1. Calciferols
2. D2, Vitamin
3. Ergocalciferols
4. Vitamin D 2
5. Vitamin D2
1. Vitamin D2
2. Calciferol
3. 50-14-6
4. Viosterol
5. Ergorone
6. Ercalciol
7. Deltalin
8. Drisdol
9. Ostelin
10. Oleovitamin D2
11. Sterogyl
12. Detalup
13. Condocaps
14. Crystallina
15. Fortodyl
16. Mulsiferol
17. Radsterin
18. Condol
19. Deratol
20. Diactol
21. Ertron
22. Geltabs
23. Daral
24. Novovitamin-d
25. Divit Urto
26. D-tracetten
27. Hi-deratol
28. Calciferon 2
29. Dee-ronal
30. Vitavel-d
31. D-arthin
32. Dee-ron
33. De-rat Concentrate
34. Vio-d
35. Rodine C
36. Activated Ergosterol
37. Calciferolum
38. Hyperkil
39. Rodinec
40. Ergocalciferolum
41. Mina D2
42. Vitamind2
43. Viosterol In Oil
44. Radiostol
45. Haliver
46. Davitin
47. Metadee
48. Mykostin
49. (+)-vitamin D2
50. Decaps
51. Infron
52. Shock-ferol
53. Davitamon D
54. Dee-osterol
55. Geltabs Vitamin D
56. Dee-roual
57. Buco-d
58. Oleovitamin D, Synthetic
59. Uvesterol D
60. Oleovitamin D
61. Chebi:28934
62. Irradiated Ergosta-5,7,22-trien-3-beta-ol
63. Synthetic Vitamin D
64. Vitamin D (ergocalciferol)
65. Condacaps
66. Viostdrol
67. Crtron
68. 9,10-secoergosta-5,7,10(19),22-tetraen-3-beta-ol
69. Vs041h42xc
70. Uvesterol-d
71. (3s,5z,7e,22e)-9,10-secoergosta-5,7,10,22-tetraen-3-ol
72. (5z,7e,22e)-(3s)-9,10-seco-5,7,10(19),22-ergostatetraen-3-ol
73. Ergosterol Activated
74. Mfcd00166988
75. Nsc-62792
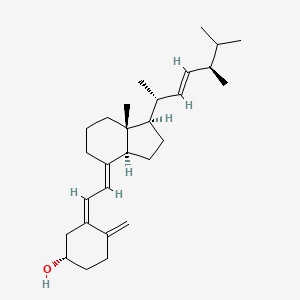
76. (1s,3z)-3-[(2e)-2-[(1r,3as,7ar)-1-[(e,2r,5r)-5,6-dimethylhept-3-en-2-yl]-7a-methyl-2,3,3a,5,6,7-hexahydro-1h-inden-4-ylidene]ethylidene]-4-methylidenecyclohexan-1-ol
77. Ergocalciferols
78. Dsstox_cid_233
79. (3beta,5z,7e,22e)-9,10-secoergosta-5,7,10(19),22-tetraen-3-ol
80. (5z,7e,22e)-(3s)-9,10-secoergosta-5,7,10(19),22-tetraen-3-ol
81. 9,10-secoergosta-5,7,10(19),22-tetraen-3-ol, (3b,5z,7e,22e)-
82. 9,10-secoergosta-5,7,10(19),22-tetraen-3-ol, (3.beta.,5z,7e,22e)-
83. Dsstox_rid_75449
84. Dsstox_gsid_20233
85. Vitamin D2 (ergocalciferol)
86. Ergocalciferolo
87. Disdrol
88. Radstein
89. Vd2-d3
90. Ergocalciferolo [dcit]
91. Smr000857106
92. Ergocalciferolum [inn-latin]
93. Vitamin D 2
94. Ergosterol Irradiated
95. Irradiated Ergosterol
96. Shock-ferol Sterogyl
97. Hsdb 819
98. Sorex C.r.
99. Einecs 200-014-9
100. Nsc 62792
101. Doral [vitamin Derivative]
102. Unii-vs041h42xc
103. Osteil
104. Delta-tracetten
105. Lanes
106. Delta-arthin
107. Beta-ol
108. D-forte
109. Ergocalciferol Oil
110. Eciferol D2
111. Vitamina D2
112. Calciferol (tn)
113. Cas-50-14-6
114. Ergoral D2
115. Ncgc00166307-01
116. Sterogyl-15
117. Sterogyl 15h
118. Cyclohexanol, 4-methylene-3-((2e)-2-((1r,3as,7ar)-octahydro-7a-methyl-1-((1r,2e,4r)-1,4,5-trimethyl-2-hexen-1-yl)-4h-inden-4-ylidene)ethylidene)-, (1s,3z)-
119. Cyclohexanol, 4-methylene-3-[(2e)-2-[(1r,3as,7ar)-octahydro-7a-methyl-1-[(1r,2e,4r)-1,4,5-trimethyl-2-hexen-1-yl]-4h-inden-4-ylidene]ethylidene]-, (1s,3z)-
120. Prestwick_554
121. Drisdol (tn)
122. Vio D
123. Ergocalciferol [usp:inn:ban:jan]
124. Vitamin D2 Solution
125. Ergo-d2
126. Osto-d2
127. Calciferol In Arach Oil
128. 9,10-seco(5z,7e,22e)-5,7,10(19),22-ergostatetraen-3-ol
129. Prestwick3_000420
130. Bmse000510
131. Vitamin D2 [mi]
132. (3-beta,5z,7e,22e)-9,10-secoergosta-5,7,10,(19),22-tetraen-3-ol
133. Vitamin D2 [fcc]
134. Schembl3420
135. Chembl1536
136. Ergocalciferol [inn]
137. Ergocalciferol [jan]
138. Ergocalciferol; 50-14-6
139. Bspbio_000380
140. Ergocalciferol (jp17/usp)
141. Ergocalciferol [hsdb]
142. Ergocalciferol [inci]
143. Mls001332467
144. Mls001332468
145. Ergocalciferol [vandf]
146. Vitamin D2 [who-ip]
147. Ergocalciferol [mart.]
148. Ergocalciferol, (+)-
149. Bpbio1_000418
150. Megxm0_000466
151. Ergocalciferol [usp-rs]
152. Ergocalciferol [who-dd]
153. Ergocalciferol [who-ip]
154. Dtxsid5020233
155. Acon1_002187
156. Hms2096c22
157. Hms2230e20
158. 1217448-46-8
159. Act02622
160. Cs-m1019
161. Zinc4629876
162. Ergocalciferol [ep Impurity]
163. Ergocalciferol [orange Book]
164. Tox21_112404
165. Tox21_202348
166. Tox21_302752
167. Bdbm50247883
168. Ergocalciferol [ep Monograph]
169. Lmst03010001
170. S4035
171. Ergocalciferol [usp Monograph]
172. Vitamin D2; Ergocalciferol; Deltalin
173. 9,10-secoergosta-5,7,10(19),22-tetraen-3-ol, (3beta,5z,7e,22e)-
174. Akos022185284
175. Ccg-268614
176. Db00153
177. Ergocalciferolum [who-ip Latin]
178. Ergocalciferol, Sigma Reference Standard
179. Ncgc00166307-02
180. Ncgc00166307-03
181. Ncgc00256529-01
182. Ncgc00259897-01
183. As-11649
184. Bp-31119
185. Ergocalciferol (d2), Analytical Standard
186. Hy-76542
187. Irradiated Ergosta-5,7,22-trien-3beta-ol
188. Vitamin D2 Ergocalciferol 400,000 Iu/g
189. Ergocalciferol, 40,000,000 Usp Units/g
190. C05441
191. D00187
192. 166v988
193. Q139200
194. Q-201930
195. 9,10-secoergosta-5,7,10(19),22-tetraen-3b-ol
196. Ergocalciferol, >=98.0% (sum Of Enantiomers, Hplc)
197. 22-tetraen 3beta 9,10,secoergosta-5,7,10(19)-ol
198. 7e677dc1-e1c4-4fc5-8f4a-bce1857f7e87
199. Vitamin D2 Solution, 100 Mug/ml In Ethanol, 98% (cp)
200. (5e,7e,22e)-9,10-secoergosta-5,7,10,22-tetraen-3-ol
201. Ergocalciferol, British Pharmacopoeia (bp) Reference Standard
202. Ergocalciferol, European Pharmacopoeia (ep) Reference Standard
203. Ergocalciferol, United States Pharmacopeia (usp) Reference Standard
204. (3s,5z,7e,22e)-9,10-secoergosta-5,7,10(19),22-tetraen-3-ol
205. Vitamin D2. Short Expiry Date Due To Chemical Nature Of Component(s)
206. (3.beta.,5z,7e,22e)-9,10-secoergosta-5,7,10(19),22-tetraen-3-ol
207. 24-methyl-9,10-secocholesta-5,7,10( 19),22-tetraene-3.beta.-ol [who-ip]
208. Ergocalciferol (vitamin D2), Pharmaceutical Secondary Standard; Certified Reference Material
209. Ergocalciferol For System Suitability, Europepharmacopoeia (ep) Reference Standard
210. Vitamin D2 Solution, 1 Mg/ml In Ethanol, Ampule Of 1 Ml, Certified Reference Material
211. (1s,3z)-3-[(2e)-2-[(1r,3as,7ar)-7a-methyl-1-[(e,1r,4r)-1,4,5-trimethylhex-2-enyl]-2,3,3a,5,6,7-hexahydro-1h-inden-4-ylidene]ethylidene]-4-methylene-cyclohexanol
212. 4-methylene-3-[2-[tetrahydro-7a-methyl-1-(1,4,5-trimethyl-2-hexenyl)-4(3ah)-indanylidene]ethylidene]-cyclohexanol
| Molecular Weight | 396.6 g/mol |
|---|---|
| Molecular Formula | C28H44O |
| XLogP3 | 7.4 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 1 |
| Rotatable Bond Count | 5 |
| Exact Mass | 396.339216023 g/mol |
| Monoisotopic Mass | 396.339216023 g/mol |
| Topological Polar Surface Area | 20.2 Ų |
| Heavy Atom Count | 29 |
| Formal Charge | 0 |
| Complexity | 678 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 6 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 3 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
MEDICATION (VET): ... Recommended for prophylaxis of milk fever in cows. ... Prevent atrophic rhinitis in pigs. ... Aid fracture healing in cats and dogs.
Rossoff, I.S. Handbook of Veterinary Drugs. New York: Springer Publishing Company, 1974., p. 653
MEDICATION (VET): To be effective ... supplementation with Ca & PO4. ... Fish meals & irradiated yeast may be used as supplemental ... source. ... Diets are routinely supplemented ... 1400-1600 IU/kg. Therapy for rickets ... Level 10-20 times daily requirement, alternate days for 1 wk. /Vitamin D/
Jones, L.M., et al. Veterinary Pharmacology & Therapeutics. 4th ed. Ames: Iowa State University Press, 1977., p. 773
In adults and children with nutritional rickets or osteomalacia and normal GI absorption, oral administration of ... ergocalciferol daily results in normal serum calcium and phosphate concentrations in about 10 days, radiographic evidence of healing of bone within 2-4 wk, and complete healing in about 6 months. ... Diet should be corrected and, after healing has occurred, supplemental doses of ergocalciferol may be discontinued in patients with normal GI absorption. In adults with severe malabsorption and vitamin D deficiency, /daily/ dosages ... have been given to correct osteomalacia. In children with malabsorption, oral ergocalciferol dosages ... have been recommended. In vitamin D-deficient infants with tetany and rickets, calcium should be administered orally or iv to control tetany. Vitamin D deficiency is then treated orally with /a daily dose/ of ergocalciferol ... until the bones have healed, ... .
McEvoy, G.K. (ed.). American Hospital Formulary Service- Drug Information 2004. Bethesda, MD: American Society of Health-System Pharmacists, Inc. 2004 (Plus Supplements)., p. 3519
In adults with Fanconi syndrome, oral ergocalciferol .. have been given along with treatment of acidosis. In children with Fanconi syndrome oral ergocalciferol ... have been used.
McEvoy, G.K. (ed.). American Hospital Formulary Service- Drug Information 2004. Bethesda, MD: American Society of Health-System Pharmacists, Inc. 2004 (Plus Supplements)., p. 3519
For more Therapeutic Uses (Complete) data for VITAMIN D2 (11 total), please visit the HSDB record page.
... Ergocalciferol should be administered with extreme caution, if at all, to patients with impaired renal function and with extreme caution in patient with heart disease, renal stones, or arterioscleroses.
McEvoy, G.K. (ed.). American Hospital Formulary Service- Drug Information 2004. Bethesda, MD: American Society of Health-System Pharmacists, Inc. 2004 (Plus Supplements)., p. 3513
Initial signs and symptoms ... consists of weakness, fatigue, lassitude, headache, nausea, vomiting, and diarrhea. Obtundation and coma may develop. Early impairment of renal function from hypercalcemia is manifest by polyuria, polydipsia, nocturia, decreased urinary concentration ability, and proteinuria.
Gilman, A.G., T.W. Rall, A.S. Nies and P. Taylor (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 8th ed. New York, NY. Pergamon Press, 1990., p. 1514
Ergocalciferol is indicated for the treatment of hypoparathyroidism, refractory rickets, and familial hypophosphatemia. Hypoparathyroidism is the result of inadequate parathyroid hormone production that occurs due to the presence of damage or removal of the parathyroid glands. This condition produces decreased calcium and increased phosphorus levels. Rickets is a condition produced due to a deficiency in vitamin D, calcium or phosphorus. However, this condition can also be related to renal diseases. It is characterized to present weak or soft bones. Familial hypophosphatemia is characterized by the impaired transport of phosphate and an altered vitamin D metabolism in the kidneys. The presence of this condition can derive in the presence of osteomalacia, bone softening and rickets.
FDA Label
After the activation of the vitamin D receptor, some of the biological changes produced by ergocalciferol include mobilization and accretion of calcium and phosphorus in the bone, absorption of calcium and phosphorus in the intestine, and reabsorption of calcium and phosphorus in the kidney. Some other effects known to be produced due to the presence of vitamin D are osteoblast formation, fetus development, induction of pancreatic function, induction of neural function, improvement of immune function, cellular growth and cellular differentiation. When compared to its vitamin D counterpart [cholecalciferol], ergocalciferol has been shown to present a reduced induction of calcidiol and hence, it is less potent. Ergocalciferol supplementation in patients with end-stage renal disease has been shown to generate a significant benefit in lab parameters of bone and mineral metabolism as well as improvement in glycemic control, serum albumin levels and reduced levels of inflammatory markers.
Bone Density Conservation Agents
Agents that inhibit BONE RESORPTION and/or favor BONE MINERALIZATION and BONE REGENERATION. They are used to heal BONE FRACTURES and to treat METABOLIC BONE DISEASES such as OSTEOPOROSIS. (See all compounds classified as Bone Density Conservation Agents.)
Calcium-Regulating Hormones and Agents
Hormones and molecules with calcium-regulating hormone-like actions that modulate OSTEOLYSIS and other extra-skeletal activities to maintain calcium homeostasis. (See all compounds classified as Calcium-Regulating Hormones and Agents.)
Vitamins
Organic substances that are required in small amounts for maintenance and growth, but which cannot be manufactured by the human body. (See all compounds classified as Vitamins.)
A - Alimentary tract and metabolism
A11 - Vitamins
A11C - Vitamin a and d, incl. combinations of the two
A11CC - Vitamin d and analogues
A11CC01 - Ergocalciferol
Absorption
Ergocalciferol is absorbed in the intestine and carried to the liver in chylomicrons. Its intestinal absorption does not present limitations unless the presence of conditions related to fat malabsorption. However, for absorption to take place, the presence of bile is required.
Route of Elimination
The active form of ergocalciferol, calcitrol, cannot be maintained for long periods in storage tissue mainly in periods of dietary or UVB deprivation. Therefore, ergocalciferol and its metabolites are excreted via the bile with a minor contribution of renal elimination. This major fecal elimination is explained due to the cubilin-megalin receptor system-mediated renal reuptake of vitamin D metabolites bound to vitamin D binding protein.
Volume of Distribution
The amount of circulating ergocalciferol is very limited as this compound is rapidly stored in fat tissue such as adipose tissue, liver and muscle. This is very obvious in reports that indicate that circulating ergocalciferol is significantly reduced in obese patients.
Clearance
There are no formal reports regarding the clearance rate of ergocalciferol. Due to the structural similarity, it is recommended to consult this parameter with [cholecalciferol]. On the other hand, the proposed renal clearance of calcitriol is of 31 ml/min.
Both vitamin D2 & vitamin D3 are absorbed from the small intestine, although vitamin D3 may be absorbed more efficiently. The exact portion of the gut that is most effective in vitamin D absorption reflects the vehicle in which the vitamin is dissolved. Most of the vitamin appears first within chylomicrons in lymph.
Hardman, J.G., L.E. Limbird, P.B., A.G. Gilman. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. New York, NY: McGraw-Hill, 2001., p. 1729
The presence of bile is required for absorption of ergocalciferol and the extent of GI absorption may be decreased in patients with hepatic, biliary, or GI disease (e.g., Crohn's disease, Whipple's disease, sprue).
McEvoy, G.K. (ed.). American Hospital Formulary Service- Drug Information 2004. Bethesda, MD: American Society of Health-System Pharmacists, Inc. 2004 (Plus Supplements)., p. 3515
A longitudinal, randomized, double blind, placebo controlled study was conducted for 6 months to monitor ultraviolet B light exposure in human milk-fed infants both with and without supplemental vitamin D2, and to measure longitudinally the bone mineral content, growth, and serum concentrations of calcium, phosphorus, 25-hydroxyvitamin D3, 25-hydroxyvitamin D2, 1,25-dihydroxyvitamin D, and parathyroid hormone. Sequential sampling was performed of 46 human milk-fed white infants; 24 received 400 IU/day of vitamin D2, and 22 received placebo. An additional 12 patients were followed who received standard infant formula. 83% of patients completed a full 6 months of the study. Ultraviolet B light exposure and measurements of growth did not differ between groups. At 6 months, the human milk groups did not differ significantly in bone mineral content or serum concentrations of parathyroid hormone or 1,25-dihydroxyvitamin D, although total 25-hydroxyvitamin D values were significantly less in the unsupplemented human milk group (23.53 + or - 9.94 vs 36.96 + or - 11.86 ng/ml; p< 0.01). However, 25-hydroxyvitamin D3 serum concentrations were significantly higher in the unsupplemented human milk-fed group compared with the supplemented group (21.77 + or - 9.73 vs 11.74 + or - 10.27 ng/ml, p< 0.01) by 6 months of age. It was concluded that unsupplemented, human milk-fed infants had no evidence of vitamin D deficiency during the first 6 months of life.
PMID:2783734 Greer FR, Marshall S; J Pediatr 114 (2): 204-12 (1989)
A comparison was made of the ability of ergocalciferol and cholecalciferol to elevate plasma concentrations of vitamin D and 25-hydroxyvitamin D in cats. Cholecalciferol, given as an oral bolus in oil, resulted in a rapid elevation of plasma concentration of cholecalciferol followed by a rapid decline. In contrast, 25-hydroxyvitamin D concentration in plasma increased until day 3 after administration and remained elevated for a further 5 days. When 337 microg of both cholecalciferol and ergocalciferol in oil were given as an oral bolus to 10 cats, the peak plasma concentrations of cholecalciferol and ergocalciferol occurred at 8 or 12 h after administration. Peak concentrations of cholecalciferol were over twice those of ergocalciferol (570 +/- 80 vs. 264 +/- 42 nmol/l). The area under the curve 0-169 h for cholecalciferol was also more than twice that for ergocalciferol. When ergocalciferol and cholecalciferol were administered in a parenteral oil-based emulsion, higher concentrations of 25-hydroxyvitamin D3 than 25-hydroxyvitamin D2 were maintained in plasma. When both vitamins were included in the diet in the nutritional range, plasma concentrations of 25-hydroxyvitamin D2 were 0.68 of those of 25-hydroxyvitamin D3. Discrimination against ergocalciferol by cats appears to result from differences in affinity of the binding protein for the metabolites of the two forms of vitamin D. These results indicate that cats discriminate against ergocalciferol, and use it with an efficiency of 0.7 of that of cholecalciferol to maintain plasma 25-hydroxyvitamin D concentration.
PMID:15379909 Morris JG; J Anim Physiol Anim Nutr (Berl) 86 (7-8): 229-38 (2002)
Osteoporosis diminishes the quality of life in adults with cystic fibrosis (CF). Vitamin D deficiency resulting from malabsorption may be a factor in the etiology of low bone mineral density (BMD) in patients with CF. OBJECTIVE: Absorption of oral ergocalciferol (vitamin D2) and the consequent response of 25-hydroxyvitamin D in 10 adults with CF and exocrine pancreatic insufficiency was compared with that of 10 healthy control subjects. DESIGN: In this pharmacokinetic study, CF patients and control subjects were pair-matched on age, sex, and race. Each subject consumed 2500 microg oral vitamin D2 with a meal. The CF group also took pancreatic enzymes that provided > or = 80000 U lipase. Blood samples were obtained at baseline and at 5, 10, 24, 30, and 36 h after vitamin D2 consumption to measure serum vitamin D2 and 25-hydroxyvitamin D concentrations. RESULTS: Vitamin D2 concentrations in all subjects were near zero at baseline. CF patients absorbed less than one-half the amount of oral vitamin D2 that was absorbed by control subjects (P < 0.001). Absorption by the CF patients varied greatly; 2 patients absorbed virtually no vitamin D2. The rise in 25-hydroxyvitamin D in response to vitamin D2 absorption was significantly lower over time in the CF group than in the control group (P = 0.0012). CONCLUSIONS: Vitamin D2 absorption was significantly lower in CF patients than in control subjects. These results may help explain the etiology of vitamin D deficiency in CF patients, which may contribute to their low BMD.
PMID:11237938 Lark RK et al; Am J Clin Nutr 73 (3): 602-6 (2001)
Ergocalciferol is inactive and hence, the first step in the body is ruled by the conversion of this parent compound to 25-hydroxyvitamin D by the action of CYP2R1 followed by the generation of the major circulating metabolite, 1,25-dihydroxyvitamin D or calcitrol. The generation of this major metabolite is ruled by the activity of CYP27B1 which is a key 1-hydroxylase and CYP24A1 which is responsible for the 25-hydroxylation. As part of the minor metabolism, ergocalciferol is transformed into 25-hydroxyvitamin D in the liver by the activity of D-25-hydroxylase and CYP2R1. As well, the formation of 24(R),25dihydroxyvitamin D is performed mainly in the kidneys by the action of 25-(OH)D-1-hydroxylase and 25-(OH)D-24-hydroxylase. Additionally, there are reports indicating significant activity of 3-epimerase in the metabolism of ergocalciferol which modifies the hydroxy group in C3 from the alpha position to a beta. The epimers formed seemed to have a reduced affinity for the vitamin D plasma proteins and to the vitamin D receptor. An alternative activation metabolic pathway has been reported and this process is characterized by the activity of CYP11A1 and its hydroxylation in the C-20. This 20-hydroxylated vitamin D seems to have similar biological activity than calcitriol.
Vitamin D ... is hydroxylated at the 25 position in liver to produce 25-hydroxy-vitamin D3 which is the major metabolite circulating in the plasma. The metabolite is further hydroxylated in the kidney to 1,25-dihydroxy-vitamin D3, the most active metabolite in initiating intestinal transport of calcium & phosphate & mobilization of mineral from bone.
American Medical Association. AMA Drug Evaluations Annual 1991. Chicago, IL: American Medical Association, 1991., p. 1952
A polar, biologically active metabolite of vitamin D2, 25-hydroxyergocalciferol, which is about 1.5 times more active in curing rickets in rats, has been isolated from pig plasma.
O'Neil, M.J. (ed.). The Merck Index - An Encyclopedia of Chemicals, Drugs, and Biologicals. 13th Edition, Whitehouse Station, NJ: Merck and Co., Inc., 2001., p. 1786
Dihydrotachysterol is a vitamin D analog that may be regaurded as a reduction product of vitamin D2 ... Dihydrotachysterol is about 1/450 as active as vitamin D in the antirachitic assay, but at high doses it is much more effective than vitamin D in mobilizing bone mineral.
Hardman, J.G., L.E. Limbird, P.B., A.G. Gilman. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. New York, NY: McGraw-Hill, 2001., p. 1730
Vitamin D2 has known human metabolites that include Vitamin D2 3-glucuronide.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
Ergocalciferol can be found circulation for 1-2 days. This quick turnover is presented due to hepatic conversion and uptake by fat and muscle cells where it is transformed to the active form.
19 to 48 hours (however, stored in fat deposits in body for prolonged periods).
Thomson.Micromedex. Drug Information for the Health Care Professional. 24th ed. Volume 1. Plus Updates. Content Reviewed by the United States Pharmacopeial Convention, Inc. Greenwood Village, CO. 2004., p. 2850
For its activity, ergocalciferol is required to be transformed to its major active circulating hydroxylated metabolite and transported to the target organs in order to bind to its target, the vitamin D receptor. The activation of the vitamin D receptor is part of the vitamin D endocrine system and it is described by the production of a change in the transcription rates of the vitamin D receptor target genes. The target genes in the DNA affected by the presence of ergocalciferol are called vitamin D response elements which are dependent on co-modulators. The vitamin D receptor is a transcription factor and member of the steroid hormone nuclear receptor family. It presents a DNA binding domain (VDRE) that, when activated, recruits coregulatory complexes to regulate the genomic activity. Additionally, ergocalciferol presents nongenomic effects such as the stimulation of intestinal calcium transport via transcaltachia.
The mechanism of action of calcitriol, the activated form of vitamin D, resembles that of the steroid and thyroid hormones. Thus, calcitriol binds to cytosolic receptors within target cells, and the receptor-hormone complex interacts with the DNA of certain genes to either enhance or inhibit their transcription. Structural analysis of the calcitriol receptor indicates that it belongs to the same supergene family as the steroid receptors. Calcitriol also appears to exert a few effects that occur too rapidly to be explained by genomic actions. /Calcitriol/
Hardman, J.G., L.E. Limbird, P.B., A.G. Gilman. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. New York, NY: McGraw-Hill, 2001., p. 1728
The mechanisms responsible for mobilization of bone salts have been only partially defined, and the interaction of multiple factors appears to be involved. Paradoxically, the cells responsible for bone resorption (osteoclasts) are not directly acted upon by calcitriol and do not appear to contain calcitriol receptors. Instead, calcitriol causes an increase in the number of osteoclasts available to resorb bone; this may result from an action upon myeloid hematopoietic precursor cells that are induced to differentiate toward functional osteoclasts. The cells responsible for bone formation (osteoblasts) do contain receptors, and calcitriol causes them to elaborate several proteins, including osteocalcin, a vitamin K-dependent protein that contains gamma-carboxyglutamic acid residues. The exact role of this protein is not known, but other unidentified substances are also elaborated that appear to stimulate the function of osteoclasts. In addition, calcitriol acts synergistically with gamma-interferon to increase the production of interleukin-1, a lymphokine that promotes bone resorption.
Hardman, J.G., L.E. Limbird, P.B., A.G. Gilman. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. New York, NY: McGraw-Hill, 2001., p. 1728