1. 4-hydroxybutyric Acid
2. Gamma-hydroxybutyric Acid
1. 4-hydroxybutyric Acid
2. Gamma-hydroxybutyric Acid
3. Xyrem
4. Gamma-hydroxybutyrate
5. 591-81-1
6. Butanoic Acid, 4-hydroxy-
7. 4-hydroxy-butyric Acid
8. Oxybate
9. Sodium Oxybate
10. 4-hydroxybutanoate
11. Gamma Hydroxybutyric Acid
12. Oxybate Sodium
13. 4-hydroxy-butanoic Acid
14. Ghb
15. Oxy-n-butyric Acid
16. Butyric Acid, 4-hydroxy-
17. Somsanit
18. Gamma Hydroxybutyrate
19. 3-carboxypropoxy Acid
20. 4-hydroxyalkanoic Acid
21. 4-hydroxybutyrate Sodium
22. 4-hydroxycarboxylic Acid
23. .gamma.-hydroxybutyrate
24. Gamma Oh
25. Gam-oh
26. Chembl1342
27. 52352-27-9
28. Chebi:30830
29. 4-hydroxybutyric Acid Monosodium Salt
30. Sodium .gamma.-oxybutyrate
31. Gamma-hydroxybutyrate Sodium
32. Sodium Gamma-hydroxybutyrate
33. 30iw36w5b2
34. 4-ohb
35. Gamma-hydroxy Sodium Butyrate
36. Sodium .gamma.-hydroxybutyrate
37. 4 Hb
38. 4-hydroxybuttersaeure
39. Eb 27
40. .gamma.-oh
41. Wy 3478
42. Wy-3478
43. .gamma.-hydroxybutyric Acid Decomposition Product
44. Butyric Acid, 4-hydroxy-, Monosodium Salt
45. Butyric Acid, 4-hydroxy-, Sodium Salt
46. Gamma-hydroxybutanoic Acid
47. 4-hydroxyacid
48. .gamma.-hydroxybutyrate Sodium
49. .gamma.-hydroxy Sodium Butyrate
50. Hydroxybutyric Acid Monosodium Salt
51. Nsc84223
52. Gamma-hydroxy Butyrate
53. Polyhydroxybutyric Acid
54. Hydroxybutyricacid
55. .gamma.-hydroxybutyric Acid, Sodium Salt
56. Ncgc00247714-01
57. Shb
58. .gamma.-hydroxybutyric Acid Monosodium Salt
59. Brn 1720582
60. Alcover
61. Unii-30iw36w5b2
62. Hsdb 6927
63. Hydroxybutyric Acid-
64. Sodium Gamma-oxybutyrate
65. .gamma.-hydroxy Butyrate
66. 4-hydroxybutanoic Acid #
67. Schembl10786
68. 4-03-00-00774 (beilstein Handbook Reference)
69. Gtpl4711
70. Dea No. 2010
71. Aa3e2af0-ab7a-4a1e-a391-199c049d7162
72. Dtxsid2074740
73. .gamma.-hydroxybutyric Acid
74. Zinc1532805
75. Bdbm50023575
76. Lmfa01050006
77. Pdsp1_000342
78. Pdsp2_000340
79. .gamma.-hydroxybutyrate [mi]
80. Gamma-hydroxybutyrate [who-dd]
81. Db01440
82. Gamma-hydroxybutyric Acid [hsdb]
83. 35054-79-6
84. Sbi-0206686.p002
85. C00989
86. C01991
87. Q207920
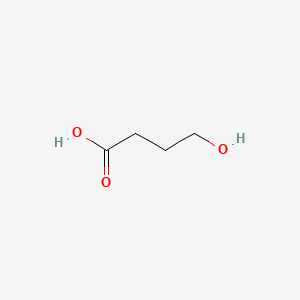
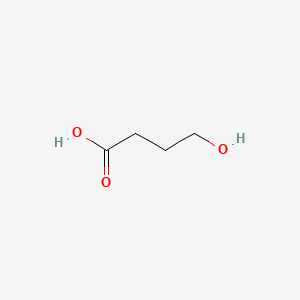
| Molecular Weight | 104.10 g/mol |
|---|---|
| Molecular Formula | C4H8O3 |
| XLogP3 | -0.6 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 3 |
| Rotatable Bond Count | 3 |
| Exact Mass | 104.047344113 g/mol |
| Monoisotopic Mass | 104.047344113 g/mol |
| Topological Polar Surface Area | 57.5 Ų |
| Heavy Atom Count | 7 |
| Formal Charge | 0 |
| Complexity | 60 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 1 | |
|---|---|
| Drug Name | XYREM |
| Active Ingredient | SODIUM OXYBATE |
| Company | JAZZ PHARMS (Application Number: N021196. Patents: 6780889, 7262219, 7668730, 7765106, 7765107, 7851506, 7895059, 8263650, 8324275, 8457988, 8589182, 8731963, 8772306, 8859619, 8952062, 9050302, 9486426, 9539330) |
Xyrem (sodium oxybate) oral solution is indicated for the treatment of excessive daytime sleepiness and cataplexy in patients with narcolepsy. /Sodium oxybate/
Thomson Health Care Inc.; Physicians' Desk Reference 62 ed., Montvale, NJ 2008, p. 1723
/Expl:/ To evaluate the efficacy and side-effect profile of off-label sodium oxybate (gamma hydroxy butyrate) therapy in severe childhood narcolepsy-cataplexy. DESIGN: Retrospective; chart review. SETTING: A multidisciplinary tertiary sleep center. PATIENTS: A group of eight children with severe narcolepsy-cataplexy diagnosed on the basis of clinical history, nocturnal polysomnography and the multiple sleep latency test were studied. A modified Epworth Sleepiness Scale and an arbitrary cataplexy severity scale (1 = minimal weakness, 2 = voluntarily preventable falls, 3 = falls to the ground) were utilized. INTERVENTIONS: Sodium oxybate therapy; concurrent medications were maintained. MEASUREMENTS AND RESULTS: Before sodium oxybate therapy, all subjects had suboptimally controlled sleepiness and cataplexy. Following treatment with sodium oxybate, 7/8 subjects (88%) improved. Cataplexy frequency decreased from a median of 38.5 to 4.5/ week (p = 0.0078). Cataplexy severity decreased from 2.75 to 1.75 (p = 0.06). The Epworth Sleepiness Scores improved from a median of 19 to 12.5 (p = 0.02). Suicidal ideation, dissociative episodes, tremor and constipation occurred in one subject each and terminal insomnia in two. Three of the 8 (38%) discontinued therapy. Two stopped the drug owing to side effects and one due to problems with postal delivery of the medication.
PMID:16944670 Murali H, Kotagal S; Sleep 29 (8): 1025-9 (2006)
Central nervous system depressant with abuse potential. Should not be used with alcohol or other CNS depressants. Sodium oxybate is GHB, a known drug of abuse. Abuse has been associated with some important central nervous system (CNS) adverse events (including death). Even at recommended doses, use has been associated with confusion, depression and other neuropsychiatric events. Reports of respiratory depression occurred in clinical trials. Almost all of the patients who received sodium oxybate during clinical trials were receiving CNS stimulants. Important CNS adverse events associated with abuse of GHB include seizure, respiratory depression and profound decreases in level of consciousness, with instances of coma and death. For events that occurred outside of clinical trials, in people taking GHB for recreational purposes, the circumstances surrounding the events are often unclear (e.g., dose of GHB taken, the nature and amount of alcohol or any concomitant drugs). /Sodium oxybate/
Thomson Health Care Inc.; Physicians' Desk Reference 62 ed., Montvale, NJ 2008, p. 1722
Because misuse and abuse of sodium oxybate (GHB) have been reported, patients with a history of drug abuse should be carefully evaluated and followed closely for signs of misuse or abuse (e.g., dosage escalation, drug-seeking behavior). Clinicians should document the diagnosis and indication for sodium oxybate therapy and be alert to drug-seeking behavior and/or feigned cataplexy. Commercially available sodium oxybate is subject to control as a schedule III drug. Nonmedical use of sodium oxybate is subject to control as a schedule I drug. /Sodium oxybate/
McEvoy, G.K. (ed.). American Hospital Formulary Service. AHFS Drug Information. American Society of Health-System Pharmacists, Bethesda, MD. 2007., p. 2625
Sodium oxybate is a CNS depressant with the potential to impair respiratory drive, especially in patients with preexisting respiratory impairment. Life-threatening respiratory depression has occurred following overdosage of the drug. Respiratory depression and an increase in obstructive sleep apnea have occurred in patients with narcolepsy receiving sodium oxybate in clinical trials. Most patients receiving sodium oxybate in clinical trials were receiving a CNS stimulant concomitantly; whether concomitant use of a CNS stimulant affected nocturnal respiration remains to be determined. Caution is advised if sodium oxybate is used in patients with respiratory impairment. Clinicians should be aware that a high incidence (50%) of sleep apnea has been reported in some cohorts of narcoleptic patients. /Sodium oxybate/
McEvoy, G.K. (ed.). American Hospital Formulary Service. AHFS Drug Information. American Society of Health-System Pharmacists, Bethesda, MD. 2007., p. 2625
Confused behavior at night, sometimes associated with wandering (sleepwalking), has occurred in patients receiving sodium oxybate in clinical trials. Since instances of substantial injury or potential injury (e.g., a fall, clothing set on fire while attempting to smoke, attempted ingestion of nail polish remover, sodium oxybate overdose) associated with sleepwalking occurred rarely during clinical trials of sodium oxybate, episodes of such activity in patients receiving the drug should be fully evaluated and appropriate interventions considered. /Sodium oxybate/
McEvoy, G.K. (ed.). American Hospital Formulary Service. AHFS Drug Information. American Society of Health-System Pharmacists, Bethesda, MD. 2007., p. 2625
For more Drug Warnings (Complete) data for 4-HYDROXYBUTANOIC ACID (21 total), please visit the HSDB record page.
Used as a general anesthetic, to treat conditions such as insomnia, clinical depression, narcolepsy, and alcoholism, and to improve athletic performance.
Treatment of narcolepsy with cataplexy in adult patients.
GHB predominantly works at two distinct binding sites in the central nervous system: it works as an agonist at the newly-characterized excitatory GHB receptor, while acting as a weak agonist at the inhibitory GABAB receptor. Since it is a naturally occurring substance, its physiological action is similar to that of some endogenous neurotransmitters in mammalian brain. GHB is probably synthesized from GABA in GABAergic neurons, and released when the neurons fire.
N07XX04
N - Nervous system
N01 - Anesthetics
N01A - Anesthetics, general
N01AX - Other general anesthetics
N01AX11 - Sodium oxybate
N - Nervous system
N07 - Other nervous system drugs
N07X - Other nervous system drugs
N07XX - Other nervous system drugs
N07XX04 - Sodium oxybate
Route of Elimination
Animal studies indicate that metabolism is the major elimination pathway for sodium oxybate, producing carbon dioxide and water via the tricarboxylic acid (Krebs) cycle and secondarily by beta-oxidation. Succinic acid enters the Krebs cycle where it is metabolized to carbon dioxide and water. Fecal and renal excretion is negligible. 5% renal elimination.
Volume of Distribution
190 to 384 mL/kg
Clearance
apparent oral cl=9.1 mL/min/kg [healthy adults receiving a single oral dose of 25 mg/kg]
4.5 mL/min/kg [cirrhotic patients without ascites receiving a single oral dose of 25 mg/kg]
4.1 mL/min/kg [cirrhotic patients with ascites receiving a single oral dose of 25 mg/kg]
Gamma-hydroxybutyric acid (GHB) ... absorption and disposition kinetics have been studied in 8 healthy male volunteers following oral administration of single doses of 12.5, 25 and 50 mg/kg The AUC increased disproportionately with the dose and so the apparent oral clearance decreased significantly as the dose was increased, whereas the terminal half-life and mean residence time increased. The peak plasma concentrations normalized to the lowest dose fell significantly with increasing doses, whilst the corresponding peak times increased. These findings suggest that both the oral absorption and the elimination of GHB are capacity-limited processes. GHB did not bind to significant extent to plasma proteins over the therapeutic concentration range. The pharmacokinetic parameters in healthy volunteers were not significantly different from those previously observed in alcohol-dependent patients with compensated alcoholic liver disease.
PMID:8299669 Palatini P et al; Eur J Clin Pharmacol 45 (4): 3353-6 (1993)
After ingestion, GHB is rapidly absorbed and quickly crosses the blood-brain barrier. It is not protein bound and is rapidly metabolized and excreted through the lungs. It has specific binding sites and selective brain distribution with the highest concentration in the basal ganglia.
Goldfrank, L.R. (ed). Goldfrank's Toxicologic Emergencies. 7th Edition McGraw-Hill New York, New York 2002., p. 940
Sodium oxybate is a hydrophilic compound that is rapidly but incompletely absorbed after oral administration with bioavailability approximately 25%. Administration of sodium oxybate immediately after a high fat meal results in delayed and decreased absorption. /Sodium oxybate/
Thomson/Micromedex. Drug Information for the Health Care Professional. Volume 1, Greenwood Village, CO. 2007., p. 2638
Monocarboxylate transporter 1 (MCT1) is an important determinant of the renal transport of the drug of abuse, gamma-hydroxybutyric acid (GHB). The objective of this study was to investigate the role of MCT2 and MCT4, present in tissues including intestine, kidney, skeletal muscle, and brain, in the membrane transport of GHB and the MCT substrate l-lactate. mRNA and protein of MCT2 and MCT4 were expressed in MDA-MB231 cells, as detected by reverse transcription-polymerase chain reaction and Western blot analysis; MCT1 and MCT3 were not detected. The uptake of GHB or l-lactate by MDA-MB231 cells was pH-dependent but not sodium-dependent. The concentration-dependent uptake of GHB was best fitted to a single-transporter model with a diffusional clearance component (K(m) of 17.6 +/- 1.5 mM, V(max) of 50.6 +/- 9.0 nmol x mg(-1) min(-1) and diffusional clearance of 0.20 +/- 0.07 microl x mg(-1) min(-1)). On the other hand, the concentration-dependent uptake of l-lactate was best fitted to a two-transporter model (K(m) of 21 +/- 2.5 and 3.0 +/- 1.5 mM, and V(max) of 268 +/- 72 and 62.9 +/- 42.2 nmol x mg(-1)min(-1), respectively). The uptake of GHB and l-lactate was inhibited by MCT inhibitors alpha-cyano-4-hydroxycinnamate (CHC), phloretin, and p-chloromercuribenzoic acid; CHC inhibited GHB and l-lactate uptake with IC(50) values of 1.71 +/- 0.39 and 0.71 +/- 0.11 mM, respectively. Small interfering RNA treatment to silence MCT2 or MCT4 significantly decreased their protein expression and the uptake of l-lactate and GHB; however, the decrease in GHB uptake with MCT2 inhibition was smaller than that for MCT4. This investigation demonstrated that GHB is a substrate for both MCT2 and MCT4; these transporters may be important in the nonlinear disposition of GHB, as well as influencing its tissue distribution.
PMID:17502341 Wang Q et al; Drug Metab Dispos 35 (8): 1393-9 (2007)
For more Absorption, Distribution and Excretion (Complete) data for 4-HYDROXYBUTANOIC ACID (7 total), please visit the HSDB record page.
gamma-Hydroxybutyrate (chemical formula HOOC-CH2-CH2- CH2OH) is a four-carbon molecule that is found naturally in the central nervous system and, in higher concentrations, in peripheral tissues. It has a structure much like gamma-aminobutyric acid (GABA), which is better understood than GHB and acts as an inhibitory neurotransmitter in vivo. gamma-Aminobutyric acid is catabolized by transamination to succinate semialdehyde, which is then oxidized to succinate. Brain tissue is capable of reducing succinate semialdehyde to GHB. Concentrations of both GHB and GHB-oxidizing enzymes are 15 to 20 times higher in kidney, heart, skeletal muscle, and brown fat than in the central nervous system.
PMID:1574880 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1003276 Chin MY et al; West J Med 156 (4): 380-4 (1992)
Animal studies indicate that metabolism is the major elimination pathway for sodium oxybate, producing carbon dioxide and water via the tricarboxylic acid (Krebs) cycle and secondarily by beta-oxidation. The primary pathway involves a cytosolic NADP+-linked enzyme, GHB dehydrogenase, that catalyses the conversion of sodium oxybate to succinic semialdehyde, which is then biotransformed to succinic acid by the enzyme succinic semialdehyde dehydrogenase. Succinic acid enters the Krebs cycle where it is metabolized to carbon dioxide and water. A second mitochondrial oxidoreductase enzyme, a transhydrogenase, also catalyzes the conversion to succinic semialdehyde in the presence of alpha-ketoglutarate. An alternate pathway of biotransformation involves beta-oxidation via 3,4-dihydroxybutyrate to carbon dioxide and water. No active metabolites have been identified. /Sodium oxybate/
Thomson Health Care Inc.; Physicians' Desk Reference 62 ed., Montvale, NJ 2008, p. 1722
30 to 60 minutes
Elimination: 0.5 to 1 hour. In a clinical study performed in 16 cirrhotic patients, the elimination half life was significantly longer (mean of 59 and 32 versus 22 minutes in healthy patients. /Sodium oxybate/
Thomson/Micromedex. Drug Information for the Health Care Professional. Volume 1, Greenwood Village, CO. 2007., p. 2638
GHB is present at much higher concentrations in the brain, where it activates GABA-B receptors to exert its sedative effects. With high affinity, GHB binds to excitatory GHB receptors that are densely expressed throughout the brain, including the cotex and hippocampus. There is some evidence in research that upon activation of GHB receptors in some brain areas, the excitatory neurotransmitter glutamate is released. GHB stimulates dopamin release at low concentrations by acting on the GHB receptor, and the release of dopamine occurs in a biphasic manner. At higher concentrations, GHB inhibits dopamine release by acting on the GABA-B receptors, which is followed by GHB receptor signaling and increased release of dopamine. This explains the paradoxical mix of sedative and stimulatory properties of GHB, as well as the so-called "rebound" effect, experienced by individuals using GHB as a sleeping agent, wherein they awake suddenly after several hours of GHB-induced deep sleep. It is proposed that overtime, the level of GHB in the brain decreases below the threshold for significant GABA-B receptor activation, leading to preferential activation of GHB receptor over GABA-B receptors and enhanced wakefulness.
Oxybate (GHB) is a metabolite of gamma-aminobutyric acid (GABA) which is synthesised and accumulated by neurones in the brain. It is present at uM concentrations in all brain regions investigated as well as in several peripheral organs, particularly in the gastro-intestinal system. Neuronal depolarization releases GHB into the extracellular space in a Ca2+-dependent manner. A family of GHB receptors in rat brain have been identified and cloned and most probably belong to the G-protein-coupled receptors. High-affinity receptors for GHB are present only in neurones, with a restricted specific distribution in the hippocampus, cortex and dopaminergic structures of rat brain. In general, stimulation of these receptors with low (physiological) amounts of GHB induces hyperpolarization in dopaminergic structures with a reduction of dopamine release. However, in the hippocampus and frontal cortex, GHB seems to induce depolarization with an accumulation of cGMP and an increase in inositol phosphate turnover. However, at higher (therapeutic) exposures, GHB receptors are saturated and probably de-sensitized and down-regulated. Such GHBergic potentiations induce dopaminergic hyperactivity, strong sedation with anaesthesia and EEG changes that are consistent with normal sleep and/or epileptic spikes.
European Medicines Agency (EMEA), Committee for Medicinal Products for Human Use; European Public Assessment Report (EPAR) (Scientific Discussion); Xyrem, p.2 (2007). Available from, as of March 19,2008: https://www.emea.europa.eu/humandocs/PDFs/EPAR/xyrem/324056en6.pdf
Gamma-hydroxybutyrate (GHB), a four-carbon fatty acid and anesthetic, is widely considered to be a relatively specific inhibitor of central dopamine (DA) release. The inhibitory effect of GHB on the latter is thought to occur as a consequence of its diminution of impulse flow in central dopaminergic neurons. However, a number of studies have recently reported that GHB primarily stimulates rather than inhibits central DA release, with any inhibitory effect produced of a modest and transitory nature. GHB has been and continues to be widely used as an important research tool largely because it is one of only a few drugs available that acts primarily on DA release. Consequently, it is important to determine whether GHB inhibits DA release as previously thought, or stimulates DA release, as more recently suggested. Following a critical review of the literature, the present report suggests that GHB does inhibit rather than stimulate presynaptic DA release in consonance with its behavioral and pharmacological activity. Recent in vivo studies indicating that GHB stimulates DA release were done under anesthesia or in the presence of a high concentration of calcium. Both conditions have been found to spuriously enhance striatal DA release in vivo, which may account for the failure of some studies to observe an inhibitory effect of GHB on DA release in vivo.
PMID:9003964 Feigenbaum JJ, Howard SG; Int J Neurosci 88 (1-2): 53-69 (1996)
Sodium oxybate is an endogenous 4-carbon fatty acid that is thought to act as a neurotransmitter in the regulation of sleep cycles, blood flow, emotion, and memory. Its actions are thought to be mediated through brain receptors specific for GHB as well as through binding to GABA-B receptors. At low doses, the drug inhibits presynaptic dopamine release, while at high doses, dopamine release may be stimulated. It is believed that sodium oxybate decreases the symptoms of narcolepsy by inducing REM sleep and increasing delta sleep. The precise mechanism by which sodium oxybate produces anticataplectic activity in patients with narcolepsy is unknown. /Sodium oxybate/
European Medicines Agency (EMEA), Committee for Medicinal Products for Human Use; European Public Assessment Report (EPAR) (Scientific Discussion); Xyrem, p.13 (2007). Available from, as of March 19,2008: https://www.emea.europa.eu/humandocs/PDFs/EPAR/xyrem/324056en6.pdf
BUILDING BLOCK



LOOKING FOR A SUPPLIER?