1. Anhydrous Tacrolimus
2. Anhydrous, Tacrolimus
3. Fk 506
4. Fk-506
5. Fk506
6. Fr 900506
7. Fr-900506
8. Fr900506
9. Prograf
10. Prograft
11. Tacrolimus Anhydrous
12. Tacrolimus, Anhydrous
1. Fujimycin
2. 104987-11-3
3. Prograf
4. Tsukubaenolide
5. Protopic
6. Fk506
7. Tacrolimus Anhydrous
8. Anhydrous Tacrolimus
9. Modigraf
10. Fk-506
11. Protopy
12. Lcp-tacro
13. Advagraf
14. Tacrolimus (fk506)
15. Fk 506
16. Fr-900506
17. Tacrolimus, Anhydrous
18. 8-deethyl-8-[but-3-enyl]-ascomycin
19. Tacrolimus (inn)
20. Fr900506
21. Astagraf Xl
22. Envarsus Xr
23. (-)-fk 506
24. Prograf (tn)
25. Tacrolimus [usan]
26. Chembl269732
27. Chebi:61049
28. Y5l2157c4j
29. Nsc-758659
30. K506
31. Ncgc00163470-03
32. Prograft
33. Tacrolimus [inn]
34. Avagraf
35. Envarsus
36. Graceptor
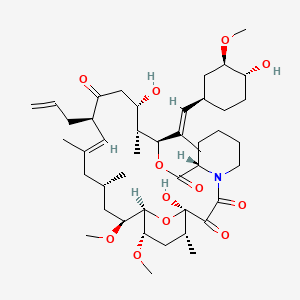
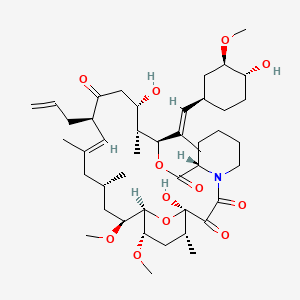
37. (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-[(1e)-2-[(1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl]-1-methylethenyl]-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propen-1-yl)-15,19-epoxy-3h-pyrido[2,1-c][1,4]oxaazacyclotricosine-1,7,20,21(4h,23h)tetrone
38. Fk-506 (tacrolimus)
39. Tacrolimus (anhydrous)
40. Sr-05000001879
41. Tacrolimus [usan:inn]
42. Hecoria
43. Talymus
44. Unii-y5l2157c4j
45. Ccris 7124
46. Mfcd00869853
47. Hsdb 8195
48. L 679934
49. Prograph
50. Tacro
51. Envarsus-xr
52. Tacrolimus [mi]
53. Schembl3088
54. Tacrolimus [mart.]
55. Dsstox_cid_26354
56. Dsstox_rid_81557
57. Tacrolimus [who-dd]
58. Dsstox_gsid_46354
59. Bspbio_001279
60. Chembl66247
61. L-679934
62. Gtpl6784
63. Dtxsid5046354
64. Chebi:93221
65. Hms503o21
66. Hms1792o21
67. Hms1990o21
68. Hms2093m19
69. Hms3403o21
70. Pharmakon1600-01503968
71. Ex-a1677
72. Tox21_112056
73. Bdbm50030448
74. Bdbm50079777
75. Lmpk04000003
76. Nsc758659
77. S5003
78. Akos005145901
79. Zinc169289411
80. Ac-1182
81. Am81227
82. Ccg-270494
83. Cs-1507
84. Db00864
85. Idi1_001040
86. Ncgc00163470-01
87. Ncgc00163470-02
88. Ncgc00163470-04
89. Ncgc00163470-05
90. Ncgc00163470-06
91. Ncgc00163470-07
92. Ncgc00163470-27
93. (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-5,19-dihydroxy-3-{(1e)-1-[(1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl]prop-1-en-2-yl}-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(prop-2-en-1-yl)-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-3h-15,19-epoxypyrido[2,1-c][1,4]oxazacyclotricosine-1,7,20,21(4h,23h)-tetrone
94. Hy-13756
95. Sbi-0052894.p002
96. Cas-104987-11-3
97. M2258
98. C01375
99. D08556
100. Ab01209746-01
101. Ab01209746_03
102. 581t933
103. Q411648
104. Q-201775
105. Sr-05000001879-1
106. Sr-05000001879-2
107. Sr-05000001879-5
108. Brd-k35452788-001-02-1
109. Brd-k69608737-001-03-7
110. Brd-k69608737-001-10-2
111. [(e)-2-[(1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl]-1-methylethenyl]-14,16-
112. 15,19-epoxy-3h-pyrido[2,1-c][1,4]oxaazacyclotricosine-1,7,20,21(23h)-tetrone,
113. (1r,9s,12s,13r,14s,17r,18e,21s,23s,24r,25s,27r)-1,14-dihydroxy-12-[(e)-1-[(1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl]prop-1-en-2-yl]-23,25-dimethoxy-13,19,21,27-tetramethyl-17-prop-2-enyl-11,28-dioxa-4-azatricyclo[22.3.1.04,9]octacos-18-ene-2,3,10,16-tetrone
114. (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-5,19-dihydroxy-3-{(e)-2-[(1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl]-1-methylethenyl}-14,16-dimethoxy-4,10,12,18-tetramethyl-8-prop-2-en-1-yl-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-3h-15,19-epoxypyrido[2,1-c][1,4]oxazacyclotricosine-1,7,20,21(4h,23h)-tetrone
115. (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-[(1e)-2-[(1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl]-1-methylethenyl]-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propen-1-yl)-15,19
116. (e)-(1r,9s,12s,13r,14r,21s,23s,24r,25s,27r)-17-allyl-1,14-dihydroxy-12-[(e)-2-((3r,4r)-4-hydroxy-3-methoxy-cyclohexyl)-1-methyl-vinyl]-23,25-dimethoxy-13,19,21,27-tetramethyl-11,28-dioxa-4-aza-tricyclo[22.3.1.0*4,9*]octacos-18-ene-2,3,10,16-tetraone
117. 15,19-epoxy-3h-pyrido(2,1-c)(1,4)oxaazacyclotricosine-1,7,20,21(4h,23h)-tetrone, 5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-((1e)-2-((1r,3r,4r)-4-hydroxy-3-methoxycyclohexyl)-1-methylethenyl)-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propen-1-yl)-, (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-
118. 15,19-epoxy-3h-pyrido(2,1-c)(1,4)oxaazacyclotricosine-1,7,20,21(4h,23h)-tetrone, 5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-(2-(4-hydroxy-3-methoxycyclohexyl)-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propenyl)-, (3s-(3r*(e(1s*,3s*,4s*)),4s*,5r*,8s*,9e,12r*,14r*,15s*,16r*,18s*,19s*,26ar*))-
119. 15,19-epoxy-3h-pyrido[2,1-c][1,4]oxaazacyclotricosine-1,7,20,21(4h,23h)-tetrone, 5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-[(1e)-2-[(1r,3r,4r)-4-hydroxy-3-methoxycyc
120. 15,19-epoxy-3h-pyrido[2,1-c][1,4]oxaazacyclotricosine-1,7,20,21(4h,23h)-tetrone, 5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-[(e)-2-[(1r,3r,4r)-4-hydroxy-3-methoxycycl Ohexyl]-1-methylethenyl]-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propen-1-yl)-, (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-
121. 4,5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-heptadecahydro-5,19-dihydroxy-3-
122. Dimethoxy-4,10,12,18-tetramethyl-8-(2-propenyl)-,(3s,4r,5s,8r,12s,14s,15r,16s,18r,19r,26as)-
123. Lohexyl]-1-methylethenyl]-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propen-1-yl)-, (3s,4r,5s,8r,9e,12s,14s,15r,16s,18r,19r,26as)-
124. Tacrolimus Solution, 1.0 Mg/ml In Acetonitrile, Ampule Of 1 Ml, Certified Reference Material
| Molecular Weight | 804.0 g/mol |
|---|---|
| Molecular Formula | C44H69NO12 |
| XLogP3 | 2.7 |
| Hydrogen Bond Donor Count | 3 |
| Hydrogen Bond Acceptor Count | 12 |
| Rotatable Bond Count | 7 |
| Exact Mass | 803.48197664 g/mol |
| Monoisotopic Mass | 803.48197664 g/mol |
| Topological Polar Surface Area | 178 Ų |
| Heavy Atom Count | 57 |
| Formal Charge | 0 |
| Complexity | 1480 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 14 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 2 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 8 | |
|---|---|
| Drug Name | Astagraf xl |
| PubMed Health | Tacrolimus |
| Drug Classes | Antipsoriatic, Immune Suppressant |
| Drug Label | ASTAGRAF XL is available for oral administration as hard gelatin capsules (tacrolimus extended-release capsules) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus USP. Inactive ingredients include ethylcellulose NF, hypromello... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Capsule, extended release |
| Route | Oral |
| Strength | eq 5mg base; eq 0.5mg base; eq 1mg base |
| Market Status | Prescription |
| Company | Astellas |
| 2 of 8 | |
|---|---|
| Drug Name | Prograf |
| PubMed Health | Tacrolimus |
| Drug Classes | Antipsoriatic, Immune Suppressant |
| Drug Label | Prograf is available for oral administration as capsules (tacrolimus capsules USP) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus USP. Inactive ingredients include lactose monohydrate NF, hypromellose USP, croscarmellose so... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Capsule; Injectable |
| Route | Injection; Oral |
| Strength | eq 0.5mg base; eq 5mg base; eq 1mg base; eq 5mg base/ml |
| Market Status | Prescription |
| Company | Astellas |
| 3 of 8 | |
|---|---|
| Drug Name | Protopic |
| PubMed Health | Tacrolimus (On the skin) |
| Drug Classes | Antipsoriatic |
| Drug Label | PROTOPIC (tacrolimus) Ointment contains tacrolimus, a macrolide immunosuppressant produced by Streptomyces tsukubaensis. It is for topical dermatologic use only. Chemically, tacrolimus is designated as [3S-[3R*[E(1S*,3S*,4S*)],4S*,5R*,8S*,9E,12R*,14R... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Ointment |
| Route | Topical |
| Strength | 0.1%; 0.03% |
| Market Status | Prescription |
| Company | Astellas |
| 4 of 8 | |
|---|---|
| Drug Name | Tacrolimus |
| PubMed Health | Tacrolimus |
| Drug Classes | Antipsoriatic, Immune Suppressant |
| Drug Label | Prograf is available for oral administration as capsules (tacrolimus capsules USP) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus USP. Inactive ingredients include lactose monohydrate NF, hypromellose USP, croscarmellose so... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Ointment; Capsule |
| Route | Oral; Topical |
| Strength | eq 5mg base; eq 0.5mg base; 0.1%; eq 1mg base; 0.03% |
| Market Status | Prescription |
| Company | Panacea Biotec; Accord Hlthcare; Sandoz; Strides Pharma; Fougera Pharms; Dr Reddys Labs; Mylan |
| 5 of 8 | |
|---|---|
| Drug Name | Astagraf xl |
| PubMed Health | Tacrolimus |
| Drug Classes | Antipsoriatic, Immune Suppressant |
| Drug Label | ASTAGRAF XL is available for oral administration as hard gelatin capsules (tacrolimus extended-release capsules) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus USP. Inactive ingredients include ethylcellulose NF, hypromello... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Capsule, extended release |
| Route | Oral |
| Strength | eq 5mg base; eq 0.5mg base; eq 1mg base |
| Market Status | Prescription |
| Company | Astellas |
| 6 of 8 | |
|---|---|
| Drug Name | Prograf |
| PubMed Health | Tacrolimus |
| Drug Classes | Antipsoriatic, Immune Suppressant |
| Drug Label | Prograf is available for oral administration as capsules (tacrolimus capsules USP) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus USP. Inactive ingredients include lactose monohydrate NF, hypromellose USP, croscarmellose so... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Capsule; Injectable |
| Route | Injection; Oral |
| Strength | eq 0.5mg base; eq 5mg base; eq 1mg base; eq 5mg base/ml |
| Market Status | Prescription |
| Company | Astellas |
| 7 of 8 | |
|---|---|
| Drug Name | Protopic |
| PubMed Health | Tacrolimus (On the skin) |
| Drug Classes | Antipsoriatic |
| Drug Label | PROTOPIC (tacrolimus) Ointment contains tacrolimus, a macrolide immunosuppressant produced by Streptomyces tsukubaensis. It is for topical dermatologic use only. Chemically, tacrolimus is designated as [3S-[3R*[E(1S*,3S*,4S*)],4S*,5R*,8S*,9E,12R*,14R... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Ointment |
| Route | Topical |
| Strength | 0.1%; 0.03% |
| Market Status | Prescription |
| Company | Astellas |
| 8 of 8 | |
|---|---|
| Drug Name | Tacrolimus |
| PubMed Health | Tacrolimus |
| Drug Classes | Antipsoriatic, Immune Suppressant |
| Drug Label | Prograf is available for oral administration as capsules (tacrolimus capsules USP) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus USP. Inactive ingredients include lactose monohydrate NF, hypromellose USP, croscarmellose so... |
| Active Ingredient | Tacrolimus |
| Dosage Form | Ointment; Capsule |
| Route | Oral; Topical |
| Strength | eq 5mg base; eq 0.5mg base; 0.1%; eq 1mg base; 0.03% |
| Market Status | Prescription |
| Company | Panacea Biotec; Accord Hlthcare; Sandoz; Strides Pharma; Fougera Pharms; Dr Reddys Labs; Mylan |
Immunosuppressive Agents
National Library of Medicine's Medical Subject Headings. Tacrolimus. Online file (MeSH, 2014). Available from, as of April 30 2014: https://www.nlm.nih.gov/mesh/2014/mesh_browser/MBrowser.html
Prograf is indicated for the prophylaxis of organ rejection in patients receiving allogeneic kidney transplants. It is recommended that Prograf be used concomitantly with azathioprine or mycophenolate mofetil (MMF) and adrenal corticosteroids. /Included in US product label/
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
Prograf is indicated for the prophylaxis of organ rejection in patients receiving allogeneic liver transplants. It is recommended that Prograf be used concomitantly with adrenal corticosteroids. Therapeutic drug monitoring is recommended for all patients receiving Prograf. /Included in US product label/
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
Prograf is indicated for the prophylaxis of organ rejection in patients receiving allogeneic heart transplants. It is recommended that Prograf be used concomitantly with azathioprine or mycophenolate mofetil (MMF) and adrenal corticosteroids. /Included in US product label/
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
For more Therapeutic Uses (Complete) data for Tacrolimus (13 total), please visit the HSDB record page.
/BOXED WARNING/ MALIGNANCIES AND SERIOUS INFECTIONS. Increased risk of development of lymphoma and other malignancies, particularly of the skin, due to immunosuppression. Increased susceptibility to bacterial, viral, fungal, and protozoal infections, including opportunistic infections. Only physicians experienced in immunosuppressive therapy and management of organ transplant patients should prescribe Prograf. Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
/BOXED WARNING/ WARNING: Long-term Safety of Topical Calcineurin Inhibitors Has Not Been Established Although a causal relationship has not been established, rare cases of malignancy (e.g., skin and lymphoma) have been reported in patients treated with topical calcineurin inhibitors, including Protopic Ointment. Therefore: Continuous long-term use of topical calcineurin inhibitors, including Protopic Ointment, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis; Protopic Ointment is not indicated for use in children less than 2 years of age; Only 0.03% Protopic Ointment is indicated for use in children 2-15 years of age.
NIH; DailyMed. DailyMed. Current Medication Information for Protopic (Tacrolimus) Ointment (Revised: May 2012). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=8c2e5036-5f1b-4e71-bf87-5faef295fa96
Topical tacrolimus therapy should be avoided for malignant or premalignant skin conditions (e.g., cutaneous T-cell lymphoma (CTCL)), which may appear clinically similar to dermatitis.
American Society of Health-System Pharmacists 2014; Drug Information 2014. Bethesda, MD. 2014
Because of a potential increased risk for skin cancer, patients /using topical tacrolimus/ should be advised to limit exposure to sunlight or other UV light by wearing protective clothing and using a broad-spectrum sunscreen with a high protection factor.
American Society of Health-System Pharmacists 2014; Drug Information 2014. Bethesda, MD. 2014
For more Drug Warnings (Complete) data for Tacrolimus (42 total), please visit the HSDB record page.
For use after allogenic organ transplant to reduce the activity of the patient's immune system and so the risk of organ rejection. It was given FDA approval in 1994 for use in liver transplantation. Since then, this indication has expanded to kidney, heart, small bowel, pancreas, lung, trachea, skin, cornea, and limb transplants. It has also been used in a topical preparation in the treatment of severe atopic dermatitis.
FDA Label
Prophylaxis of transplant rejection in adult kidney or liver allograft recipients.
Treatment of allograft rejection resistant to treatment with other immunosuppressive medicinal products in adult patients.
Prophylaxis of transplant rejection in adult kidney or liver allograft recipients. Treatment of allograft rejection resistant to treatment with other immunosuppressive medicinal products in adult patients.
Prophylaxis of transplant rejection in adult and paediatric, kidney, liver or heart allograft recipients.
Treatment of allograft rejection resistant to treatment with other immunosuppressive medicinal products in adult and paediatric patients.
Prophylaxis of transplant rejection in adult kidney or liver allograft recipients.
Treatment of allograft rejection resistant to treatment with other immunosuppressive medicinal products in adult patients.
* Flare treatment:
Adults and adolescents (16 years of age and above)
Treatment of moderate to severe atopic dermatitis in adults who are not adequately responsive to or are intolerant of conventional therapies such as topical corticosteroids.
Children (two years of age and above)
Treatment of moderate to severe atopic dermatitis in children (two years of age and above) who failed to respond adequately to conventional therapies such as topical corticosteroids.
* Maintenance treatment:
Maintenance treatment of moderate to severe atopic dermatitis for the prevention of flares and the prolongation of flare-free intervals in patients experiencing a high frequency of disease exacerbations (i. e. occurring four or more times per year) who have had an initial response to a maximum of six weeks treatment of twice daily tacrolimus ointment (lesions cleared, almost cleared or mildly affected).
Treatment of moderate to severe atopic dermatitis in adults who are not adequately responsive to or are intolerant of conventional therapies such as topical corticosteroids. Treatment of moderate to severe atopic dermatitis in children (2 years of age and above) who failed to respond adequately to conventional therapies such as topical corticosteroids.
Maintenance treatment of moderate to severe atopic dermatitis for the prevention of flares and the prolongation of flare-free intervals in patients experiencing a high frequency of disease exacerbations (i. e. occurring 4 or more times per year) who have had an initial response to a maximum of 6 weeks treatment of twice daily tacrolimus ointment (lesions cleared, almost cleared or mildly affected).
Prevention of solid organ transplant rejection, Treatment of solid organ transplant rejection
Tacrolimus acts by reducing peptidyl-prolyl isomerase activity by binding to the immunophilin FKBP-12 (FK506 binding protein) creating a new complex. This inhibits both T-lymphocyte signal transduction and IL-2 transcription. Tacrolimus has similar activity to cyclosporine but rates of rejection are lower with tacrolimus. Tacrolimus has also been shown to be effective in the topical treatment of eczema, particularly atopic eczema. It suppresses inflammation in a similar way to steroids, but is not as powerful. An important dermatological advantage of tacrolimus is that it can be used directly on the face; topical steroids cannot be used on the face, as they thin the skin dramatically there. On other parts of the body, topical steroid are generally a better treatment.
Calcineurin Inhibitors
Compounds that inhibit or block the PHOSPHATASE activity of CALCINEURIN. (See all compounds classified as Calcineurin Inhibitors.)
Immunosuppressive Agents
Agents that suppress immune function by one of several mechanisms of action. Classical cytotoxic immunosuppressants act by inhibiting DNA synthesis. Others may act through activation of T-CELLS or by inhibiting the activation of HELPER CELLS. While immunosuppression has been brought about in the past primarily to prevent rejection of transplanted organs, new applications involving mediation of the effects of INTERLEUKINS and other CYTOKINES are emerging. (See all compounds classified as Immunosuppressive Agents.)
L04AD02
L04AD02
L04AD02
L04AD02
D11AH01
D11AX14
L04AD02
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
D - Dermatologicals
D11 - Other dermatological preparations
D11A - Other dermatological preparations
D11AH - Agents for dermatitis, excluding corticosteroids
D11AH01 - Tacrolimus
L - Antineoplastic and immunomodulating agents
L04 - Immunosuppressants
L04A - Immunosuppressants
L04AD - Calcineurin inhibitors
L04AD02 - Tacrolimus
Absorption
Absorption of tacrolimus from the gastrointestinal tract after oral administration is incomplete and variable. The absolute bioavailability in adult kidney transplant patients is 1710%; in adults liver transplant patients is 226%; in healthy subjects is 185%. The absolute bioavailability in pediatric liver transplant patients was 3124%. Tacrolimus maximum blood concentrations (Cmax) and area under the curve (AUC) appeared to increase in a dose-proportional fashion in 18 fasted healthy volunteers receiving a single oral dose of 3, 7, and 10 mg. When given without food, the rate and extent of absorption were the greatest. The time of the meal also affected bioavailability. When given immediately after a meal, mean Cmax was reduced 71%, and mean AUC was reduced 39%, relative to the fasted condition. When administered 1.5 hours following the meal, mean Cmax was reduced 63%, and mean AUC was reduced 39%, relative to the fasted condition.
Route of Elimination
In man, less than 1% of the dose administered is excreted unchanged in urine. When administered IV, fecal elimination accounted for 92.630.7%, urinary elimination accounted for 2.31.1%.
Volume of Distribution
2.6 2.1 L/kg [pediatric liver transplant patients]
1.07 0.20 L/kg [patients with renal impairment, 0.02 mg/kg/4 hr dose, IV]
3.1 1.6 L/kg [Mild Hepatic Impairment, 0.02 mg/kg/4 hr dose, IV]
3.7 4.7 L/kg [Mild Hepatic Impairment, 7.7 mg dose, PO]
3.9 1.0 L/kg [Severe hepatic impairment, 0.02 mg/kg/4 hr dose, IV]
3.1 3.4 L/kg [Severe hepatic impairment, 8 mg dose, PO]
Clearance
0.040 L/hr/kg [healthy subjects, IV]
0.172 0.088 L/hr/kg [healthy subjects, oral]
0.083 L/hr/kg [adult kidney transplant patients, IV]
0.053 L/hr/kg [adult liver transplant patients, IV]
0.051 L/hr/kg [adult heart transplant patients, IV]
0.138 0.071 L/hr/kg [pediatric liver transplant patients]
0.12 0.04 (range 0.06-0.17) L/hr/kg [pediatric kidney transplant patients]
0.038 0.014 L/hr/kg [patients with renal impairment, 0.02 mg/kg/4 hr dose, IV]
0.042 0.02 L/hr/kg [Mild Hepatic Impairment, 0.02 mg/kg/4 hr dose, IV]
0.034 0.019 L/hr/kg [Mild Hepatic Impairment, 7.7 mg dose, PO]
0.017 0.013 L/hr/kg [Severe hepatic impairment, 0.02 mg/kg/4 hr dose, IV]
0.016 0.011 L/hr/kg [Severe hepatic impairment, 8 mg dose, PO]
The aim of this study was to assess tacrolimus levels in breast milk and neonatal exposure during breastfeeding. An observational cohort study was performed in two tertiary referral high-risk obstetric medicine clinics. Fourteen women taking tacrolimus during pregnancy and lactation, and their 15 infants, 11 of whom were exclusively breast-fed, were assessed. Tacrolimus levels were analyzed by liquid chromatography-tandem mass spectrometry. Samples from mothers and cord blood were collected at delivery and from mothers, infants, and breast milk postnatally where possible. All infants with serial sampling had a decline in tacrolimus level, which was approximately 15% per day (ratio of geometric mean concentrations 0.85; 95% confidence interval, 0.82-0.88; P<0.001). Breast-fed infants did not have higher tacrolimus levels compared with bottle-fed infants (median 1.3 ug/L [range, 0.0-4.0] versus 1.0 ug/L (range, 0.0-2.3), respectively; P=0.91). Maximum estimated absorption from breast milk is 0.23% of maternal dose (weight-adjusted). Ingestion of tacrolimus by infants via breast milk is negligible. Breastfeeding does not appear to slow the decline of infant tacrolimus levels from higher levels present at birth.
PMID:23349333 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3613954 Bramham K et al; Clin J Am Soc Nephrol 8 (4): 563-7 (2013)
Maternal and umbilical cord (venous and arterial) samples were obtained at delivery from eight solid organ allograft recipients to measure tacrolimus and metabolite bound and unbound concentrations in blood and plasma. Tacrolimus pharmacokinetics in breast milk were assessed in one subject. Mean (+ or - SD) tacrolimus concentrations at the time of delivery in umbilical cord venous blood (6.6 + or - 1.8 ng ml(-1)) were 71 + or - 18% (range 45-99%) of maternal concentrations (9.0 + or - 3.4 ng ml(-1)). The mean umbilical cord venous plasma (0.09 + or - 0.04 ng ml(-1)) and unbound drug concentrations (0.003 + or - 0.001 ng ml(-1)) were approximately one fifth of the respective maternal concentrations. Arterial umbilical cord blood concentrations of tacrolimus were 100 + or - 12% of umbilical venous concentrations. In addition, infant exposure to tacrolimus through the breast milk was less than 0.3% of the mother's weight-adjusted dose. Differences between maternal and umbilical cord tacrolimus concentrations may be explained in part by placental P-gp function, greater red blood cell partitioning and higher haematocrit levels in venous cord blood.
PMID:23528073 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3845323 Zheng S et al; Br J Clin Pharmacol 76 (6): 988-96 (2013)
Ten colostrum samples were obtained from six women in the immediate postpartum period (0-3 days) with a mean drug concentration of 0.79 ng/mL (range 0.3-1.9 ng/mL). The median milk:maternal plasma ratio was 0.5.
Briggs, G.G., Freeman, R.K., Yaffee, S.J.; Drugs in Pregancy and Lactation Nineth Edition. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, PA. 2011, p. 1385
The plasma protein binding of tacrolimus is approximately 99% and is independent of concentration over a range of 5-50 ng/mL. Tacrolimus is bound mainly to albumin and alpha-1-acid glycoprotein, and has a high level of association with erythrocytes. The distribution of tacrolimus between whole blood and plasma depends on several factors, such as hematocrit, temperature at the time of plasma separation, drug concentration, and plasma protein concentration. In a US study, the ratio of whole blood concentration to plasma concentration averaged 35 (range 12 to 67). There was no evidence based on blood concentrations that tacrolimus accumulates systemically upon intermittent topical application for periods of up to 1 year. As with other topical calcineurin inhibitors, it is not known whether tacrolimus is distributed into the lymphatic system.
NIH; DailyMed. DailyMed. Current Medication Information for Protopic (Tacrolimus) Ointment (Revised: May 2012). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=8c2e5036-5f1b-4e71-bf87-5faef295fa96
For more Absorption, Distribution and Excretion (Complete) data for Tacrolimus (9 total), please visit the HSDB record page.
The metabolism of tacrolimus is predominantly mediated by CYP3A4 and secondarily by CYP3A5. Tacrolimus is metabolized into 8 metabolites: 13-demethyl tacrolimus, 31-demethyl tacrolimus, 15-demethyl tacrolimus, 12-hydroxy tacrolimus, 15,31-didemethyl tacrolimus, 13,31-didemethyl tacrolimus, 13,15-didemethyl tacrolimus, and a final metabolite involving O-demethylation and the formation of a fused ring. The major metabolite identified in incubations with human liver microsomes is 13-demethyl tacrolimus. In in vitro studies, a 31-demethyl metabolite has been reported to have the same activity as tacrolimus.
Tacrolimus is extensively metabolized by the mixed-function oxidase system, primarily the cytochrome P-450 system (CYP3A). A metabolic pathway leading to the formation of 8 possible metabolites has been proposed. Demethylation and hydroxylation were identified as the primary mechanisms of biotransformation in vitro. The major metabolite identified in incubations with human liver microsomes is 13-demethyl tacrolimus. In in vitro studies, a 31-demethyl metabolite has been reported to have the same activity as tacrolimus.
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
Fk_506 has known human metabolites that include 13-O-Desmethyltacrolimus and 15-O-Desmethyltacrolimus.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
The elimination half life in adult healthy volunteers, kidney transplant patients, liver transplants patients, and heart transplant patients are approximately 35, 19, 12, 24 hours, respectively. The elimination half life in pediatric liver transplant patients was 11.53.8 hours, in pediatric kidney transplant patients was 10.25.0 (range 3.4-25) hours.
In a mass balance study of IV administered radiolabeled tacrolimus to 6 healthy volunteers, ... the elimination half-life based on radioactivity was 48.1+ or - 15.9 hours whereas it was 43.5 + or- 11.6 hours based on tacrolimus concentrations. ... When administered PO, the elimination half-life based on radioactivity was 31.9 + or- 10.5 hours whereas it was 48.4 + or - 12.3 hours based on tacrolimus concentrations ... .
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
... A case of tacrolimus toxicity in a non-transplant patient /is presented/. ... /The/ patient's tacrolimus dose was 2.1 mg/kg/day for 4 days (therapeutic 0.03 to 0.05 mg/kg/day). Her tacrolimus elimination half-life was 16.5 hours, compared to a mean half-life in healthy volunteers of 34.2 +/- 7.7 hours. ...
PMID:18608277 O'Connor AD et al; Clin Toxicol (Phila) 46 (9): 838-40 (2008)
The mechanism of action of tacrolimus in atopic dermatitis is not known. While the following have been observed, the clinical significance of these observations in atopic dermatitis is not known. It has been demonstrated that tacrolimus inhibits T-lymphocyte activation by first binding to an intracellular protein, FKBP-12. A complex of tacrolimus-FKBP-12, calcium, calmodulin, and calcineurin is then formed and the phosphatase activity of calcineurin is inhibited. This prevents the dephosphorylation and translocation of nuclear factor of activated T-cells (NF-AT), a nuclear component thought to initiate gene transcription for the formation of lymphokines. Tacrolimus also inhibits the transcription for genes which encode IL-3, IL-4, IL-5, GM-CSF, and TNF-, all of which are involved in the early stages of T-cell activation. Additionally, tacrolimus has been shown to inhibit the release of pre-formed mediators from skin mast cells and basophils, and to downregulate the expression of FceRI on Langerhans cells.
Tacrolimus is a macrolide immunosuppressant produced by Streptomyces tsukubaensis. Tacrolimus is commercially available for topical use as a 0.03 or 0.1% ointment. The exact mechanism(s) of action of tacrolimus in the treatment of atopic dermatitis has not been elucidated but appears to involve inhibition of the activation of T cells. Tacrolimus also has been shown to inhibit release of mediators from skin mast cells and basophils and to downregulate the expression of high-affinity receptors for immunoglobulin E (IgE) on Langerhans cells. Although tacrolimus is not genotoxic and does not interact directly with DNA, the drug may impair local immunosurveillance.
American Society of Health-System Pharmacists 2014; Drug Information 2014. Bethesda, MD. 2014
Tacrolimus inhibits T-lymphocyte activation, although the exact mechanism of action is not known. Experimental evidence suggests that tacrolimus binds to an intracellular protein, FKBP-12. A complex of tacrolimus-FKBP-12, calcium, calmodulin, and calcineurin is then formed and the phosphatase activity of calcineurin inhibited. This effect may prevent the dephosphorylation and translocation of nuclear factor of activated T-cells (NF-AT), a nuclear component thought to initiate gene transcription for the formation of lymphokines (such as interleukin-2, gamma interferon). The net result is the inhibition of T-lymphocyte activation (i.e., immunosuppression).
NIH; DailyMed. Current Medication Information for Prograf (Tacrolimus) Capsule, Gelatin Coated; Prograf (Tacrolimus) Injection, Solution (Revised: September 2013). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7f667de1-9dfa-4bd6-8ba0-15ee2d78873b
The mechanism of action of tacrolimus in atopic dermatitis is not known. While the following have been observed, the clinical significance of these observations in atopic dermatitis is not known. It has been demonstrated that tacrolimus inhibits T-lymphocyte activation by first binding to an intracellular protein, FKBP-12. A complex of tacrolimus-FKBP-12, calcium, calmodulin, and calcineurin is then formed and the phosphatase activity of calcineurin is inhibited. This effect has been shown to prevent the dephosphorylation and translocation of nuclear factor of activated T-cells (NF-AT), a nuclear component thought to initiate gene transcription for the formation of lymphokines (such as interleukin-2, gamma interferon). Tacrolimus also inhibits the transcription for genes which encode IL-3, IL-4, IL-5, GM-CSF, and TNF-a, all of which are involved in the early stages of T-cell activation. Additionally, tacrolimus has been shown to inhibit the release of pre-formed mediators from skin mast cells and basophils, and to down regulate the expression of FceRI on Langerhans cells.
NIH; DailyMed. DailyMed. Current Medication Information for Protopic (Tacrolimus) Ointment (Revised: May 2012). Available from, as of June 17, 2014: https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=8c2e5036-5f1b-4e71-bf87-5faef295fa96
Tacrolimus, formerly known as FK506, is a macrolide antibiotic with immunosuppressive properties. Although structurally unrelated to cyclosporin A (CsA), its mode of action is similar. It exerts its effects principally through impairment of gene expression in target cells. Tacrolimus bonds to an immunophilin, FK506 binding protein (FKBP). This complex inhibits calcineurin phosphatase. The drug inhibits calcium-dependent events, such as interleukin-2 gene transcription, nitric oxide synthase activation, cell degranulation, and apoptosis. Tacrolimus also potentiates the actions of glucocorticoids and progesterone by binding to FKBPs contained within the hormone receptor complex, preventing degradation. The agent may enhance expression of the transforming growth factor beta-1 gene in a fashion analogous to that demonstrated for CsA. T cell proliferation in response to ligation of the T cell receptor is inhibited by tacrolimus. Type 1 T helper cells appear to be preferentially suppressed compared with type 2 T helper cells. T cell-mediated cytotoxicity is impaired. B cell growth and antibody production are affected indirectly by the suppression of T cell-derived growth factors necessary for these functions. Antigen presentation appears to be spared. ...
PMID:8588225 Thomson AW et al; Ther Drug Monit 17 (6): 584-91 (1995)