1. Hpth (1-34)
2. Human Parathyroid Hormone (1-34)
3. Parathar
4. Teriparatide
5. Teriparatide Acetate
1. Parathar
2. Parathyroid Hormone (1-34) (human)
3. 52232-67-4
4. Teriparatida
5. Teriparatidum
6. Teriparatidum [latin]
7. Teriparatida [spanish]
8. Human Parathyroid Hormone (1-34)
9. Human Pth (1-34)
10. Unii-10t9csu89i
11. (1-34)-human Parathormone
12. 1-34-parathormone (human)
13. Parathyroid Hormone (1-34)
14. Mn 10t
15. Hsdb 7367
16. Hpth (1-34)
17. Mn 10-t
18. Teriparatide [usan:inn:ban:jan]
19. Parathyroid Hormone Peptide (1-34)
20. Hpth- (1-34)
21. Zt 034
22. 10t9csu89i
23. Chebi:135983
24. Pth 1-34
25. Akos015994659
26. Hs-2025
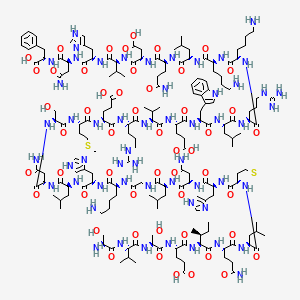
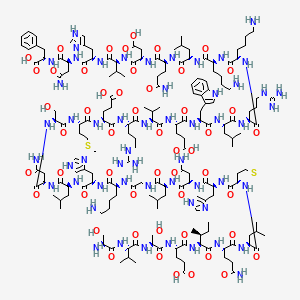
| Molecular Weight | 4118 g/mol |
|---|---|
| Molecular Formula | C181H291N55O51S2 |
| XLogP3 | -18.7 |
| Hydrogen Bond Donor Count | 60 |
| Hydrogen Bond Acceptor Count | 62 |
| Rotatable Bond Count | 146 |
| Exact Mass | 4116.1342973 g/mol |
| Monoisotopic Mass | 4115.1309424 g/mol |
| Topological Polar Surface Area | 1800 Ų |
| Heavy Atom Count | 289 |
| Formal Charge | 0 |
| Complexity | 9740 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 34 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Bone Density Conservation Agents
National Library of Medicine, SIS; ChemIDplus Record for Teriparatide (52232-67-4), MESH Heading. Available from, as of March 15, 2006: https://chem.sis.nlm.nih.gov/chemidplus/chemidlite.jsp
Forteo is indicated for the treatment of postmenopausal women with osteoporosis who are at high risk for fracture. These include women with a history of osteoporotic fracture, or who have multiple risk factors for fracture, or who have failed or are intolerant of previous osteoporosis therapy, based upon physician assessment. In postmenopausal women with osteoporosis, forteo increases BMD and reduces the risk of vertebral and nonvertebral fractures.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1741
Forteo is indicated to increase bone mass in men with primary or hypogonadal osteoporosis who are at high risk for fracture. These include men with a history of osteoporotic fracture, or who have multiple risk factors for fracture, or who have failed or are intolerant to previous osteoporosis therapy, based upon physician assessment. In men with primary or hypogonadal osteoporosis, forteo increases BMD. The effects of forteo on risk for fracture in men have not been studied.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1741
In male and female rats, teriparatide caused an increase in the incidence of osteosarcoma (a malignant bone tumor) that was dependent on dose and treatment duration. The effect was observed at systemic exposures to teriparatide ranging from 3 to 60 times the exposure in humans given a 20-ug dose. Because of the uncertain relevance of the rat osteosarcoma finding to humans, teriparatide should be prescribed only to patients for whom the potential benefits are considered to outweigh the potential risk. Teriparatide should not be prescribed for patients who are at increased baseline risk for osteosarcoma (including those with Paget's disease of bone or unexplained elevations of alkaline phosphatase, open epiphyses, or prior external beam or implant radiation therapy involving the skeleton).
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1739
Adverse effects reported to have been increased by teriparatide treatment in clinical trials included leg cramps and dizziness. Adverse effects reported in at least 2% of patients receiving teriparatide and more frequently than with placebo but without attribution of causality include pain, arthralgia, rhinitis, asthenia, nausea, dizziness, headache, hypertension, increased cough, pharyngitis, constipation, dyspepsia, diarrhea, rash, insomnia, depression, pneumonia, vertigo, dyspnea, neck pain, vomiting, syncope, leg cramps, angina pectoris, GI disorder, sweating, or tooth disorder.
McEvoy, G.K. (ed.). American Hospital Formulary Service- Drug Information 2005. Bethesda, MD: American Society of Health-System Pharmacists, Inc. 2005 (Plus Supplements)., p. 3088
In short-term clinical pharmacology studies with teriparatide, transient episodes of symptomatic orthostatic hypotension were observed infrequently. Typically, an event began within 4 hours of dosing and spontaneously resolved within a few minutes to a few hours. When transient orthostatic hypotension occurred, it happened within the first several doses, it was relieved by placing the person in a reclining position, and it did not preclude continued treatment.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1741
The safety and efficacy of forteo have not been evaluated beyond 2 years of treatment. Consequently, use of the drug for more than 2 years is not recommended. In clinical trials, the frequency of urolithiasis was similar in patients treated with forteo and placebo. However, forteo has not been studied in patients with active urolithiasis. If active urolithiasis or pre-existing hypercalciuria are suspected, measurement of urinary calcium excretion should be considered. Forteo should be used with caution in patients with active or recent urolithiasis because of the potential to exacerbate this condition.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1741
For more Drug Warnings (Complete) data for TERIPARATIDE (13 total), please visit the HSDB record page.
Bone Density Conservation Agents
Agents that inhibit BONE RESORPTION and/or favor BONE MINERALIZATION and BONE REGENERATION. They are used to heal BONE FRACTURES and to treat METABOLIC BONE DISEASES such as OSTEOPOROSIS. (See all compounds classified as Bone Density Conservation Agents.)
Calcium-Regulating Hormones and Agents
Hormones and molecules with calcium-regulating hormone-like actions that modulate OSTEOLYSIS and other extra-skeletal activities to maintain calcium homeostasis. (See all compounds classified as Calcium-Regulating Hormones and Agents.)
Systemic clearance of teriparatide (approximately 62 L/hr in women and 94 L/hr in men) exceeds the rate of normal liver plasma flow, consistent with both hepatic and extra-hepatic clearance. Volume of distribution, following intravenous injection, is approximately 0.12 L/kg. Intersubject variability in systemic clearance and volume of distribution is 25% to 50%.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1739
Teriparatide is extensively absorbed after subcutaneous injection; the absolute bioavailability is approximately 95% based on pooled data from 20-, 40-, and 80-ug doses. The rates of absorption and elimination are rapid. The peptide reaches peak serum concentrations about 30 minutes after subcutaneous injection of a 20-ug dose and declines to non-quantifiable concentrations within 3 hours.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1739
The half-life of teriparatide in serum is 5 minutes when administered by intravenous injection and approximately 1 hour when administered by subcutaneous injection. The longer half-life following subcutaneous administration reflects the time required for absorption from the injection site.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1739
The skeletal effects of teriparatide depend upon the pattern of systemic exposure. Once-daily administration of teriparatide stimulates new bone formation on trabecular and cortical (periosteal and/or endosteal) bone surfaces by preferential stimulation of osteoblastic activity over osteoclastic activity. In monkey studies, teriparatide improved trabecular microarchitecture and increased bone mass and strength by stimulating new bone formation in both cancellous and cortical bone. In humans, the anabolic effects of teriparatide are manifest as an increase in skeletal mass, an increase in markers of bone formation and resorption, and an increase in bone strength. By contrast, continuous excess of endogenous PTH, as occurs in hyperparathyroidism, may be detrimental to the skeleton because bone resorption may be stimulated more than bone formation.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1739
Endogenous 84-amino-acid parathyroid hormone (PTH) is the primary regulator of calcium and phosphate metabolism in bone and kidney. Physiological actions of PTH include regulation of bone metabolism, renal tubular reabsorption of calcium and phosphate, and intestinal calcium absorption. The biological actions of PTH and teriparatide are mediated through binding to specific high-affinity cell-surface receptors. Teriparatide and the 34 N-terminal amino acids of PTH bind to these receptors with the same affinity and have the same physiological actions on bone and kidney. Teriparatide is not expected to accumulate in bone or other tissues.
Physicians Desk Reference 60th ed, Thomson PDR, Montvale, NJ 2006., p. 1739