, 2014: https://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/001039/human_med_000947.jsp&mid=WC0b01ac058001d124
The metabolism of saxagliptin is primarily mediated by cytochrome P450 3A4/5 (CYP3A4/5). 50% of the absorbed dose will undergo hepatic metabolism. The major metabolite of saxagliptin, 5-hydroxy saxagliptin, is also a DPP4 inhibitor, which is one-half as potent as saxagliptin.
The metabolism of saxagliptin is primarily mediated by CYP3A4/5. In in vitro studies, saxagliptin and its active metabolite did not inhibit CYP1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, or 3A4, or induce CYP1A2, 2B6, 2C9, or 3A4. Therefore, saxagliptin is not expected to alter the metabolic clearance of coadministered drugs that are metabolized by these enzymes. Saxagliptin is a P-glycoprotein (P-gp) substrate but is not a significant inhibitor or inducer of P-gp. ... The major metabolite of saxagliptin is also a DPP4 inhibitor, which is one-half as potent as saxagliptin.
NIH; DailyMed. Current Medication Information for Onglyza (Saxagliptin) Tablet, Film-coated (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ba48ac4b-9503-4006-f6e2-3b8a83059c03
Saxagliptin = 2.5 hours; 5-hydroxy saxagliptin = 3.1 hours;
Following a single oral dose of Onglyza 5 mg to healthy subjects, the mean plasma terminal half-life for saxagliptin and its active metabolite was 2.5 and 3.1 hours, respectively.
NIH; DailyMed. Current Medication Information for Onglyza (Saxagliptin) Tablet, Film-coated (Revised: May 2013). Available from, as of July 18, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ba48ac4b-9503-4006-f6e2-3b8a83059c03
Saxagliptin is a dipeptidyl peptidase-4 (DPP-4) inhibitor antidiabetic for the treatment of type 2 diabetes. DPP-4 inhibitors are a class of compounds that work by affecting the action of natural hormones in the body called incretins. Incretins decrease blood sugar by increasing consumption of sugar by the body, mainly through increasing insulin production in the pancreas, and by reducing production of sugar by the liver. [Bristol-Myers Squibb Press Release] DPP-4 is a membrane associated peptidase which is found in many tissues, lymphocytes and plasma. DPP-4 has two main mechanisms of action, an enzymatic function and another mechanism where DPP-4 binds adenosine deaminase, which conveys intracellular signals via dimerization when activated. Saxagliptin forms a reversible, histidine-assisted covalent bond between its nitrile group and the S630 hydroxyl oxygen on DPP-4. The inhibition of DPP-4 increases levels active of glucagon like peptide 1 (GLP-1), which inhibits glucagon production from pancreatic alpha cells and increases production of insulin from pancreatic beta cells.
Type 2 diabetes (T2D) is one of the major risk factors associated with Alzheimer's disease (AD). Recent studies have found similarities in molecular mechanisms that underlie the respective degenerative developments in the two diseases. Pharmacological agents, such as dipeptidyl peptidase-4 (DPP-4) inhibitors, which increase the level of glucagon-like peptide-1 (GLP-1) and ameliorate T2D, have become valuable candidates as disease modifying agents in the treatment of AD. In addition, endogenous GLP-1 levels decrease amyloid beta (Abeta) peptide and tau phosphorylation in AD. The present study examines the efficacy of Saxagliptin, a DPP-4 inhibitor in a streptozotocin (STZ) induced rat model of AD. Three months following induction of AD by intracerebral administration of streptozotocin, animals were orally administered Saxagliptin (0.25, 0.5 and 1 mg/kg) for 60 days. The effect of the DPP-4 inhibitor on hippocampal GLP-1 levels, Abeta burden, tau phosphorylation, inflammatory markers and memory retention were evaluated. The results reveal an attenuation of Abeta, tau phosphorylation and inflammatory markers and an improvement in hippocampal GLP-1 and memory retention following treatment. This remarkable therapeutic effect of Saxagliptin mediated through DPP-4 inhibition demonstrates a unique mechanism for Abeta and tau clearance by increasing GLP-1 levels and reverses the behavioural deficits and pathology observed in AD.
PMID:23603201 Kosaraju J et al; Neuropharmacology 72: 291-300 (2013) doi: 10.1016/j.neuropharm.2013.04.008.
Saxagliptin inhibits dipeptidyl peptidase-4 (DPP-4), an enzyme that inactivates incretin hormones glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). Both saxagliptin and its active metabolite (5-hydroxy saxagliptin) are more selective for inhibition of DPP-4 than for DPP-8 or DPP-9. Saxagliptin increases circulating levels of GLP-1 and GIP in a glucose-dependent manner. GLP-1 and GIP stimulate insulin secretion from pancreatic beta-cells in a glucose-dependent manner (i.e., when glucose concentrations are normal or elevated). GLP-1 also decreases glucagon secretion from pancreatic alpha-cells, leading to reduced hepatic glucose production. Saxagliptin lowers fasting plasma glucose concentrations and reduces glucose excursions following a glucose load or meal in patients with type 2 diabetes mellitus.
American Society of Health-System Pharmacists 2014; Drug Information 2014. Bethesda, MD. 2014, p. 3209