1. 1-24-acth
2. 1-24-corticotropin
3. Acth (1-24)
4. Acth 1-24
5. Acth, Synthetic
6. Corticotropin (1-24)-peptide
7. Corticotropin (1-24)-tetracosapeptide
8. Cortosyn
9. Cosyntropin
10. Synthetic Acth
11. Tetracosactide
12. Tetracosactrin
13. Tetracosapeptide
1. Cosyntropin
2. Tetracosactide
3. Cortrosyn (tn)
4. Tetracosactrin
5. 16960-16-0
6. Tetracosactide Acetate
7. Cosyntropin (usp)
8. Adrenocorticotropic Hormone Fragment 1-24 Human, Rat
9. Schembl720535
10. Gtpl6965
11. D00284
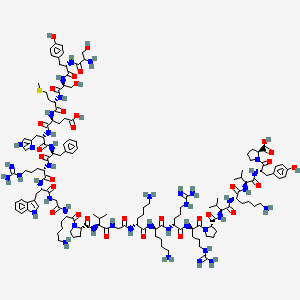
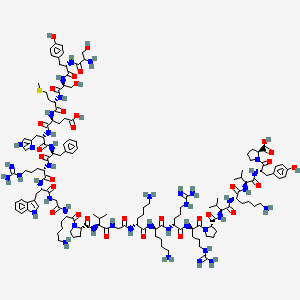
| Molecular Weight | 2933.4 g/mol |
|---|---|
| Molecular Formula | C136H210N40O31S |
| XLogP3 | -7.9 |
| Hydrogen Bond Donor Count | 42 |
| Hydrogen Bond Acceptor Count | 41 |
| Rotatable Bond Count | 96 |
| Exact Mass | 2932.5839961 g/mol |
| Monoisotopic Mass | 2931.5806412 g/mol |
| Topological Polar Surface Area | 1180 Ų |
| Heavy Atom Count | 208 |
| Formal Charge | 0 |
| Complexity | 6500 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 21 |
| Undefined Atom Stereocenter Count | 1 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Cosyntropin is used as an aid in the diagnosis of adrenocortical insufficiency. The 30-minute cosyntropin test provides a good method of screening for primary adrenocortical insufficiency (Addison's disease) and is preferable to corticotropin for rapid screening since it is less likely to cause allergic reactions. When a greater stimulus to the adrenal cortex is desired, corticotropin or cosyntropin may be administered by IV infusion. If subnormal increases in plasma cortisol concentrations occur following administration of corticotropin or cosyntropin, additional tests providing prolonged stimulation of the adrenal cortex are required before impaired adrenocortical function can be diagnosed precisely and differentiation between primary and secondary adrenocortical insufficiency can be established. /Included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Investigationally, long-acting IM depot cosyntropin preparations have been used as an aid in the diagnosis of adrenocortical insufficiency and, in patients with normal adrenocortical function, in the long-term management of chronic inflammatory and degenerative disorders that are responsive to glucocorticoids. /NOT included in US product label/
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
/Experimental therapy/ ... The outcome of children with cryptogenic infantile spasms treated with high-dose synthetic adrenocorticotropic hormone (ACTH) and the relation between early treatment, within 1 month of onset, and outcome /were evaluated/. The long-term cognitive and seizure outcomes of 37 patients with cryptogenic infantile spasms (onset, age 3 to 9 months) receiving standardized treatment regimen of high-dose tetracosactide depot, 1 mg IM every 48 h for 2 weeks, with a subsequent 8- to 10-week slow taper and followed by oral prednisone, 10 mg/day for a month, with a subsequent slow taper for 5 months or until the infant reached the age of 1 year, whichever came later /were assessed/ . Development was assessed before treatment. Seizure outcomes were followed up prospectively. Cognitive outcomes were determined after 6 to 21 years and analyzed in relation to treatment lag and pretreatment regression. Twenty-two infants were treated within 1 month of onset of infantile spasms, and 15 after 1 to 6.5 months. Normal cognitive outcome was found in all 22 (100%) patients of the early-treatment group, and in 40% of the late-treatment group. Normal cognitive outcome was found in all 25 (100%) patients who had no or only mild mental deterioration at presentation, including four in the late-treatment group but in only three of the 12 patients who had had marked or severe deterioration before treatment. Early treatment of cryptogenic infantile spasms with a high-dose ACTH protocol is associated with favorable long-term cognitive outcomes. Once major developmental regression lasts for a month or more, the prognosis for normal cognitive outcome is poor. Further studies are needed on the optimal treatment regimen for this disorder.
PMID:15009227 Kivity S et al; Epilepsia 45 (3): 255-62 (2004).
Indications: Acute exacerbations in patients suffering from multiple sclerosis. Hypsarrhythmia, and or infantile spasms. /Tetracosactrin zinc phosphate complex - depot (NOT available in US)/
Prescribing Information for Synacthen Depot (tetracosactrin zinc phosphate complex); Novartis Pharmaceuticals Australia Pty Ltd (June 2005). Available from, as of March 22, 2010: https://www.novartis.com.au/PI_PDF/synd.pdf
Cosyntropin is less antigenic than corticotropin and is less likely to produce allergic reactions than is corticotropin; however, hypersensitivity reactions have occurred rarely. Patients known to be sensitized to corticotropin and who have markedly positive skin tests usually react negatively when tested intradermally with cosyntropin. Some patients who are hypersensitive to corticotropin preparations may be able to tolerate cosyntropin, but cross-sensitivity reactions may occur. The possibility of hypersensitivity reactions should be considered in all patients receiving cosyntropin, especially in those with preexisting allergic diseases and/or a history of allergic reactions to corticotropin. Patients should be carefully observed for hypersensitivity reactions during and after administration of cosyntropin.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Since Cortrosyn (cosyntropin) for Injection is intended for diagnostic and not therapeutic use, adverse reactions other than a rare hypersensitivity reaction are not anticipated. A rare hypersensitivity reaction usually associated with a pre-existing allergic disease and/or a previous reaction to natural ACTH is possible. Symptoms may include slight whealing with splotchy erythema at the injection site. There have been rare reports of anaphylactic reaction. The following adverse reactions have been reported in patients after the administration of Cortrosyn and the association has been neither confirmed nor refuted: bradycardia, tachycardia, hypertension, peripheral, edema, rash.
US Natl Inst Health; DailyMed. Current Medication Information for CORTROSYN (cosyntropin) injection, powder, for solution (May 2006). Available from, as of February 24, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=3164
FDA Pregnancy Risk Category: C /RISK CANNOT BE RULED OUT. Adequate, well controlled human studies are lacking, and animal studies have shown risk to the fetus or are lacking as well. There is a chance of fetal harm if the drug is given during pregnancy; but the potential benefits may outweigh the potential risk./
US Natl Inst Health; DailyMed. Current Medication Information for CORTROSYN (cosyntropin) injection, powder, for solution (May 2006). Available from, as of February 24, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=3164
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Cortrosyn (cosyntropin) for Injection is administered to a nursing woman.
US Natl Inst Health; DailyMed. Current Medication Information for CORTROSYN (cosyntropin) injection, powder, for solution (May 2006). Available from, as of February 24, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=3164
For more Drug Warnings (Complete) data for Cosyntropin (15 total), please visit the HSDB record page.
Hormones
Chemical substances having a specific regulatory effect on the activity of a certain organ or organs. The term was originally applied to substances secreted by various ENDOCRINE GLANDS and transported in the bloodstream to the target organs. It is sometimes extended to include those substances that are not produced by the endocrine glands but that have similar effects. (See all compounds classified as Hormones.)
H - Systemic hormonal preparations, excl. sex hormones and insulins
H01 - Pituitary and hypothalamic hormones and analogues
H01A - Anterior pituitary lobe hormones and analogues
H01AA - Acth
H01AA02 - Tetracosactide
Cosyntropin is rapidly absorbed following IM administration.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Adsorption of tetracosactrin on to zinc phosphate provides for sustained release of the active substance from the intramuscular injection site. After an injection of a mg Synacthen Depot IM, the radioimmunologically determined plasma concentrations of tetracosactrin lie for 12 hours between 200 and 300 pg/mL. Tetracosactrin has an apparent distribution volume of approximately 0.4 L/kg. /Tetracosactrin zinc phosphate complex - depot (NOT available in US)/
Prescribing Information for Synacthen Depot (tetracosactrin zinc phosphate complex); Novartis Pharmaceuticals Australia Pty Ltd (June 2005). Available from, as of March 22, 2010: https://www.novartis.com.au/PI_PDF/synd.pdf
The precise distribution and metabolic fate of cosyntropin is not known, but the drug is rapidly removed from the plasma by many tissues. Cosyntropin apparently does not cross the placenta.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)
Cosyntropin elicits all the pharmacologic responses usually produced by endogenous corticotropin; however, cosyntropin is immunologically much less active than corticotropin since most of the antigenic activity of corticotropin has been attributed to the C-terminal portion of the molecule (i.e., the 22-39 amino acid residues). In patients with normal adrenocortical function, cosyntropin stimulates the adrenal cortex to secrete cortisol (hydrocortisone), corticosterone, several weakly androgenic substances, and to a very limited extent aldosterone. When cosyntropin is used diagnostically, the effect of the drug is usually measured by determining plasma cortisol concentrations prior to and following administration of the drug. In patients with primary adrenocortical insufficiency (Addison's disease), cosyntropin does not substantially increase plasma cortisol concentrations.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009)